Abstract
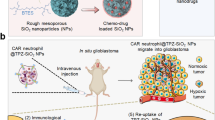
Pharmaceuticals have been developed for the treatment of a wide range of bone diseases and disorders, but suffer from problematic delivery to the bone marrow. Neutrophils are naturally trafficked to the bone marrow and can cross the bone marrow–blood barrier. Here we report the use of neutrophils for the targeted delivery of free drugs and drug nanoparticles to the bone marrow. We demonstrate how drug-loaded poly(lactic-co-glycolic acid) nanoparticles are taken up by neutrophils and are then transported across the bone marrow–blood barrier to boost drug concentrations in the bone marrow. We demonstrate application of this principle to two models. In a bone metastasis cancer model, neutrophil delivery is shown to deliver cabazitaxel and significantly inhibit tumour growth. In an induced osteoporosis model, neutrophil delivery of teriparatide is shown to significantly increase bone mineral density and alleviate osteoporosis indicators.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
Data supporting the findings of this study are available within the Article and its Supplementary Information. All relevant data can be made available upon reasonable request to the corresponding authors. Source data are provided with this paper.
References
Rodan Gideon, A. & Martin, T. J. Therapeutic approaches to bone diseases. Science 289, 1508–1514 (2000).
Chaudhari, K. R. et al. Bone metastasis targeting: a novel approach to reach bone using Zoledronate anchored PLGA nanoparticle as carrier system loaded with Docetaxel. J. Control. Release 158, 470–478 (2012).
Tavassoli, M. The marrow–blood barrier. Br. J. Haematol. 41, 297–302 (1979).
Adjei, I. M., Sharma, B., Peetla, C. & Labhasetwar, V. Inhibition of bone loss with surface-modulated, drug-loaded nanoparticles in an intraosseous model of prostate cancer. J. Control. Release 232, 83–92 (2016).
Sun, W. et al. Bone-targeted nanoplatform combining zoledronate and photothermal therapy to treat breast cancer bone metastasis. ACS Nano 13, 7556–7567 (2019).
Chen, Q. et al. Bone targeted delivery of SDF-1 via alendronate functionalized nanoparticles in guiding stem cell migration. ACS Appl. Mater. Interfaces 10, 23700–23710 (2018).
Mann, A. P. et al. E-selectin-targeted porous silicon particle for nanoparticle delivery to the bone marrow. Adv. Mater. 23, H278–H282 (2011).
Wang, H. et al. Tetracycline-grafted PLGA nanoparticles as bone-targeting drug delivery system. Int. J. Nanomed. 10, 5671–5685 (2015).
Aoki, K., Alles, N., Soysa, N. & Ohya, K. Peptide-based delivery to bone. Adv. Drug Deliv. Rev. 64, 1220–1238 (2012).
Lavrador, P., Gaspar, V. M. & Mano, J. F. Stimuli-responsive nanocarriers for delivery of bone therapeutics – barriers and progresses. J. Control. Release 273, 51–67 (2018).
Lahoz-Beneytez, J. et al. Human neutrophil kinetics: modeling of stable isotope labeling data supports short blood neutrophil half-lives. Blood 127, 3431–3438 (2016).
Theilgaard-Mönch, K. et al. The transcriptional program of terminal granulocytic differentiation. Blood 105, 1785–1796 (2005).
Martin, C. et al. Chemokines acting via CXCR2 and CXCR4 control the release of neutrophils from the bone marrow and their return following senescence. Immunity 19, 583–593 (2003).
Cacalano, G. et al. Neutrophil and B cell expansion in mice that lack the murine IL-8 receptor homolog. Science 265, 682–684 (1994).
Eash, K. J., Greenbaum, A. M., Gopalan, P. K. & Link, D. C. CXCR2 and CXCR4 antagonistically regulate neutrophil trafficking from murine bone marrow. J. Clin. Invest. 120, 2423–2431 (2010).
Lawrence, S. M., Corriden, R. & Nizet, V. How neutrophils meet their end. Trends Immunol. 41, 531–544 (2020).
Borregaard, N. Neutrophils, from marrow to microbes. Immunity 33, 657–670 (2010).
Wang, J. et al. Visualizing the function and fate of neutrophils in sterile injury and repair. Science 358, 111–116 (2017).
Garner, H. & de Visser, K. E. Neutrophils take a round-trip. Science 358, 42–43 (2017).
Furze, R. C. & Rankin, S. M. Neutrophil mobilization and clearance in the bone marrow. Immunology 125, 281–288 (2008).
Suratt, B. T. et al. Neutrophil maturation and activation determine anatomic site of clearance from circulation. Am. J. Physiol. Lung Cell. Mol. Physiol. 281, L913–L921 (2001).
Løvås, K., Knudsen, E., Iversen, P. O. & Benestad, H. B. Sequestration patterns of transfused rat neutrophilic granulocytes under normal and inflammatory conditions. Eur. J. Haematol. 56, 221–229 (1996).
Hofman, M. S. et al. 177Lu-PSMA-617 versus cabazitaxel in patients with metastatic castration-resistant prostate cancer (TheraP): a randomised, open-label, phase 2 trial. Lancet 397, 797–804 (2021).
Wang, J. et al. ROS-responsive nanocomplex of aPD-L1 and cabazitaxel improves intratumor delivery and potentiates radiation-mediated antitumor immunity. Nano Lett. 22, 8312–8320 (2022).
Blick, S. K. A., Dhillon, S. & Keam, S. J. Teriparatide. Drugs 68, 2709–2737 (2008).
Xue, J. et al. Neutrophil-mediated anticancer drug delivery for suppression of postoperative malignant glioma recurrence. Nat. Nanotechnol. 12, 692–700 (2017).
Schwartz, R. S. & Erban, J. K. Timing of metastasis in breast cancer. N. Engl. J. Med. 376, 2486–2488 (2017).
Cai, W.-L. et al. microRNA-124 inhibits bone metastasis of breast cancer by repressing Interleukin-11. Mol. Cancer 17, 9 (2018).
Taguchi, T. SY7-2 - treatment strategy of bone metastasis in breast cancer. Ann. Oncol. 28, ix33 (2017).
Parveen, S. et al. Therapeutic targeting with DABIL-4 depletes myeloid suppressor cells in 4T1 triple-negative breast cancer model. Mol. Oncol. 15, 1330–1344 (2021).
Balog, J. et al. Single cell mass cytometry revealed the immunomodulatory effect of cisplatin via downregulation of splenic CD44+, IL-17A+ MDSCs and promotion of circulating IFN-γ myeloid cells in the 4T1 metastatic breast cancer model. Int. J. Mol. Sci. 21, 170 (2019).
DuPre, S. A. & Hunter, K. W. Jr Murine mammary carcinoma 4T1 induces a leukemoid reaction with splenomegaly: association with tumor-derived growth factors. Exp. Mol. Pathol. 82, 12–24 (2007).
Yun, H. M. et al. 2,4,5-Trimethoxyldalbergiquinol promotes osteoblastic differentiation and mineralization via the BMP and Wnt/β-catenin pathway. Cell Death Dis. 6, e1819 (2015).
Al Rifai, O. et al. Proprotein convertase furin regulates osteocalcin and bone endocrine function. J. Clin. Invest. 127, 4104–4117 (2017).
Yeom, J., Ma, S. & Lim, Y.-H. Probiotic Propionibacterium freudenreichii MJ2 enhances osteoblast differentiation and mineralization by increasing the OPG/RANKL ratio. Microorganisms 9, 673 (2021).
An, J. M. et al. Oral delivery of parathyroid hormone using a triple-padlock nanocarrier for osteoporosis via an enterohepatic circulation pathway. ACS Appl. Mater. Interfaces 13, 23314–23327 (2021).
Bain, B. J. & England, J. M. Normal haematological values: sex difference in neutrophil count. Br. Med. J. 1, 306–309 (1975).
Wright, L. E. et al. Murine models of breast cancer bone metastasis. Bonekey Rep. 5, 804–804 (2016).
Acknowledgements
This work was supported by the National Natural Science Foundation of China (81973246 (J.Y.) and 82003667 (L.L.)). We thank J. Wang from the Core Facilities, Zhejiang University School of Medicine, X. Zhang from the Analysis Center of Agrobiology and Environmental Sciences and Institute of Agrobiology and Environmental Sciences, Zhejiang University, and G. Wang from the radiology department, the First Affiliated Hospital, Zhejiang University School of Medicine for technical support. We thank Servier Medical Art for support with figure drawing.
Author information
Authors and Affiliations
Contributions
Z.L., L.L. and J.Y. designed the experiments, analysed the data and wrote the paper. Z.L. performed most of the experiments. Y.Lu., X.S., X.G. and Y.Liu assisted with animal experiments. Y.S., X.Li. and B.Q. assisted with cellular experiments. J.Z. and X.Liu. helped with data analysis. M.J., J.H. and S.W. revised the manuscript. Q.L., J.Y. and L.L. supervised the project.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Nanotechnology thanks Michael Mitchell and Sara Rankin for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–14.
Supplementary Video 1
PET/CT video of Free FDG at 2 h.
Supplementary Video 2
PET/CT video of Free FDG at 6 h.
Supplementary Video 3
PET/CT video of NEs (age: 6 h) at 2 h.
Supplementary Video 4
PET/CT video of NEs (age: 6 h) at 6 h.
Supplementary Video 5
PET/CT video of NEs (age: 24 h) at 2 h.
Supplementary Video 6
PET/CT video of NEs (age: 24 h) at 6 h.
Source data
Source Data Fig. 2
Main Fig. 2 statistical source data.
Source Data Fig. 3
Main Fig. 3 statistical source data.
Source Data Fig. 4
Main Fig. 4 statistical source data.
Source Data Fig. 5
Main Fig. 5 statistical source data.
Source Data Fig. 6
Main Fig. 6 statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luo, Z., Lu, Y., Shi, Y. et al. Neutrophil hitchhiking for drug delivery to the bone marrow. Nat. Nanotechnol. 18, 647–656 (2023). https://doi.org/10.1038/s41565-023-01374-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41565-023-01374-7
This article is cited by
-
Enhancing aortic valve drug delivery with PAR2-targeting magnetic nano-cargoes for calcification alleviation
Nature Communications (2024)
-
Rerouting nanoparticles to bone marrow via neutrophil hitchhiking
Nature Nanotechnology (2023)