Abstract
Epidemiological knowledge of circulating carbapenem-resistant Klebsiella pneumoniae (CRKP) is needed to develop effective strategies against this public health threat. Here we present a longitudinal analysis of 1,017 CRKP isolates recovered from patients from 40 hospitals across China between 2016 and 2020. Virulence gene and capsule typing revealed expansion of CRKP capsule type KL64 (59.5%) alongside decreases in KL47 prevalence. Hypervirulent CRKP increased in prevalence from 28.2% in 2016 to 45.7% in 2020. Phylogenetic and spatiotemporal analysis revealed Beijing and Shanghai as transmission hubs accounting for differential geographical prevalence of KL47 and KL64 strains across China. Moderate frequency capsule or O-antigen loss was also detected among isolates. Non-capsular CRKP were more susceptible to phagocytosis, attenuated during mouse infections, but showed increased serum resistance and biofilm formation. These findings give insight into CRKP serotype prevalence and dynamics, revealing the importance of monitoring serotype shifts for the future development of immunological strategies against CRKP infections.
Similar content being viewed by others
Main
Carbapenem-resistant Klebsiella pneumoniae (CRKP) has emerged as a major public health threat1 due to its multidrug-resistant nature and ability to cause infections with high mortality rates2. According to the 2023 China Antimicrobial Surveillance Network (CHINET), K. pneumoniae has become the second most commonly isolated bacterium in clinics in China, and the resistance rate to meropenem has steadily increased from 2.9% in 2005 to 30.0% in 2023 (http://www.chinets.com/Data/GermYear). This increase in resistance prevalence has, in turn, limited therapeutic options and increased the demand for novel strategies to control CRKP infection.
Vaccines targeting surface polysaccharide antigens, such as the capsular polysaccharide (CPS, K antigen) or lipopolysaccharide (LPS, O antigen), have been proposed as a promising alternative to antimicrobials for combating multidrug-resistant pathogens3,4. Vaccines and monoclonal antibodies have shown protection against K. pneumoniae in experimental animal models5,6,7,8 but have not yet progressed beyond clinical trials for human use9. Furthermore, K. pneumoniae contains at least 79 capsular types (K types) that differ both genetically and phenotypically3,10, posing a major challenge to achieving broad vaccine coverage. Consequently, there is a need for up-to-date epidemiological insight into the most prevalent and clinically relevant serotypes (type of surface antigens of the organism, such as K or O antigens) to effectively inform and guide vaccine development strategies.
The prevalence of K. pneumoniae varies between countries and hosts. In recent years, several studies have reported on the prevalence of K. pneumoniae infection in different countries, including the distribution and prevalence of drug resistance, virulence and capsular genotypes11,12,13. However, little is known about its sero-epidemiology in China, mainly due to the limited availability of commercial antibodies for serological typing and the inability of genetic typing to detect phenotypic variation resulting from genetic mutations or disruptions in polysaccharide synthesis-related genes14,15,16,17. The widespread occurrence and expansion of CRKP-associated infection across China necessitates a systematic analysis of the population structure, resistance mechanisms and virulence evolution of strains isolated from different areas.
In this Article, we conducted a nationwide, longitudinal, retrospective, epidemiological investigation of CRKP in China. We provided comprehensive data on the distribution and longitudinal evolution of K types, antimicrobial resistance (AMR) and virulence factors profiles among CRKP strains in the country. In particular, we identified a substantial proportion of capsular- or O-antigen-deficient strains in various infection samples and experimentally investigated the potential bases for the acquired survival advantage of these capsular-deficient strains. These findings on serotype prevalence provide initial insight in the development of effective strategies to control CRKP infection.
Results
CRKP isolate capsule and antimicrobial profiling
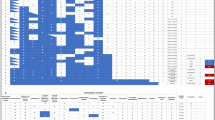
During 2016–2020, a total of 1,017 non-duplicate CRKP isolates were collected from K. pneumoniae-infected adult patients admitted to 40 hospitals located in 26 provinces or municipalities in China (Extended Data Fig. 1 and Supplementary Table 1). Antimicrobial susceptibility testing results are summarized in Supplementary Note and Supplementary Table 2. Carbapenemase genes were detected by PCR in 98.2% (999/1,017) of the CRKP isolates, the vast majority of which were blaKPC-2 (89.4%, 909/1,017), followed by blaNDM (4.8%, 49/1,017) and blaOXA-48-like (1.8%, 18/1,017) (Supplementary Table 3). We identified 18 (1.8%) non-carbapenemase-producing CRKP isolates, of which 15 (83.3%) had both the porin (Ompk35/Ompk36) mutation and extended-spectrum β-lactamase genes (Supplementary Table 3).
Capsular genotyping revealed 58 different K loci; the majority belonged to K types KL64 (50.4%) and KL47 (25.9%) (Supplementary Table 4). The frequencies of these two K types varied with time and geography. We observed a significant increase in KL64 from 35.0% in 2016 to 59.6% in 2020, accompanied by a decrease in KL47 from 42.3% to 17.8% (Fig. 1a; P value for trend = 5.2 × 10−5, 2.1 × 10−9, respectively). Furthermore, KL64 accounted for the majority of the isolates from eastern and central China, including Shanghai, Zhejiang and Sichuan, whereas isolates from northern and northeastern China, that is, Beijing, Liaoning and Tianjin, were predominantly KL47 (Fig. 1b). Other K types were less common (1–54 isolates; Supplementary Table 4) and may be endemic regionally. For example, KL19 accounted for 13.4% of isolates from Shanghai, Zhejiang and Jiangxi in eastern China, while KL10 accounted for 18.1% of isolates from Liaoning and Heilongjiang in northeastern China (Fig. 1b).
a, Percentage of K types between different years. The five most common K types (KL64, KL47, KL19, KL25 and KL10) and other K types are shown. b, Map of CRKP clinical isolates collected from 26 provinces or municipalities in China. The included areas are overlaid with blue flags if there were <10 CRKP isolates, otherwise with pie charts of the K-type percentages. The size of these pie charts is proportional to the number of CRKP isolates. Histograms around the map show the proportions of annual K types in certain areas, as indicated by the arrows. The grey bar indicates that the number of CRKP strains in that year was less than 3. c, Five common carbapenem resistance genes (blaIMP, blaNDM, blaVIM, blaKPC and blaOXA-48-like) were identified in 1,017 CRKP isolates. The number of CRKP isolates in each K type, n, is given above. The resistance rates to imipenem, tigecycline, polymyxin B, CZA and amikacin in different K-type strains are shown as a heat map below (see Supplementary Table 2 for details).
We also showed the differences in phenotype of antimicrobial susceptibility and distribution of carbapenemase genes by sequencing-based PCR between K types. The top seven K types were predominantly associated with blaKPC-2, which was susceptible to ceftazidime–avibactam (CZA) and resistant to amikacin (except KL19) (Fig. 1c), while 56.5% of the isolates in KL51 and KL60 carried blaOXA-48-like. Notably, more than a third of the KL51, KL15 and other rare K-type isolates carried blaNDM and showed resistance to CZA (Fig. 1c).
Virulence-associated gene carriage in CRKP isolates
We screened for the presence of five hypervirulence-associated genes (rmpA, rmpA2, iroB, iucA and peg344) by PCR in all CRKP isolates13,18,19 and classified 413 (40.6%) isolates carrying both iucA and rmpA/rmpA2 genes as hypervirulent CRKPs (hv-CRKPs)20, including 31 isolates with all five hypervirulence-associated genes. The majority of hv-CRKPs were from K types KL64 (312/413, 75.5%) and KL47 (67/413, 16.2%). Notably, among the top ten K-type strains, KL60 contained the highest proportion of hv-CRKP strains (7/11, 63.6%), followed by KL64 (312/513, 60.8%), KL62 (5/12, 41.7%) and KL47 (67/263, 25.5%) (Fig. 2a).
a, The proportion of hv-CRKP in different K-type CRKP isolates in China during 2016–2020. The grey bars indicate strains with iucA and rmpA/rmpA2 genes, and the black bars indicate strains with all five virulence genes (rmpA, rmpA2, iroB, iucA and peg344). The number of CRKP strains of K type, n, is given below. b, Trends in the proportion of hv-CRKP in all CRKPs and those from KL64 and KL47. Annual and total hv-CRKP rates in KL64 and KL47 strains in different regions are shown below. Grey blocks indicate years with less than three KL64 or KL47 strains. c, Circular alignment of virulent plasmids pST11-Vir-2 (CP039526) and pST11-Vir-3 (CP048945) referring to pST11-Vir-1-KPC (AY378100) via BRIG. Representative genes are labelled in the outermost circle, with the hypervirulence-associated genes in red.
The proportion of hv-CRKP increased over the five years, from 28.2% in 2016 to 45.7% in 2020 (P value for trend = 0.0061), which could be attributed to both the population expansion of KL64 and a threefold increase in hv-CRKP levels in KL47, from 10.1% in 2016 to 40.5% in 2020 (P value for trend = 1.1 × 10−4). By contrast, the frequency of hv-CRKP in KL64 remained stable over the period 2016–2020 (P value for trend = 0.61) (Fig. 2b). High levels of hv-CRKP in KL64 were found in Henan (88.2%), Zhejiang (87.8%), Beijing (81.8%) and Jiangsu (80.7%), while most KL47 strains in Shanghai (81.3%) and Liaoning (69.0%) were hv-CRKP. Conversely, low hv-CRKP frequencies were found in both KL64 (28.2%, 21.2%) and KL47 (0%, 0%) isolates from Hubei and Sichuan throughout the study period. Notably, the prevalence of KL47 hv-CRKPs increased significantly in Liaoning (2016–2019, P value for trend = 0.019) and Beijing (2016–2020, P value for trend = 0.037) (Fig. 2b).
The varying levels of hv-CRKP in KL64 and KL47 strains were partially explained by their associated virulence plasmids (Fig. 2c). Details of the levels of hv-CRKP in KL64 and KL47 strains with associated virulence plasmids are described in Supplementary note.
Genomic epidemiology of KL47 and KL64 CRKP in China
To obtain a phylogenetic overview of the two most common K-type CRKPs, we performed whole-genome sequencing on 207 KL47 and 319 KL64 isolates and found that >99% (523/526) of them belonged to sequence type ST11 (Supplementary Tables 5 and 6). These 523 ST11 isolates were integrated with additional 3,047 public ST11 genomes to form a global genomic collection of 3,570 isolates. After filtering recombination regions, a maximum likelihood phylogeny of the ST11 lineage was estimated based on the remaining non-repetitive, non-recombinant single-nucleotide polymorphisms in the core genome. We manually separated the tree into four major lineages, of which L2 and L3 were broadly consistent with clonal groups identified based on the cgLIN codes14 and L1 is a subclade of the L2 lineage that consisted of almost exclusively Chinese isolates (99.1%, 2,111/2,130). Based on kleborate predictions, we found a strong correlation between the 44 K types and 6 O types in ST11, with KL64:O2 and KL47:OL101 accounting for 61% (2,187/3,570) of the strains, especially those in L1. The most common carbapenemase in ST11 was blaKPC-2, followed by blaOXA-48 and blaNDM-1 (Fig. 3a).
a, The population structure of ST11 strains. The metadata is shown on the right-hand side. The grey boxes show the four lineages identified along the tree. CARB, carbapenemase; CGs, clonal groups predicted by cgLIN codes. b, The maximum likelihood tree of lineage L1 with branches recalibrated by BactDating. Dates next to particular branches indicate their estimated date of origin with the 95%CI in brackets. Branches are colour-coded according to their estimated regional origin with root nodes of KL47 and KL64 clades shown nearby. Additional geographic estimates of the nodes have been calculated using three models implemented in the APE package in R and visualized in Extended Data Fig. 3. The major regional transmissions (≥8 isolates in the target region) in each of the KL47 (8 events; blue) and KL64 (12 events; orange) clades are shown as grey arcs with serial numbers on the outside. The outer rings show regions, O types and K types, carbapenemase-carrying plasmids, virulence plasmids and each of the five hypervirulence genes from inside to outside, each colour-coded according to the key. The star in the KL64 clade shows a cluster of hv-CRKP isolates, with their times of origin and 95%CI nearby. There were 19 clusters of 14 rare serotypes as predicted by kleborate in lineage L1, which were labelled accordingly. c, National distributions of the ST11 L1 strains. Each region is colour-coded according to the percentage of KL64, and the arrows indicate regions that received ≥5 inter-regional transmissions from Shanghai (red) or Beijing (blue), with the thickness proportional to the number of transmissions. Distinct patterns were found between Shanghai and Beijing transmissions. Shanghai strains were mainly transmitted to the eastern and central regions, whereas Beijing strains were transmitted to the northern and northeastern regions, in line with the patterns of inter-regional health seeking in China. d, The number of observed transmissions originated from each region extracted from the L1 tree in b. The two predominant sources (Shanghai and Beijing) are highlighted in red.
Spatiotemporal transmission of L1 CRKP within China
Most of the strains in lineage L1 were from China (2,111 strains), followed by the USA (7), Oman (3), Singapore (3), and four other countries. Temporal signals were found in lineage L1 based on regression of root-to-tip genetic distance against sampling time (R2 = 0.18, P = 8.2 × 10−12) and further demonstrated based on two date randomization tests (Extended Data Fig. 2a–c and Methods). Therefore, based on the phylogeny above, we estimated the spatiotemporal dynamics of lineage L1 using BactDating and inferred the fluctuation of its effective population sizes using skygrowth in R. The ancestral inter-regional transmissions and serovar changes were also inferred using both TreeTime and the Analyses of Phylogenetics and Evolution (APE) package in R. The most recent common ancestor of L1 was estimated to be present before 1983 (95% confidence interval (95%CI) 1979–1987) in serotype KL47:OL101, whereas the KL64:O2 serotype was estimated to emerge in 2003 (95%CI 2002–2004) as a subclade of L1 and experienced rapid national dissemination in the past decade. Notably, we also predicted 14 other K genotypes in L1, some of which formed local clusters, that is, KL25 in Sichuan and KL110 in Jiangsu (Fig. 3b and Supplementary Table 7).
The KL47 strains were estimated to originate in either Zhejiang or Beijing by different models, although all agreed on its long-term persistence in Zhejiang since 1990 (95%CI 1986–1993) (Fig. 3b and Extended Data Fig. 3). By contrast, the KL64 clade was estimated to originate in Zhejiang by all models. We predicted a total of 308 cross-regional transmissions along the phylogeny, which were branches that connect nodes with different geographic inferences by TreeTime. We found that 53.6% (165) of these transmissions had parental nodes in either Beijing or Shanghai, the two major sources of transmissions (Fig. 3c). Among them, Beijing was estimated to contribute 75 transmissions, mostly to northern and northeastern regions, and Shanghai was estimated to contribute 90 transmissions, mainly to eastern and central regions (Fig. 3d).
Furthermore, the majority of the transmissions leave only one or a few isolates in the target regions. We, therefore, focused on 20 major events that were evidenced by ≥8 isolates in the target regions (Fig. 3b). Many of the major transmissions in the KL47 strains involve Beijing and its neighbouring, northern regions such as Henan (event KL47.2), Liaoning (event KL47.2) and Tianjin (events KL47.2 and KL47.7), contributing to the predominance of KL47 clade in northern China (blue route; Fig. 3c). Conversely, KL64 strains were estimated to experience nine major transmissions from Shanghai to central and eastern China including Jiangsu (event KL64.1), Hubei (event KL64.2), Sichuan (event KL64.5) and other regions (red route, Fig. 3c), resulting in their increasing KL64 frequencies.
Non-capsulated CRKP exist among KL64 and KL47 isolates
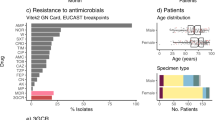
All isolates identified as KL64 or KL47 by genotyping were subjected to serologic typing, and 7.4% (38/513) KL64 and 12.2% (32/263) KL47 isolates, respectively, did not react with the corresponding antisera in the Quellung reaction (Extended Data Fig. 4 and Supplementary Table 8). These isolates appeared translucent, showed a significant reduction in polysaccharide capsule uronic acid (Fig. 4a) and were confirmed as NEKp (non-capsulated K. pneumoniae) strains by electron microscopy (Fig. 4b). The frequency of NEKp did not change significantly over the study period (Supplementary Table 9; P value for trend = 0.97 and 0.99) nor between samples from different body sites (Fig. 4c; P = 0.47).
a, CPS of NEKp and selected paired EKp strains measured by uronic acid assay. Paired EKp strains were randomly selected from regions and samples similar to those of NEKp. Parental EKp strains and their isogenic Δcps mutants are indicated by arrows. The 20–445Δcps and 18–81Δcps mutants had a significantly lower amount of polysaccharide capsule uronic acid compared to WT strains. The number of EKp and NEKp strains of K type KL64 or KL47, n, is given below. Data are shown as the mean ± s.e.m. Each point represents the mean value of three biological replicates of one strain. For clarity, individual error bars for each strain are not shown. Unpaired two-sided Welch’s t-test was performed for statistical analysis. b, Transmission electron microscopy images of representative EKp (KL64 strain 19–241 and KL47 strain 18–729) and NEKp (KL64 strain 19–242 and KL47 strain 18–737) strains. Each electron micrograph shows the representative result of three repetitions. c, Frequency of NEKp strains isolated from different sites of infection. The number of CRKP strains in different infection sites is shown below. Pearson’s chi-squared test was used to analyse the proportion difference of NEKp strains in different infection samples. d, cps-locus and rfaH gene variants in NEKp isolates. Mutations found in the capsule biosynthesis genes in KL64 and KL47 NEKp isolates. The black flag indicates the location of the mutation. Red, black and blue lines indicate ISs, single-nucleotide polymorphisms and deletions, respectively. n, the total number of mutations observed in this gene. e, Metagenomic analysis of cps-locus variants in unprocessed clinical samples (for details, see Supplementary Table 10). NS, not significant.
Various mutations, including insertion sequences (ISs), point mutations and deletions, were found in the cps region or the rfaH gene of NEKp strains, mainly affecting the initial glycosyltransferase genes (wbaP for KL47 and wcaJ for KL64) (Fig. 4d and Supplementary Table 8). Capsule-deficient phenotypes were replicated in the mutant strains 18–81-KL47ΔwbaP and 20–445-KL64ΔwcaJ, and their capsule production could be restored upon complementation (Fig. 4a and Extended Data Fig. 4). Complementation with wcaJ/wbaP also restored capsule production in clinical NEKp strains with corresponding gene disruptions, further supporting the link between wcaJ/wbaP disruptions and the capsule-deficient phenotype (Extended Data Fig. 4).
To investigate whether such capsule deficiency occurs during in vitro culture in the laboratory, we cultured ten random strains for each of KL47 and KL64 in blood agar plate for 48 h and found very low levels (<0.56%) of capsule-deficient mutants (Extended Data Fig. 5). In addition, we metagenomically sequenced 49 unprocessed clinical samples with CRKP infections. Among the 11 samples with >5-fold coverage, three had disrupted cps genes, including nonsense mutations or ISKpn26 insertions in wcaJ, and other disruptions, demonstrating the presence of capsule-deficient mutations in vivo (Fig. 4e and Supplementary Table 10).
Characterization of NEKp strains under infection pressures
We compared NEKp/capsule-deficient (isogenic Δcps) strains with EKp (encapsulated K. pneumoniae) strains in vitro and in vivo to assess the impact of capsule synthesis on fitness. Consistent with previous studies21, NEKp/Δcps strains showed increased biofilm production and higher susceptibility to macrophage phagocytosis (Fig. 5a–c). Mouse intraperitoneal infection experiments showed that the isogenic Δcps mutants showed reduced lethality and competitive fitness for dissemination to the lung, liver and spleen compared to the parental EKp strains (Fig. 5d–h). Surprisingly, the serum-killing assay revealed a higher proportion of serum-resistant strains in NEKp strains than in EKp strains (Fig. 6a; KL47 P = 0.018, KL64 P = 2.0 × 10−4). Notably, the isogenic Δcps mutants did not show significant growth advantages over their parents in the Luria–Bertani (LB) media (Extended Data Fig. 6), suggesting that reduced metabolic load due to abolished capsule synthesis is unlikely to be a causative factor. By comparing the antiserum capacity of parental EKp strains, capsule polysaccharide depolymerase-treated (capsule-stripped) EKp strains, isogenic Δcps and ΔcpsΔops mutants, we demonstrated that both CPS and O-antigenpolysaccharide (OPS) play a critical role in serum resistance (Fig. 6b and Extended Data Fig. 7). In addition, we found that isogenic Δcps mutants (except O− strains) showed increased serum resistance along with enhanced O antigen expression compared to the capsule-stripped EKp strains (Fig. 6b and Extended Data Fig. 7). Transcriptomic and real-time PCR (RT-PCR) analyses also revealed the overexpression of LPS and peptidoglycan synthesis genes in Δcps strains compared to parental strains (Extended Data Fig. 8a). These results suggest that disruption of capsule synthesis enhances the synthesis of O-antigen and ultimately increases antiserum capacity. We speculated that the cessation of CPS synthesis might lead to reduced consumption of undecaprenyl phosphate (Und-P) pool, a limiting factor in the biosynthesis of glycans22. This could potentially redirect Und-P for excess O-antigen synthesis. Our observations suggest a potential link between altered Und-P dynamics and changes in serum resistance, as indicated in Extended Data Fig. 8b. Nonetheless, the exact mechanisms and precise Und-P flux alterations following CPS synthesis disruption need to be further investigated.
a, Biofilm formation of NEKp strains and the selected paired EKp strains. Parental EKp strains and their isogenic Δcps mutants are indicated by arrows. Data are shown as the mean ± s.e.m. Each point represents the mean value of three biological replicates of one strain. For clarity, individual error bars for each strain are not shown. Unpaired two-sided Welch’s t-test was performed for statistical analysis. b, Phagocytosis of EKp and NEKp strains by RAW 264.7 macrophages. c, Phagocytosis of EKp and NEKp strains by peritoneal macrophages. Peritoneal macrophages were collected from 7-week-old female C57BL/6J mice. In b and c, WT parental EKp strains were more resistant to phagocytosis than isogenic Δcps strains. Data represent the mean ± s.e.m. of four biological replicates of one strain. Unpaired two-sided Student’s t-test with Welch’s correction was performed for statistical analysis in b and c. d–h, The capsule of KL47 (c,f–h) and KL64 (e,f–h) K. pneumoniae impose competitive fitness in the mouse intraperitoneal infection model. The KL47 (d) and KL64 (e) survival rate was evaluated after intraperitoneal infection of C57BL/6J mice with EKp strains or their isogenic Δcps mutants at the assigned dose (19–89 or 19–89Δcps: 3 × 107 CFU; 16–312, 18–404, 18–729 and 16–140 or their Δcps mutants: 6 × 107 CFU). Kaplan–Meier analysis and log-rank test was performed for statistical analysis. n = 6 (18–404 and 19–89 or their Δcps mutants), n = 5 (18–729, 16–140 and 16–312 or their Δcps mutants). Bacterial load was assessed after intraperitoneal infection of C57BL/6J mice with a 1:1 ratio of WT to isogenic Δcps mutant. WT and Δcps mutants in the lung (f), liver (g) and spleen (h) were quantified at 24 hpi to calculate the competitive index value. Two-sided one-sample t-test was performed to compare the mean of log10-transformed competitive index to a hypothetical value of 0 for each group. Each dot represents an individual mouse. n = 5.
a, Distribution of serum resistance levels of NEKp strains and selected paired EKp strains. Bacteria were incubated in 75% baby rabbit serum, and the antiserum levels were determined. Colours represent different levels of serum resistance. The mean rank difference of two groups was analysed by Cochran–Mantel–Haenszel test. n indicates the number of strains. b, Effect of capsule deficiency on O-antigen expression and its association with serum resistance. Serum-killing assays were performed by incubating the EKp strain 16–312, KL64 CPS depolymerase (Dep4115)-pretreated strain16–312 (capsule-stripped), 16–312Δcps, 16–312ΔcpsΔops and strains complemented with cps or ops with 75% baby rabbit serum for 1 or 2 h at 37 °C. The percentage of survival was determined as the number of surviving bacteria relative to the initial bacterial addition. Unpaired two-sided Student’s t-test with Welch’s correction was used for statistical analysis. Data are shown as the mean ± s.e.m. of three biological replicates and represent one experiment of three independent experiments. LPS was prepared by hot phenol–water method and analysed by silver staining. Core-OS, core-oligosaccharide. c, SBA against parental EKp and isogenic Δcps strains by serum from the patients infected with KL47 or KL64 K. pneumoniae. K. pneumoniae strains were incubated with the heat-inactivated serum from patients for 1 h at 37 °C in the presence of baby rabbit complement. Survival ratios were normalized to the survival strains in the presence of baby rabbit complement alone. Data are the mean ± s.e.m. of four biological replicates. Unpaired two-sided Student’s t-test was used for statistical analysis. d, Model for the surface polysaccharide switch affects K. pneumoniae fitness during infection. The de novo biosynthesis of Und-P can be inhibited by fosmidomycin and increased by overexpression of ispU. CPS synthesis gene mutation results in the inability to utilize Und-P, thereby probably increasing the flow of Und-P to O antigen synthesis, with the consequence of increased biofilm formation, maintained or even increased antiserum capacity and facilitated evasion of antibody-mediated killing, although deficient in dissemination. Gene ispU encodes the undecaprenyl-pyrophosphate synthase; G3P, glyceraldehyde-3-phosphate.
Furthermore, compared to the parental KL47/KL64 EKp strains, the isogenic Δcps mutants showed higher resistance to heat-inactivated sera collected from patients infected with K. pneumoniae KL47/KL64 in the serum bactericidal activity (SBA) assay, suggesting capsule depletion as a potential mechanism for evading humoral immune responses (Fig. 6c).
Collectively, NEKp strains showed a fitness advantage by increasing biofilm formation, serum resistance and anti-SBA but deficiencies in dissemination and anti-phagocytosis (Fig. 6d).
O-antigen-deficient strains in KL64 or KL47 CRKP isolates
Based on the O-antigen-specific phage and silver staining assay, we observed a prevalence of O− strains in both KL47 (13/64, 20.3%) and KL64 (22/76, 29.0%) CRKPs (Extended Data Figs. 9a–e and 10a and Supplementary Table 8). Sequence analysis revealed IS insertions in the rfb region of the O− strains, particularly in the genes wbbL and wbbB in KL47 strains, and wbbO, wbbN and wbbM in KL64 strains (Extended Data Fig. 10b and Supplementary Table 8). Evaluation of the genomic data also revealed a similar prevalence of O− strains in 23.2% (48/207) and 22.3% (71/319) of the KL47 and KL64 isolates, respectively (Extended Data Fig. 10c). The frequency of O− strains showed no difference between body samples (Extended Data Fig. 10d; P = 0.13). In addition, examination of the metagenomic reads revealed that disrupted O antigen clusters were found in 3 out of the 11 samples (>5× depth), demonstrating the presence of O-antigen disrupting mutations in vivo (Extended Data Fig. 10e).
Discussion
This study describes a nationwide, longitudinal retrospective study on CRKP epidemiology in China. We demonstrated the dominance of two K types of KL47 and KL64 in China during 2016–2020, which together accounted for 76.3% of CRKPs. This indicates that KL47 and KL64 capsule types could be considered for future vaccine development. Furthermore, we highlighted the regionally biased distribution of K types, with KL64 predominance in eastern and central regions and KL47 in the north and northeast, as well as region-specific endemic K types including KL19 in eastern China and KL10 in northeastern China. Our findings on K-type prevalence provide a critical foundation for the development of future immunoprophylactic approaches against CRKP infections.
Based on the largest phylogeny of ST11 to our knowledge, we catalogued its global genetic diversity into 12 lineages and attributed the prevalence of KL64 and KL47 in China to the clonal expansion of lineage L1, which has been epidemic in China for decades23. Notably, we also found at least 14 other K types in lineage L1, which might potentially emerge in the future.
We inferred the national transmissions of the epidemic L1 lineage based on its phylogeny. The top two inter-regional healthcare providers, Shanghai and Beijing, were estimated to account for 53% of the inter-regional transmission of L1 strains. Besides, Zhejiang and Henan, part of the largest sources of outbound patients, were also the third and fourth sources of transmission. Moreover, we predicted high frequencies of transmissions from Beijing to other northern regions, and from Shanghai to central and eastern regions (Fig. 3c), which are in line with the different inter-regional healthcare-seeking patterns among patients in eastern and northern China24. The visiting patients may have become infected with CRKP during their stay in cities and brought infection back to the hospitals in their hometown, or vice versa. Thus, the different prevalence of K types between Shanghai and Beijing directly influenced the seroepidemiology of their neighbouring regions, resulting in the current regional distribution of K types (as in Fig. 1b). Our in silico predictions of the national transmissions of lineage L1 highlighted the needs of systematic investigations on the association between CRKPs and the inter-regional healthcare-seeking behaviours.
We attributed 98.2% of the carbapenem resistance to plasmid-mediated carbapenemase acquisition. Similar to previous reports25,26, 89.4% of the CRKPs throughout China carried blaKPC-2 and remained susceptible to CZA. Meanwhile, it is noteworthy that many strains from KL15, KL51 and other rare K types carried blaNDM/blaIMP, which showed resistance to CZA. The emergence of hv-CRKP strains harbouring both carbapenemase and hypervirulence genes has been associated with increased clinical mortality and has become a global concern, particularly in China19. Our study revealed a high yet steadily increasing prevalence of hypervirulent strains (40.6%) among CRKPs in China. Interestingly, most of the hv-CRKPs emerged through the acquisition of virulence plasmids into existing CRKP lineages, such as KL47 and KL64, rather than vice versa, suggesting a greater fitness cost of acquiring carbapenemases than virulence genes.
Interestingly, 12.2% and 7.4% of genotyped KL47 and KL64 CRKP isolates, respectively, showed NEKp phenotypes. These are unlikely to be in vitro artefacts during laboratory subculture, as we also identified disrupted capsular genes in the unprocessed clinical samples by metagenomic analysis. Most of the conversion involved the insertion of an IS element into the initial glycosyltransferase genes in the cps regions, which was unexpected as the IS elements are normally considered to be selfish DNA and not involved in the metabolic process of the host27.
The in vivo presence of the capsule-deficient bacteria and their role during the infection has long been a mystery. In particular, NEKp showed significantly reduced transmission capacity and heterogeneity in serum resistance ability28,29,30, raising the question of whether their capsule deficiency was beneficial or simply a stochastic evolutionary dead-end. Contrary to previous reports mainly in urinary tract infections21, we found similar levels of NEKp from different sites of infection. Our results suggested that the fitness advantage of NEKp is not due to low metabolic burden. Instead, we speculated that in vivo maintenance of NEKp may involve metabolic redistribution of a key resource, Und-P, which is required for the synthesis of extracytoplasmic glycan polymers including peptidoglycan, CPS and O-antigen31. However, In-depth in vivo studies are needed to understand the role of the surface polysaccharide switch along the infection process.
Yet, such in vivo growth advantages have been under strong purifying selection in long-term evolution. Consistent with previous reports32, the NEKp strains were scattered throughout the phylogenetic tree and did not form clusters. Given that the frequency of NEKp strains was stable over the study period and the importance of the capsule for K. pneumoniae survival in vitro29 and dissemination upon infection28, it is tempting to postulate that these NEKp strains have reduced transmissibility and exist as evolutionary terminal forms without the risk of massive clonal transmission.
We also demonstrated the widespread prevalence of O− strains among clinical isolates and proved their existence in vivo using metagenomic analysis. Due to the lack of commercial antiserum specific for O2a or OL101, we invented a phage-based method that tests the presence of the O-antigen by using its specific targeting phages after depolymerizing the capsules using depolymerase. We found high levels (approximately 25%) of O− strains in the two predominant K-type CRKPs. Rough strains induced by the insertion of IS in the rfb regions have only been rarely reported33, and our results suggest that vaccines and monoclonal antibodies targeting O-antigens may have lower in vivo efficiencies than what is expected.
A limitation of this work is that the strains were predominantly collected from patients admitted to large hospitals and therefore may not be representative of the epidemiological trends among patients in smaller, community-based hospitals. In addition, the lack of clinical data from patients hampered our ability to analyse the association between NEKp strains and antimicrobial use and patient immune status.
In conclusion, we describe a 5-year multi-centre surveillance of CRKP-associated infections in China and provide a comprehensive overview of the distribution and evolution of the capsule, AMR and key virulence characteristics of the CRKP strains. We also describe a balanced evolution of CRKPs that has resulted in the maintenance of moderate but stable levels of capsular- and O-antigen-deficient strains in clinical samples.
Methods
Ethics statement
All of our research complies with the relevant ethical regulations. The study protocol was approved by the Institutional Review Board of Huashan Hospital, Fudan University (number 2018-408 and number 2019-460). Patients’ serum, sputum, urine, bile and pus were collected at Ruijin Hospital affiliated with Shanghai Jiaotong University. Approval was obtained from the Ethics Committee of the Ruijin Hospital, Shanghai Jiaotong University (number 2017-205). Verbal consent was obtained from the patients before their participation. All patients and data included in the study were anonymized.
All animal procedures were performed in accordance with the Regulations for the Administration of Affairs Concerning Experimental Animals and approved by the Animal Ethics Review Committee of the School of Pharmacy, Fudan University (project number 2023-03-HSYY-QXH-31) and the Animal Ethics Review Committee of Shanghai Jiaotong University (project number A-2023-009). All experimental C57BL/6J mice (specific pathogen-free grade) were female, 7 weeks old and purchased from Shanghai Jiao Tong University School of Medicine. Mice were housed in a standard laboratory environment with a 12 h light/12 h dark cycle, 21–24 °C ambient temperature and 40–60% relative humidity. Mice were given free access to the standard chow diet and drinking water. Mice were randomly allocated into different groups. The number of mice used in each experiment is indicated in the figure legends. No mice or data points were excluded from the analyses.
Strain collection and antimicrobial susceptibility testing
A total of 1,017 CRKP strains were non-duplicate sequentially collected from K. pneumoniae infected patients admitted to 40 hospitals in 26 Chinese cities every October 1–31 between 2016 and 2020 by the China Antimicrobial Surveillance Network (www.chinets.com). All isolates were identified by matrix-assisted laser desorption ionization–time of flight mass spectrometry (bioMérieux, France). Minimal inhibitory concentrations (MICs) were determined using the reference broth microdilution method recommended by the Clinical and Laboratory Standards Institute (CLSI), which was used to categorize K. pneumoniae as susceptible (S), resistant (R) or intermediate (I). The breakpoints of K. pneumoniae according to CLSI M100-ED31 were interpreted for imipenem (S ≤ 1 mg l−1, R ≥ 4 mg l−1), meropenem (S ≤ 1 mg l−1, R ≥ 4 mg l−1), CZA (S ≤ 8/4 mg l−1, R ≥ 16/4 mg l−1), cefepime (S ≤ 2 mg l−1, R ≥ 16 mg l−1), ceftazidime (S ≤ 4 mg l−1, R ≥ 16 mg l−1), ceftriaxone (S ≤ 1 mg l−1, R ≥ 4 mg l−1), cefoperazone–sulbactam (according to cefoperazone S ≤ 16 mg l−1, R ≥ 64 mg l−1), piperacillin–tazobactam (S ≤ 16 mg l−1, R ≥ 128 mg l−1), cefuroxime (S ≤ 8 mg l−1, R ≥ 32 mg l−1), cefazolin (S ≤ 2 mg l−1, R ≥ 8 mg l−1), amikacin (S ≤ 16 mg l−1, R ≥ 64 mg l−1), trimethoprim–sulfamethoxazole (S ≤ 2/38 mg l−1, R ≥ 4/76 mg l−1), aztreonam (S ≤ 4 mg l−1, R ≥ 16 mg l−1), ciprofloxacin (S ≤ 0.25 mg l−1, R ≥ 1 mg l−1) and levofloxacin (S ≤ 0.5 mg l−1, R ≥ 2 mg l−1)34. Tigecycline MICs were interpreted using the US Food and Drug Administration MIC breakpoints for Enterobacterales (S ≤ 2 mg l−1, R ≥ 8 mg l−1) (https://www.fda.gov/drugs/development-resources/antibacterial-susceptibility-test-interpretive-criteria). European Committee on Antimicrobial Susceptibility Testing (41) (EUCAST) MIC interpretive breakpoints were used for polymyxin B (S ≤ 2 mg l−1, R ≥ 4 mg l−1). Escherichia coli ATCC 25922 and E. coli ATCC 35218 were tested as the quality control strains for antimicrobial susceptibility testing. The K. pneumoniae strains resistant to at least one of the carbapenem antibiotics (meropenem or imipenem) were defined as CRKP. Abbreviations and their expansions in this study are listed in Supplementary Table 11.
More than half of the patients were male (667; 65.6%). The mean age of the patients was 56.17 (±18.70) years. The most common specimen sources were sputum (458/1,017, 45.03%), blood culture (242/1,017, 23.80%) and urine (120/1,017, 11.80%). See details in Supplementary Table 1. Most isolates (41.00%) were collected from patients in medical intensive care units.
K-typing by wzi genotyping
To identify the K types of K. pneumoniae strain, the wzi allele was amplified by PCR and aligned with the wzi sequences deposited in the database of Institut Pasteur (http://bigsdb.web.pasteur.fr)31. KL14, KL64, KL15, KL51 and KL102 were further identified by PCR amplification of the variable sequence of the wzy gene35,36,37. Besides, the Kaptive software was also used to identify the capsule synthesis loci (K-loci or KL)38. The primers used for genotyping are listed in Supplementary Table 12.
PCR screening for carbapenem resistance genes and virulence-associated genes
The presence of common carbapenem resistance genes (blaIMP, blaNDM, blaVIM, blaKPC and blaOXA-48-like) and virulence-associated genes (rmpA, rmpA2, iroB, iucA and peg344) was confirmed by PCR using the primers described in Supplementary Table 12. The positive PCR amplicons of carbapenem resistance genes were sequenced and aligned with the sequences released from GenBank (www.ncbi.nlm.nih.gov/blast/).
Whole-genome sequencing and bioinformatics analysis
We performed whole-genome sequencing on 207 KL47 and 319 KL64 isolates to obtain a phylogenetic overview of the two most common K-type CRKPs (strains were randomly selected for sequencing, and the selection criteria are shown in Extended Data Fig. 1) and on non-carbapenemase-producing CRKP strains to analyse other mechanisms of carbapenem resistance. Genomic libraries were prepared using the Rapid Plus DNA Lib Prep Kit for Illumina (catalogue number RK20208) and sequenced using Illumina NovaSeq 6000. The obtained reads were trimmed by Trimmomatic v0.39, and strain assemblies were generated using EToKi assemble39. The assembled genomes were annotated using PROKKA40. ISs were predicted using ISfinder (http://www-is.biotoul.fr). AMR genes and virulence genes were predicted using Kleborate41.
Phylogenetic analysis
Three of the 526 genomic sequenced strains were not in ST11 and therefore not included in the phylogenetic analysis. The remaining 523 genomes, plus all public ST11 genomes, were aligned to a reference genome (GCF_011066505.1; sample from blood, Hong Kong, China, 2016) using the EToKi align module to obtain a multiple sequence alignment of the nonrepetitive core genomic regions shared by ≥95% of the genomes. The resulting alignments were subjected to a maximum-likelihood phylogeny using the EToKi phylo module; the recombinant regions were removed using RecHMM42 and were visualized using Phandango43. Furthermore, we used EToKi MLSType to genotype all ST11 genomes based on the scgMLST_629S scheme hosted in Institut Pasteur (https://bigsdb.pasteur.fr/klebsiella/). All the obtained core genome multilocus sequence typing (cgMLST) profiles were separated into clonal groups using the LINcoding script (https://gitlab.pasteur.fr/BEBP/LINcoding) with a cutoff of 69.7933% allele similarity as described in https://bigsdb.pasteur.fr/klebsiella/cgmlst-lincodes/.
Inferences of population dynamics for lineage L1
The origin time of the ST11 population was estimated using BactDating44. Parallel chains of 5 × 106 samples each were run for each of the substitution models of ‘strictgamma’, ‘mixedgamma’, and ‘carc’. The first 50% of the chain (3 × 106 samples) for each model was discarded as burn-ins, and the convergence of the run was determined by ensuring effective sampling sizes of >100 for all parameters. The results from all samples were compared based on their Bayes factors using the modelcompare function in BactDating, which indicated that the ‘strictgamma’ model was optimal. Finally, the dynamics of effective population sizes were estimated using the skygrowth package in R45, and the geographic origins of each node in the tree were estimated using the maximum-likelihood algorithm implemented in TreeTime46. In addition, we also estimated the ancestral geographic origins of each node using the Ancestral Character Estimation function in the APE package in R with three different models of ‘ER’, which assumes equal transmission rates across all regions, ‘SYM’, which assumes different, yet symmetric rates for transmissions between different pairs of regions, and ‘ARD’, which is an all-rates-different model. These models generated slightly different results, which are summarized in Extended Data Fig. 3. The tree was visualized using iTOL v647.
Evaluation of temporal signal in lineage L1
The presence of a temporal signal in lineage L1 was tested using three approaches. The regression of root-to-tip distances and dates of isolation was estimated using TempEst with a correlation coefficient (R) of 0.18 and P value of 8.2 × 10−12. We then randomly permutated the isolation dates of the strains 10 times and estimated their R values as shown in Extended Data Fig. 2b. The same datasets were also used for BactDating inferences as described above, and their substitution rates were compared with the rate from the actual data, which was also shown in Extended Data Fig. 2c.
Identification of carbapenemase-encoding and hypervirulence-associated plasmids
To detect plasmids in the ST11 isolates, all 6,779 complete sequences of Klebsiella plasmids were downloaded from the National Center for Biotechnology Information (NCBI) RefSeq database (July 2022) and used as references. All 3,570 ST11 genomes were compared with the reference plasmid sequences using BLASTn; the alignment regions for each plasmid among the assemblies were summarized, and only plasmids that have >50% of their sequences aligned with >85% identities were kept. For each genome, we reordered its associated plasmid references according to the alignment scores and selected the hits using a ‘Best-first’ greedy algorithm that is similar to what is described in ref. 48. Briefly, for each iteration, the reference plasmid with the greatest alignment score was selected, and all contigs associated with it were taken out. This process was repeated until there was no hit left. Furthermore, to identify hypervirulence-associated plasmids, we predicted the presence of the carbapenemase or the five hypervirulence-associated genes (iucA, iroB, rmpA, rmpA2 and peg344) in the selected contigs based on BLASTn alignments. Only the plasmids that carry at least one of these functional genes were reported. The identified plasmids were then aligned onto the NCBI RefSeq database again to obtain similar plasmids and had their incompatibility and MOB types determined using the MOB-Typer software49.
Capsular Quellung assay for genotyped KL47 and KL64 K. pneumoniae strains
The traditional serologic method, the Quellung assay, was performed to further confirm the K-type results for these KL47 (263 strains) and KL64 (513 strains) clinical strains in this study15. Rabbit K47-antiserum and K64-antiserum were prepared as described previously15. Bacteria in 1× phosphate-buffered saline (PBS) were mixed with the equal volume of rabbit K64-antiserum (titre of 1:1.5 × 107) or K47-antiserum (titre of 1: 6.1 × 106) or control rabbit serum and incubated with the methylene blue solution (Sangon Biotech, catalogue number A610622) on a glass slide for 15 min. Finally, the mixture was observed under a light microscope.
Capsule extraction and uronic acid quantification
The capsule polysaccharide of strains was extracted and quantified as previously described21,50. Briefly, 1 × 109 colony forming units (CFU) bacteria were pelleted for capsule uronic acid extraction. Bacteria were mixed with 1% Zwittergent 3–14 detergent (Sangon Biotech, catalogue number A610552) in 100 mM citric acid (Sangon Biotech, catalogue number A610055). Then uronic acid was precipitated by ethanol (Sinopharm Chemical Reagent, catalogue number 10009218), incubated with 0.0125 M sodium tetraborate/sulfuric acid (tetraborate, Sigma-Aldrich, catalogue number 221732; sulfuric acid, Sinopharm Chemical Reagent, catalogue number 10021608) and 0.125% carbazole absolute ethanol (carbazole, Sangon Biotech, catalogue number A600269), finally measured at 530 nm and correlated to a standard curve of d-glucuronic acid.
Transmission electron microscopy
Bacteria of 5 × 108 CFU were pelleted and fixed in 2.5% glutaraldehyde (Sangon Biotech, catalogue number A600875) and 4% polyformaldehyde (Servicebio, catalogue number G1101) for 2 h at room temperature. Then the ultra-thin sections were prepared, and the image from transmission electron microscopy was obtained with the Hitachi transmission electron microscope H-9500 (Tokyo, Japan) at the Electron Microscopy Imaging Laboratory of Shanghai Jiaotong University School of Medicine (Shanghai, China).
Estimation of the mutation rate of capsule deletion in vitro
A single colony of the EKp strain was plated on blood agar plate and incubated at 37 °C for 48 h. All bacterial colonies were then collected and resuspended in 1× PBS. The mutation rate was obtained by counting the proportion of strains that appeared translucent over the total colonies.
Metagenomic sequencing and analysis
Clinical specimens were obtained from Ruijin Hospital Affiliated to Shanghai Jiaotong University School of Medicine. The sputum, urine, bile and pus used for metagenomic sequencing were collected from K. pneumoniae infected patients, 83.3% (10/12) of whom were male. The mean age of the patients was 66.00 (±11.59) years (for details, see Supplementary Table 10). Sputum and pus specimens were incubated with 4% sterilized sodium hydroxide (Sinopharm Chemical Reagent, catalogue number 10019718) for 1 h at room temperature to liquefy. Urine and bile specimens were centrifuged to obtain enriched specimens pellet. All specimens were incubated at 83 °C for 30 min for sterilization, then incubated with 5 mg ml−1 lysozyme (Vazyme, catalogue number DE103) and 32 U ml−1 lysostaphin (Sigma-Aldrich, catalogue number L7386) for 4 h at 37 °C and incubated with 0.1 mg ml−1 protease K (LABLEAD Biotech, catalogue number K0510) for 2 h at 65 °C. Finally, bacterial DNA was further extracted and purified using the TIANamp Bacterial DNA Kit (TIANGEN Biotech, catalogue number DP302). Paired-end libraries with insert sizes of ~300 bp were prepared using Illumina’s standard genomic DNA library preparation procedure (VAHTS Universal DNA Library Prep kit for Illumina V3) and sequenced on an Illumina NovaSeq 6000 using the S4 reagent kits (v.1.5) according to the manufacturer’s instructions. Low-quality bases and adapters in the metagenomic reads were screened and removed using BBDuk (https://sourceforge.net/projects/bbmap/). The presence of K. pneumoniae in the samples was determined using both KRAKEN (https://ccb.jhu.edu/software/kraken/) and SPARSE (https://github.com/zheminzhou/SPARSE). Sequences of the K- and O-antigen gene clusters obtained from Kaptive were used as references to identify sequence variations. All reads in each sample were aligned to these reference sequences using minimap2 and visually examined with the help of samtools v.1.2. The long-range deletions and insertions of transposons were identified by recognizing multiple reads encompassing the conjugative sites. The frameshifts and nonsense mutations in the coding sequences were recognized by comparing all sequence variations with gene annotations.
Deletion clones and complementary plasmid construction
The K. pneumoniae ∆cps (∆wcaJ, ∆wbaP or ∆wbaP∆wcaA), ∆ops (∆wbbN or ∆wbbL) and ∆cps∆ops (∆wcaJ∆wbbN) mutants were constructed using the λ Red-dependent recombination system and the flippase (FLP)/FLP recognition target (FRT) recombination system according to the methods reported previously51,52. First, the donor DNA comprising 500 bp upstream of the target gene, the hygromycin-resistant gene and 500 bp downstream of the target gene was constructed via Gibson. The hygromycin-resistant gene flanked by the FRT was PCR-amplified from pUC19-Hph plasmid. Then the thermosensitive plasmid pKOBEG harbouring the apramycin-resistant gene was introduced into the competent cells derived from the wild-type (WT) strain using electroporation technology. The pKOBEG carried the λ phage red operon controlled by a promoter under the induction of arabinose. The donor DNA was then electroporated into WT pKOBEG. Ultimately, the cps or ops gene in the WT strain was replaced by the FRT-flanked hygromycin-resistant gene. The mutants were selected on LB agar plates containing apramycin (Sangon Biotech, catalogue number A600090) and hygromycin (Rhawn, catalogue number R053999) and confirmed by PCR and Sanger sequencing. The 16–312∆cps∆ops double knockout mutant was conducted by first replacing cps (wcaJ) using the hygromycin-resistant gene, then removing the hygromycin resistance gene by FLP /FRT recombination method and finally further deleting the ops (wbbN) gene by the hygromycin-resistant gene replacement. Plasmid pKOBEG was removed by growth at 42 °C with shaking.
For complementary plasmid construction, the cps or ops genes of KL64 or KL47 strains were amplified from K. pneumoniae strains 16–312 and 19–249, respectively. They were then cloned into the pACYC184 or pBAD33 vector, and the recombinant plasmids were transformed into the cps or ops mutant strains. In addition, the 16–312Δcps::cps (16–312∆wcaJ::wcaJ) strain was generated by the λ-red-mediated in situ complementation method. Briefly, donor DNA containing 500 bp upstream of the cps gene, the cps gene, the hygromycin resistance gene and 500 bp downstream of cps gene was electroporated into 16–312Δcps strain harbouring pKOBEG vector. Mutants were then selected on LB agar plates containing apramycin and hygromycin. Expression of cps or ops genes was confirmed by the Quellung reaction assay or silver staining, respectively. Primers used for deletion clone construction and complementation and details of the engineered mutants are listed in Supplementary Tables 12 and 13 The gene in cps-locus or rfb-locus and their putative gene products are listed in Supplementary Table 14.
Macrophage phagocytosis assay
The phagocytosis assay was performed using the mouse macrophage cell line RAW 264.7 (ATCC catalogue number TIB-71) and peritoneal macrophages as previously described53. Peritoneal macrophages were collected from 7-week-old female C57BL/6J mice on the 5th day after intraperitoneal injection of 1 ml 5% thioglycollate broth (BD Difco, catalogue number 211716)54. Briefly, 5 × 105 cells were infected with bacteria at a multiplicity of infection of 50 for 1 h. The cells were then washed three times with 1× PBS and treated with 500 μl Dulbecco’s modified eagle medium (Servicebio, catalogue number G4515) containing 300 μg ml−1 gentamycin (Sangon Biotech, catalogue number A506614) or amikacin (Solarbio, catalogue number A9660) for 1 h to eliminate the extracellular bacteria. After washing three times with 1× PBS, the cells were treated with 1 ml of 1% TritonX-100 (Sangon Biotech, catalogue number A110694) for 10 min to release the intracellular bacteria. Then intracellular bacteria were counted by serial dilution agar plating method.
In vitro bacterial competition assay
Each WT strain (1 × 105 ml−1) was mixed 1:1 with the isogenic Δcps mutant in LB medium and incubated at 37 °C for 24 h. Bacteria were then serially diluted and plated on LB and LB containing hygromycin (Rhawn, catalogue number R053999) plates. The ratio of ∆cps (the number of colonies on hygromycin LB plates) to WT (the number of colonies on LB plates minus the number of colonies on hygromycin LB plates) was calculated to obtain the competitive index value.
In vivo bacterial competition assay
Groups of five 7-week-old female C57BL/6J mice were infected intraperitoneally with an assigned dose of WT or Δcps mutant to evaluate the systemic infectivity of the bacteria. Survival curves were monitored for 10 days. Differences in mouse survival were determined by Kaplan–Meier survival analysis with log-rank test. The in vivo bacterial competition assay was performed in 7-week-old female C57BL/6J mice (n = 5). Each WT strain was mixed with the isogenic Δcps mutant at a ratio of 1:1 in 200 µl 1× PBS and injected intraperitoneally into mice. After 24 h post infection, mice were euthanized, and the burdens of WT and Δcps mutant in lung, liver and spleen were counted by serial dilution on LB agar plates and LB agar plates containing hygromycin (Rhawn, catalogue number R053999), respectively. The ratio of mutant:WT was calculated to obtain the competitive index value.
Biofilm formation assay
The ability of K. pneumoniae strains to form biofilms was determined as described previously21,55. Briefly, bacteria were incubated in tryptic soy broth medium (Hopebio, catalogue number HB4150) to optical density (OD) = 0.4. The bacterial suspension was incubated in a 96-well microtitre plate at 37 °C for 48 h, then stained with 0.4% crystal violet (Macklin, catalogue number C805211) at 37 °C for 45 min and destained with 33% acetic acid (Sinopharm Chemical Reagent, catalogue number 10000208) for 30 min. Finally, the sample was read at a wavelength of 595 nm.
Serum resistance assay
The serum resistance ability of the strains was estimated using the serum resistance assay. About 5 × 104 CFU bacteria were incubated with 75% baby rabbit complement at 37 °C for 1, 2 and 3 h. Bacterial counts were determined to enumerate the survival rate. The survival rate was calculated using the following formula: survival rate 1 (SR1) = (CFU surviving at 1 h post-complement treatment/CFU surviving in initial) × 100; SR2 = (CFU surviving at 2 h post-complement treatment/CFU surviving in initial) × 100; SR3 = (CFU surviving at 3 h post-complement treatment/CFU surviving in initial) × 100. Each isolate was classified as previously described56. Briefly, serum resistance level 1 is SR1 and SR2 < 10%, and SR3 < 0.1%; level 2 is SR1 and SR2 between 10% and 100%, and SR3 < 10%; level 3 is SR1 > 100%, SR2 and SR3 < 100%; level 4 is SR1 and SR2 > 100%, and SR3 < 100%; level 5 is SR1, SR2 and SR3 > 100%, and SR2 > SR3; level 6 is SR1, SR2 and SR3 > 100%, and SR1 < SR2 < SR3. Isolates belonging to levels 1 and 2, levels 3 and 4, and levels 5 and 6 were defined as ‘sensitive’, ‘intermediate’ and ‘resistant’, respectively.
To compare WT/Δcps strains with depolymerase-treated strains, bacteria were incubated with their corresponding K-type depolymerase (KL47 strains with Dep 4257 and KL64 strains with Dep 4115, at a final concentration of 100 μg ml−1), or K-type-irrelevant depolymerase (Dpo717, which were specific for KL19 CPS) for 1 h before incubation with 75% baby rabbit serum. The percentage of survival was determined as the number of surviving bacteria relative to the initial bacterial addition.
Furthermore, fosmidomycin and ispU overexpression were performed to evaluate the effect of Und-P on serum resistance. To inhibit the synthesis of Und-P, 16-312Δcps mutants were cultured overnight in LB medium with or without 500 ng ml−1 fosmidomycin (Rhawn, catalogue number R047510) and subcultured to OD = 0.7. To increase the synthesis of Und-P, a recombinant pBAD33-ispU plasmid with an arabinose-induced promoter was constructed and transformed into Δcps mutants. Bacteria were grown overnight in LB medium containing 10 mM arabinose and 50 µg ml−1 apramycin and subcultured to OD = 0.7. Finally, bacteria were incubated with 75% baby rabbit complement at 37 °C for 1 h. Bacterial viability was determined by the serial dilution agar plating method.
LPS isolation and electrophoresis
A total of 1010 CFU bacteria were pelleted for LPS extraction. Capsular strains of the depolymerase treatment group were treated with the corresponding K-type depolymerase or K-type-irrelevant depolymerase at 37 °C for 2 h. Then, 100 µg ml−1 deoxyribonuclease (Roche, catalogue number 4716728001), 50 µg ml−1 ribonuclease (TIANGEN Biotech, catalogue number RT405) and 200 µg ml−1 proteinase K (LABLEAD Biotech, catalogue number K0510) were used to eliminate nucleic acids and protein. LPS was extracted by the hot phenol/water method58. Finally, samples were run on 15% sodium dodecyl sulfate–polyacrylamide gels and visualized by silver staining.
RNA sequencing
RNA sequencing was performed as previously described with slight modification59,60. K. pneumoniae strains 16–312 and 16–312Δcps mutant were grown in LB to an OD600 of 0.7. Bacteria were pelleted by centrifugation, snap frozen in liquid nitrogen and cryopreserved at −80 °C. Total RNA from bacteria was extracted and purified using the RNAprep Pure Cell / Bacteria Kit (TIANGEN Biotech, catalogue number DP430). RNA integrity was assessed using the Agilent 2100 Bioanalyzer. RNA sequencing was performed at the Shanghai Personal Biotechnology (Shanghai, China). P < 0.05 was defined as significant difference. The LPS and peptidoglycan synthetic genes and their putative gene products are listed in Supplementary Table 14.
Quantitative RT-PCR
Purified RNA was reverse transcribed to complementary DNA using the Thermo Scientific RevertAid RT Kit (Thermo Scientific, catalogue number M1631). Transcript levels of wbbM, LpxD, LpxM, LpxA, mraY and murA were detected by quantitative RT-PCR. The relative abundance of LPS- and peptidoglycan-synthesizing genes was calculated by the 2−ΔΔCT method using the 16S ribosomal RNA gene as a reference. Primers for quantitative RT-PCR are listed in Supplementary Table 12.
Serum bactericidal activity
The SBA assay was determined using a method previously reported with slight modification61,62. WT strain and isogenic Δcps mutant were incubated with 10% heat-inactivated serum from patients (infected with KL47 or KL64 K. pneumoniae strains) in the presence of 15% baby rabbit complement or 15% baby rabbit complement alone for 1 h. The percentage of survival was calculated by dividing the viable counts of patient serum plus complement by complement alone. The serum of infected patients was obtained from Ruijin Hospital Affiliated to Shanghai Jiaotong University School of Medicine; 62.5% (5/8) of patients were male. The mean age of the patients was 51.13 (±13.78) years.
Statistical analyses
Unpaired two-sided Student’s t-test was used to compare the means between two groups. The Welch’s correction was used when variation was unequal. Pearson’s chi-square was used to compare groups for proportion data. The Cochran–Mantel–Haenszel test was used to compare the mean rank difference of two groups in serum resistance assay. The Cochran–Armitage test for trend was used to analyse the temporal trend in the proportions of the K types, hypervirulent strains and NEKp strains from 2016 to 2020. Differences in mouse survival were determined by Kaplan–Meier survival analysis with log-rank test. Two-sided one-sample t-test was used to compare the mean of log10-transformed competitive index or competitive index to a hypothetical value of 0 or 1 in competition assay. No comparison between groups was involved in the competition assay. P < 0.05 was considered statistically significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The raw reads of 542 K. pneumoniae sequenced in this study were uploaded to the NCBI database under the project PRJNA1028672. A total of 3,047 publicly available genomes were enrolled including 2,695 public ST11 K. pneumoniae genomes which were available in the NCBI database under various projects (Supplementary Table 6), and 352 ST11 K. pneumoniae genomes were downloaded from Genome Sequence Archive63 in Chinese National Genomics Data Center64 under project PRJCA003173 (n = 300) and PRJCA012323 (n = 52). The metagenomic sequences of clinical samples acquired during the capsule and O-antigen trial parts were uploaded to the NCBI database under the project PRJNA1028672. The transcriptome sequencing data were uploaded to the NCBI database under the project PRJNA1028672 as well. Reference genome for phylogenetic analysis of ST11 strains were set as GCF_011066505.1. The original images and data are provided in the Source data. Source data are provided with this paper.
Code availability
The SRA Toolkit (2.8.0) was used to download genomes and short reads from the NCBI. The following software were used in the analysis: Trimmomatic v.0.39, EToKi v.1.3, PROKKA v.1.14, ISfinder v.1, Kleborate v.2.3.2, Kaptive v.2.0.7, RecHMM v.1, Phandango v.1.3.0, BactDating v.1.1, TreeTime v.0.10.1, iTOL v.6, TempEst v.1.5.3, BLASTn v.2.9.0+, MOB-Typer v.3.1.0, BRIG v.0.95, BBDuk v.1, KRAKEN v.2.1.2, minimap2 v.2.26-r1175, samtools v.1.2, SPARSE v.1, R skygrowth v.0.3.1, R APE v.5.7.1, LINcoding script v.1 and search plasmic.git v.1 (https:/eithub.com/xiaoliu8/searchplasmic.git).
References
Shrivastava, S., Shrivastava, P. & Ramasamy, J. World Health Organization releases global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. J. Med. Soc. https://doi.org/10.4103/jms.jms_25_17 (2018).
Antimicrobial Resistance Collaborators Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 399, 629–655 (2022).
Follador, R. et al. The diversity of Klebsiella pneumoniae surface polysaccharides. Microb. Genom 2, e000073 (2016).
Singh, S. et al. LPS O antigen plays a key role in Klebsiella pneumoniae capsule retention. Microbiol. Spectr. 10, e0151721 (2022).
Rollenske, T. et al. Cross-specificity of protective human antibodies against Klebsiella pneumoniae LPS O-antigen. Nat. Immunol. 19, 617–624 (2018).
Diago-Navarro, E. et al. Novel, broadly reactive anticapsular antibodies against carbapenem-resistant Klebsiella pneumoniae protect from infection. mBio https://doi.org/10.1128/mBio.00091-18 (2018).
Feldman, M. F. et al. A promising bioconjugate vaccine against hypervirulent Klebsiella pneumoniae. Proc. Natl Acad. Sci. USA 116, 18655–18663 (2019).
Diago-Navarro, E. et al. Antibody-based immunotherapy to treat and prevent infection with hypervirulent Klebsiella pneumoniae. Clin. Vaccine Immunol. https://doi.org/10.1128/CVI.00456-16 (2017).
Malachowa, N. et al. Vaccine protection against multidrug-resistant Klebsiella pneumoniae in a nonhuman primate model of severe lower respiratory tract infection. mBio https://doi.org/10.1128/mBio.02994-1 (2019).
Pan, Y. J. et al. Genetic analysis of capsular polysaccharide synthesis gene clusters in 79 capsular types of Klebsiella spp. Sci. Rep. 5, 15573 (2015).
Zhao, L. et al. Molecular epidemiology of antimicrobial resistance, virulence and capsular serotypes of carbapenemase-carrying Klebsiella pneumoniae in China. Antibiotics https://doi.org/10.3390/antibiotics11081100 (2022).
Wang, M. et al. Clinical outcomes and bacterial characteristics of carbapenem-resistant Klebsiella pneumoniae complex among patients from different global regions (CRACKLE-2): a prospective, multicentre, cohort study. Lancet Infect. Dis. 22, 401–412 (2022).
Zhang, Y. et al. Evolution of hypervirulence in carbapenem-resistant Klebsiella pneumoniae in China: a multicentre, molecular epidemiological analysis. J. Antimicrob. Chemother. 75, 327–336 (2020).
Hennart, M. et al. A dual barcoding approach to bacterial strain nomenclature: genomic taxonomy of Klebsiella pneumoniae strains. Mol. Biol. Evol. https://doi.org/10.1093/molbev/msac135 (2022).
Li, J. et al. Identification of a depolymerase specific for K64-serotype Klebsiella pneumoniae: potential applications in capsular typing and treatment. Antibiotics https://doi.org/10.3390/antibiotics1002014 (2021).
Wang, J. et al. The molecular epidemiology of prevalent Klebsiella pneumoniae strains and humoral antibody responses against carbapenem-resistant K. pneumoniae infections among pediatric patients in Shanghai. mSphere 7, e0027122 (2022).
Hua, Y. et al. Characterization and functional studies of a novel depolymerase against K19-Type Klebsiella pneumoniae. Front. Microbiol. 13, 878800 (2022).
Russo, T. A. et al. Identification of biomarkers for differentiation of hypervirulent Klebsiella pneumoniae from classical K. pneumoniae. J. Clin. Microbiol. https://doi.org/10.1128/jcm.00776-18 (2018).
Gu, D. et al. A fatal outbreak of ST11 carbapenem-resistant hypervirulent Klebsiella pneumoniae in a Chinese hospital: a molecular epidemiological study. Lancet Infect. Dis. 18, 37–46 (2018).
Zhou, K. et al. Novel subclone of carbapenem-resistant Klebsiella pneumoniae sequence type 11 with enhanced virulence and transmissibility, China. Emerg. Infect. Dis. 26, 289–297 (2020).
Ernst, C. M. et al. Adaptive evolution of virulence and persistence in carbapenem-resistant Klebsiella pneumoniae. Nat. Med. 26, 705–711 (2020).
Tatar, L. D., Marolda, C. L., Polischuk, A. N., van Leeuwen, D. & Valvano, M. A. An Escherichia coli undecaprenyl-pyrophosphate phosphatase implicated in undecaprenyl phosphate recycling. Microbiology 153, 2518–2529 (2007).
Qi, Y. et al. ST11, the dominant clone of KPC-producing Klebsiella pneumoniae in China. J. Antimicrob. Chemother. 66, 307–312 (2011).
Yang, Y. & Wang, Y. Analysis of the characteristics of cross-regional patient groups and differences in hospital service utilization in Beijing. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph19063227 (2022).
Chen, L. et al. Outbreak of IncX8 plasmid-mediated KPC-3-producing enterobacterales infection, China. Emerg. Infect. Dis. 28, 1421–1430 (2022).
Findlay, J., Poirel, L., Juhas, M. & Nordmann, P. KPC-mediated resistance to ceftazidime–avibactam and collateral effects in Klebsiella pneumoniae. Antimicrob. Agents Chemother. 65, e0089021 (2021).
Agren, J. A. & Clark, A. G. Selfish genetic elements. PLoS Genet. 14, e1007700 (2018).
Tan, Y. H., Chen, Y., Chu, W. H. W., Sham, L. T. & Gan, Y. H. Cell envelope defects of different capsule-null mutants in K1 hypervirulent Klebsiella pneumoniae can affect bacterial pathogenesis. Mol. Microbiol. 113, 889–905 (2020).
Buffet, A., Rocha, E. P. C. & Rendueles, O. Nutrient conditions are primary drivers of bacterial capsule maintenance in Klebsiella. Proc. Biol. Sci. 288, 20202876 (2021).
Wang, S. et al. Evolution of virulence, fitness, and carbapenem resistance transmission in ST23 hypervirulent Klebsiella pneumoniae with the capsular polysaccharide synthesis gene wcaJ inserted via insertion sequence elements. Microbiol. Spectr. 10, e0240022 (2022).
Brisse, S. et al. wzi gene sequencing, a rapid method for determination of capsular type for Klebsiella strains. J. Clin. Microbiol. 51, 4073–4078 (2013).
Haudiquet, M., Buffet, A., Rendueles, O. & Rocha, E. P. C. Interplay between the cell envelope and mobile genetic elements shapes gene flow in populations of the nosocomial pathogen Klebsiella pneumoniae. PLoS Biol. 19, e3001276 (2021).
Artyszuk, D. et al. The impact of insertion sequences on O-serotype phenotype and its O-locus-based prediction in Klebsiella pneumoniae O2 and O1. Int. J. Mol. Sci. https://doi.org/10.3390/ijms21186572 (2020).
Performance Standards for Antimicrobial Susceptibility Testing 31st edn, CLSI supplement M100 (Clinical and Laboratory Standards Institute, 2021).
Pan, Y. J. et al. Capsular types of Klebsiella pneumoniae revisited by wzc sequencing. PLoS ONE 8, e80670 (2013).
Hsu, C. R., Lin, T. L., Pan, Y. J., Hsieh, P. F. & Wang, J. T. Isolation of a bacteriophage specific for a new capsular type of Klebsiella pneumoniae and characterization of its polysaccharide depolymerase. PLoS ONE 8, e70092 (2013).
Yu, F. et al. Multiplex PCR analysis for rapid detection of Klebsiella pneumoniae carbapenem-resistant (sequence type 258 [ST258] and ST11) and hypervirulent (ST23, ST65, ST86, and ST375) strains. J. Clin. Microbiol. 56, e00731–18 (2018).
Lam, M. M. C., Wick, R. R., Judd, L. M., Holt, K. E. & Wyres, K. L. Kaptive 2.0: updated capsule and lipopolysaccharide locus typing for the Klebsiella pneumoniae species complex. Microb. Genom. https://doi.org/10.1099/mgen.0.000800 (2022).
Zhou, Z. et al. The EnteroBase user’s guide, with case studies on Salmonella transmissions, Yersinia pestis phylogeny, and Escherichia core genomic diversity. Genome Res. 30, 138–152 (2020).
Seemann, T. Prokka: rapid prokaryotic genome annotation. Bioinformatics 30, 2068–2069 (2014).
Lam, M. M. C. et al. A genomic surveillance framework and genotyping tool for Klebsiella pneumoniae and its related species complex. Nat. Commun. 12, 4188 (2021).
Zhou, Z. et al. Transient Darwinian selection in Salmonella enterica serovar Paratyphi A during 450 years of global spread of enteric fever. Proc. Natl Acad. Sci. USA 111, 12199–12204 (2014).
Hadfield, J. et al. Phandango: an interactive viewer for bacterial population genomics. Bioinformatics 34, 292–293 (2018).
Didelot, X., Croucher, N. J., Bentley, S. D., Harris, S. R. & Wilson, D. J. Bayesian inference of ancestral dates on bacterial phylogenetic trees. Nucleic Acids Res. 46, e134 (2018).
Volz, E. M. & Didelot, X. Modeling the growth and decline of pathogen effective population size provides insight into epidemic dynamics and drivers of antimicrobial resistance. Syst. Biol. 67, 719–728 (2018).
Sagulenko, P., Puller, V. & Neher, R. A. TreeTime: maximum-likelihood phylodynamic analysis. Virus Evol. 4, vex042 (2018).
Letunic, I. & Bork, P. Interactive Tree Of Life (iTOL) v5: an online tool for phylogenetic tree display and annotation. Nucleic Acids Res. 49, W293–W296 (2021).
Pierce, N. T., Irber, L., Reiter, T., Brooks, P. & Brown, C. T. Large-scale sequence comparisons with sourmash. F1000Research https://doi.org/10.12688/f1000research.19675.1 (2019).
Robertson, J. & Nash, J. H. E. MOB-suite: software tools for clustering, reconstruction and typing of plasmids from draft assemblies. Microb. Genom. https://doi.org/10.1099/mgen.0.000206 (2018).
Domenico, P., Schwartz, S. & Cunha, B. A. Reduction of capsular polysaccharide production in Klebsiella pneumoniae by sodium salicylate. Infect. Immun. 57, 3778–3782 (1989).
Chaveroche, M. K., Ghigo, J. M. & d’Enfert, C. A rapid method for efficient gene replacement in the filamentous fungus Aspergillus nidulans. Nucleic Acids Res. 28, E97 (2000).
Datsenko, K. A. & Wanner, B. L. One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc. Natl Acad. Sci. USA 97, 6640–6645 (2000).
Panjaitan, N. S. D. et al. The PTS components in Klebsiella pneumoniae affect bacterial capsular polysaccharide production and macrophage phagocytosis resistance. Microorganisms https://doi.org/10.3390/microorganisms9020335 (2021).
Bengoechea, J. A., Singla, S., Harjai, K., Katare, O. P. & Chhibber, S. Encapsulation of bacteriophage in liposome accentuates its entry in to macrophage and shields it from neutralizing antibodies. PLoS ONE https://doi.org/10.1371/journal.pone.0153777 (2016).
Heiden, S. E. et al. A Klebsiella pneumoniae ST307 outbreak clone from Germany demonstrates features of extensive drug resistance, hypermucoviscosity, and enhanced iron acquisition. Genome Med. 12, 113 (2020).
Abate, G., Koh, T. H., Gardner, M. & Siu, L. K. Clinical and bacteriological characteristics of Klebsiella pneumoniae causing liver abscess with less frequently observed multi-locus sequences type, ST163, from Singapore and Missouri, US. J. Microbiol. Immunol. Infect. 45, 31–36 (2012).
Wu, Y. et al. A novel polysaccharide depolymerase encoded by the phage SH-KP152226 confers specific activity against multidrug-resistant Klebsiella pneumoniae via biofilm degradation. Front. Microbiol. 10, 2768 (2019).
Pridmore, A. C. et al. A lipopolysaccharide-deficient mutant of Neisseria meningitidis elicits attenuated cytokine release by human macrophages and signals via toll-like receptor (TLR) 2 but not via TLR4/MD2. J. Infect. Dis. 183, 89–96 (2001).
Wang, L. et al. Two-component response regulator OmpR regulates mucoviscosity through energy metabolism in Klebsiella pneumoniae. Microbiol. Spectr. https://doi.org/10.1128/spectrum.00544-23 (2023).
Cai, R. et al. Phage resistance mutation triggered by OmpC deficiency in Klebsiella pneumoniae induced limited fitness costs. Microb. Pathog. https://doi.org/10.1016/j.micpath.2022.105556 (2022).
Kobayashi, S. D. et al. Antibody-mediated killing of carbapenem-resistant ST258 Klebsiella pneumoniae by human neutrophils. mBio https://doi.org/10.1128/mBio.00297-18 (2018).
Stevenson, T. C. et al. Immunization with outer membrane vesicles displaying conserved surface polysaccharide antigen elicits broadly antimicrobial antibodies. Proc. Natl Acad. Sci. USA https://doi.org/10.1073/pnas.1718341115 (2018).
Chen, T. et al. The genome sequence archive family: Toward explosive data growth and diverse data types. Genom. Proteom. Bioinform. 19, 578–583 (2021).
CNCB-NGDC Members and Partners. Database resources of the National Genomics Data Center, China National Center for Bioinformation in 2022. Nucleic Acids Res. 50, D27–D38 (2022).
Acknowledgements
We gratefully acknowledge the contribution of the members of the CHINET group for collection of the isolates in this study. We thank the Electron Microscopy Imaging Laboratory in Shanghai Jiaotong University School of Medicine for helping with transmission electron microscopy imaging. We thank Y. Song at Shanghai Jiaotong University for helping with statistical analyses. We thank Y. Wang at China Agricultural University for sharing the plasmid pACYC184. We thank H. Ou at Shanghai Jiaotong University for sharing the plasmid pBAD33. This work was funded by the National Natural Science Foundation of China (grant number 81971896 (P.H.), 82172311 (F.H.), 32141002 (F.H.), 32170003 (Z.Z.) and 32370099 (Z.Z.)), the National Key Research and Development Project of China (2022YFA1304300) (P.H.), the China Antimicrobial Surveillance Network (Independent Medical Grants from Pfizer, 2018QD100) (F.H.) and Shanghai Antimicrobial Surveillance Network (3030231003) (F.H.).
Author information
Authors and Affiliations
Contributions
F.H., P.H. and Z.Z. conceived the study and wrote the manuscript. Y.P., R.H. and R.M. performed the experiments. H. Li and X.L. analysed the bioinformatics data. Y.W., H. Lun, X.Q., A.W., M.Z. and B.L. helped with experiments. J.L. helped with writing the manuscript. P.H. and Z.Z. supervised the project.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Microbiology thanks Otavio Raro and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1
Flowchart of data collection, and genotypic and phenotypic characterization of the CRKP isolates.
Extended Data Fig. 2 The root-to-tip distances and date randomisation tests for Lineage L1.implemented in the ACE function in the APE package.
a: A scatter plot generated by TempEst that shows linear regression of root-to-tip distances against isolation dates of the strains. The coefficient of determination (R2) and P-value is shown as well. The residual mean square was calculated using two-sided test. b, c: The date-randomisation tests based on the ‘True data’ and 10 datasets with the isolation dates of 1,756 samples randomly permutated. Data are presented as mean values ± SEM in part C. Significant greater R2 values of the root-to-tip tests were obtained from the true data than all the randomized data (B). And significantly greater substitution rates were also obtained based on the BactDating inferences (C).
Extended Data Fig. 3 Ancestral state reconstruction of L1 Lineage using the maximum likelihood (ML) algorithm implemented in the ACE function in the APE package.
The inferences were run based on three different models of (a) ER, which assumes equal transmission rates across all regions, (b) SYM, which assumes different, yet symmetric rates for transmissions between different pairs of regions, and (c) ARD, which is an all-rates-different model. Branches were colour-coded according to their most likely regional origins in the inferences (see keys). And the estimated possibility of the top region in certain major branches were shown nearby.
Extended Data Fig. 4 Capsule deficiency in KL47 and KL64 genotyped clinical isolates.
Quellung reaction of K. pneumoniae strains. K. pneumoniae strains were incubated with anti-K64 serum (or anti-K47 serum) or control serum as described in Methods. Compared with the control, the positive results showed capsular swelling under light microscopy with an oil immersion lens (magnification, 100). WT strains (KL64: 20–445, KL47: 18–81) and isogenic Δcps mutants showed Quellung reaction positive and negative, respectively. Quellung reaction of 20–445Δcps and 18–81Δcps was restored by complementation. Besides, Quellung reaction was restored by complementation with wcaJ or wbaP in a set of corresponding gene mutant clinical NEKp strains (KL64: 19–479, 19–501; KL47:16–30, 16–133). Each graph shows the representative result of three repetitions. The arrow points to the swollen capsule. Scale bar, 5 µm.
Extended Data Fig. 5 The mutation of capsule deletion rate in vitro culture.
The mutation of capsule deletion rate of KL64 and KL47 EKP isolates after 48 hours of culture in blood plate. Data are shown as the mean ± SEM. Each point represents the mean value of three biological replicates of one strain. For clarity, individual error bars for each strain are not shown.
Extended Data Fig. 6 Capsule of KL47 and KL64 K. pneumoniae does not impose a fitness cost in vitro.
In vitro competition assays were performed between KL47 strains (16–140, 18–404 and 19–249) and their isogenic Δcps mutants, and between KL64 strains (16–312 and 19–89) and their isogenic Δcps mutants. Bacteria were inoculated into LB broth at a ratio of 1:1 for 24 h at 37 °C, and WT and Δcps mutants were quantified by differential plating to calculate the competitive index (CI) value. Two-sided one-sample t-test was performed to compare the mean of CI to a hypothetical value of one (asterisk) for each group. Data represents the mean ( ± SEM) of three biological replicates. NS, no significance.
Extended Data Fig. 7 Effect of capsule deficiency on serum resistance and O antigen expression.
a: Serum killing assays were performed by incubating the parental EKp strains (twelve strains with different levels of serum resistance), KL64 capsular polysaccharide depolymerase (Dep41) or KL47 depolymerase (Dep42) pretreated parental EKp strains, the engineered isogenic Δcps strains with 75% baby rabbit serum for 1 hour at 37 °C. Percent survival was determined as the number of surviving bacteria relative to the initial bacterial addition. b: LPS was prepared by hot phenol-water method and analyzed by silver staining. The results of the serum killing assay showed that all capsule-stripped parental strains exhibited decreased serum resistance compared to that of untreated parental strains (except for those serum-sensitive strains that barely survived 1 hour post serum treatment) (A), demonstrating that K. pneumoniae capsules do play an important role in serum resistance. Six out of twelve isogenic Δcps mutants exhibited increased resistance to serum compared to the capsule-stripped parental strains (A). Increased amounts of OPS were observed in the isogenic Δcps mutants compared to the parental EKp strains (B). The remaining six isogenic Δcps mutants which showed no change in resistance to serum compared to the the depolymerase-treated parental strains, were all serum-sensitive strains with disruption of O antigen synthesis, as confirmed by LPS silver staining (B) and genome sequence analysis (A). N.D., rfb-locus mutation gene not detected in O− strain 16–140. Each point represents the mean value of three biological replicates. For clarity, individual error bars for each strain are not shown.
Extended Data Fig. 8 Investigation of the mechanism underlying the increased antiserum capacity of NEKp strains.
a: RNA sequencing and qRT-PCR of WT and Δcps strains. RNA sequencing heat map showing the differential expression of LPS and PG synthesis genes between EKp strain 16–312 and 16–312 Δcps mutant. qPCR assay was used to determine the relative mRNA levels of LPS and PG synthesis-related genes in 16–312 and 16–312 Δcps using the 2-ΔΔCT method. PG, peptidoglycan. Data represents the mean ( ± SEM) of three biological replicates of one strain. Unpaired two-sided Welch’s t-test was performed for statistical analysis. b: Effect of Und-P on serum resistance using either fosmidomycin to inhibit the Und-P de novo biosynthesis or ispU overexpression to increase the Und-P biosynthesis. Strains 16–312Δcps were grown in LB medium with or without FM (500 ng/ml); strains 16–312Δcps /ispU and 16–312Δcps/ EV were grown in LB medium with 10 mM arabinose. The serum killing assay was performed by incubating the strains with 75% baby rabbit complement for 1 hour at 37 °C. Percent survival was determined as the number of surviving bacteria relative to the initial bacterial addition. FM, fosmidomycin; EV, empty vector. Data represents the mean ( ± SEM) of four biological replicates of one strain. Unpaired two-sided Student’s t-test was performed for statistical analysis. Core-OS, core-oligosaccharide.
Extended Data Fig. 9 Identification of smooth and rough LPS in KL64O2a and KL47OL101 strains.
a: Phage SH-KpO2a (specific for O serotype O2a strains) and phage SH-KpOL101(specific for O serotype OL101 strains) can specifically infect and lyse corresponding O serotype non-capsulated K. pneumoniae strains with smooth LPS but not strains with rough LPS. Phage SH-KpO2a and SH-KPOL101 were isolated from sewage water using the host strain of K. pneumoniae 19–971 (KL64/O2a NEKp strain) and 19–253 (KL47/OL101 NEKp strain), respectively. Dep4115 and Dep4223 are specific depolymerases against K. pneumoniae KL64 and KL47 capsule, respectively. Spot assay results showed that phage SH-KpO2a and SH-KpOL101 formed the clear spot on the lawn of NEKp strain 19–971 and strain 19–253, respectively, while showed no spot on the lawn of their isogenic Δops mutants. LPS of the corresponding strains was prepared by hot phenol-water method and analyzed by silver staining (C). b: EKp strains of serotype O2a (16–312) and OL101(19–249) did not form lytic spots when infected with phage SH-KpO2a or SH-KpOL101 alone, whereas EKp strains pretreated with KL64 or KL47 depolymerase were susceptible to phage SH-KpO2a or SH-KpOL101, and formed clear spots (caused by phages) with haloes (caused by depolymerase) around. EKp isogenic Δops mutants pretreated with depolymerase were resistant to phage SH-KpO2a or SH-KpOL101, and formed translucent circles without clear spots. LPS of the corresponding strains was prepared by hot phenol-water method and analyzed by silver staining (C). d: LPS silver staining and phage spot assay of clinically isolated serotype KL64 O2a strains and serotype KL47 OL101 EKp strains. e: LPS silver stain and phage spot assay of clinical O− strains and complementary strains with ops. Each graph shows the representative result of three repetitions(A-E). Core-OS, core-oligosaccharide.
Extended Data Fig. 10 O antigen deficient strains in KL64 and KL47 strains.
a: O antigen of seventy NEKp strains and seventy selected paired EKp strains were detected by phage spot assay. KL64 and KL47 strains were infected with phage SH-KpO2a (with depolymerase Dep41) and SH-KpOL101 (with depolymerase Dep42), respectively. Strains that did not develop plaques were identified as O− strains. Some strains were further confirmed by LPS silver staining (see Supplementary Table 8 for details). n, indicates the number of CRKp strains. b: variants in rough LPS strains. Mutations found in the O2a and OL101 antigen biosynthesis genes in K. pneumoniae isolates (see Supplementary Table 8 for details). The black flag indicates the location of the mutation. Red, black and blue lines indicate ISs, SNPs and deletions, respectively. n, indicates the total number of mutations observed in that gene. c: The proportion of O− strains was estimated in 523 sequenced KL64 and KL47 strains. Strains with mutations in the rfb-locus were identified as O− strains. n, indicates the number of CRKp strains. d: Frequency of O− strains (526 KL64 and KL47 strains assessed by whole genome sequencing) isolated from different sites of infection. The number of strains in different infection sites is shown below. Pearson’s Chi-square test was used to analyze the proportion difference of O− strains strains in different infection samples. NS, no significance. e: Metagenomic analysis of rfb-locus variants in unprocessed clinical specimens (see Supplementary Table 10 for details).
Supplementary information
Supplementary Information
Supplementary Note.
Supplementary Table
Supplementary Table 1. CRKP patient characteristics. Supplementary Table 2. In vitro activities of agents against 1,017 CRKP strains. Supplementary Table 3. Frequency of carbapenemases of CRKP strains in 2016–2020. Supplementary Table 4. Frequency of capsular types of CRKP strain in 2016–2020. Supplementary Table 5. Distribution of resistant genes and mutations in KL64 and KL47 strains. Supplementary Table 6. Details of isolates used in the ST11 phylogeny analysis. Supplementary Table 7. K type, O type and geographical distribution of different clades in L1 lineage. Supplementary Table 8. Variation in phenotype and genotype of NEKp strains and selected paired EKp strains. Supplementary Table 9. The proportion of non-encapsulated strains in KL64 and KL47 CRKP isolates. Supplementary Table 10. cps-locus variants and rfb-locus variants in a clinical metagenomic specimen. Supplementary Table 11. Abbreviations in this paper. Supplementary Table 12. Primers used in this paper. Supplementary Table 13. Engineered mutants in this paper. Supplementary Table 14. Gene and gene products in this paper.
Source data
Source Data Fig. 4
Statistical source data for Fig. 4.
Source Data Fig. 5
Statistical source data for Fig. 5.
Source Data Fig. 6
Statistical source data for Fig. 6.
Source Data Fig. 6
Unprocessed gels for Fig. 6.
Source Data Extended Data Fig. 5
Statistical source data for Extended Data Fig. 5.
Source Data Extended Data Fig. 6
Statistical source data for Extended Data Fig. 6.
Source Data Extended Data Fig. 7
Statistical source data for Extended Data Fig. 7.
Source Data Extended Data Fig. 7
Unprocessed gels for Extended Data Fig. 7.
Source Data Extended Data Fig. 8
Statistical source data for Extended Data Fig. 8.
Source Data Extended Data Fig. 9
Unprocessed gels for Extended Data Fig. 9.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hu, F., Pan, Y., Li, H. et al. Carbapenem-resistant Klebsiella pneumoniae capsular types, antibiotic resistance and virulence factors in China: a longitudinal, multi-centre study. Nat Microbiol 9, 814–829 (2024). https://doi.org/10.1038/s41564-024-01612-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-024-01612-1