Abstract
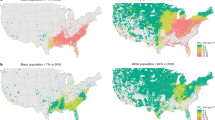
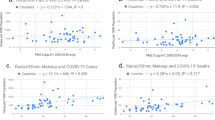
Average ambient fine particulate matter (PM2.5) concentrations have decreased in the US in recent years, but the health benefits of this improvement among different racial/ethnic groups are unknown. We estimate the associations between long-term exposure to ambient PM2.5 and cause-specific cardiovascular disease (CVD) mortality rate and assess the PM2.5-attributable CVD deaths by race/ethnicity across 3,103 US counties during 2001–2016 (n = 595,776 county-months). A 1 µg m−3 increase in PM2.5 concentration was associated with increases of 7.16 (95% confidence interval (CI): 3.81, 10.51) CVD deaths per 1,000,000 Black people per month, significantly higher than the estimates for non-Hispanic white people (1.76 (95% CI: 1.37, 2.15); difference in coefficients: 5.40 (95% CI: 2.03, 8.77), P = 0.001). No significant difference in this association was observed between Hispanic (2.66 (95% CI: −0.03, 5.35)) and non-Hispanic white people (difference in coefficients: 0.90 (95% CI: −1.81, 3.61), P = 0.523). From 2001 to 2016, the absolute disparity in PM2.5-attributable CVD mortality burden was reduced by 44.04% between non-Hispanic Black and white people and by 2.61% between Hispanic and non-Hispanic white people. However, in 2016, the burden remained 3.47 times higher for non-Hispanic Black people and 0.45 times higher for Hispanic people than for non-Hispanic white people. We call for policies that aim to reduce both exposure and vulnerability to PM2.5 for racial/ethnic minorities.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The monthly county-level cause-specific mortality data can be requested from the National Center for Health Statistics (https://www.cdc.gov/nchs/index.htm). Other data that support the findings of this study are available at https://zenodo.org/record/8121894 (https://doi.org/10.5281/zenodo.8121894)57.
Code availability
R code for this analysis is available at https://github.com/CHENlab-Yale/PM2.5_CVD_mortality_US.
References
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222 (2020).
Brunekreef, B. et al. Mortality and morbidity effects of long-term exposure to low-level PM2.5, BC, NO2, and O3: an analysis of European cohorts in the ELAPSE Project. HEI Report Series (2021).
Crouse, D. L. et al. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: a Canadian national-level cohort study. Environ. Health Perspect. 120, 708–714 (2012).
Brauer, M. et al. Mortality–Air Pollution Associations in Low-Exposure Environments (MAPLE): phase 2. HEI Report Series (2022).
Dominici, F. et al. Assessing adverse health effects of long-term exposure to low levels of ambient air pollution: implementation of causal inference methods. HEI Report Series (2022).
Di, Q. et al. An ensemble-based model of PM2.5 concentration across the contiguous United States with high spatiotemporal resolution. Environ. Int. 130, 104909 (2019).
Hubbell, B. J., Crume, R. V., Evarts, D. M. & Cohen, J. M. Policy monitor: regulation and progress under the 1990 Clean Air Act amendments. Rev. Environ. Econ. Policy 4, 122–138 (2010).
Fann, N., Coffman, E., Timin, B. & Kelly, J. T. The estimated change in the level and distribution of PM2.5-attributable health impacts in the United States: 2005–2014. Environ. Res. 167, 506–514 (2018).
Diderichsen, F., Hallqvist, J. & Whitehead, M. Differential vulnerability and susceptibility: how to make use of recent development in our understanding of mediation and interaction to tackle health inequalities. Int J. Epidemiol. 48, 268–274 (2019).
US Global Change Research Program. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment (USGCRP, 2016).
Liu, J. et al. Disparities in air pollution exposure in the United States by race/ethnicity and income, 1990–2010. Environ. Health Perspect. 129, 127005 (2021).
Tessum, C. W. et al. PM2.5 polluters disproportionately and systemically affect people of color in the United States. Sci. Adv. 7, eabf4491 (2021).
Jbaily, A. et al. Air pollution exposure disparities across US population and income groups. Nature 601, 228–233 (2022).
Hajat, A., Hsia, C. & O’Neill, M. S. Socioeconomic disparities and air pollution exposure: a global review. Curr. Environ. Health Rep. 2, 440–450 (2015).
Colmer, J., Hardman, I., Shimshack, J. & Voorheis, J. Disparities in PM2.5 air pollution in the United States. Science 369, 575–578 (2020).
Kravitz-Wirtz, N., Crowder, K., Hajat, A. & Sass, V. The long-term dynamics of racial/ethnic inequality in neighborhood air pollution exposure, 1990-2009. Du Bois Rev. 13, 237–259 (2016).
Wright, W. J. As above, so below: anti-Black violence as environmental racism. Antipode 53, 791–809 (2021).
Gottlieb, R. Forcing the Spring: the Transformation of the American Environmental Movement (Island Press, 2005).
Woo, B. et al. Residential segregation and racial/ethnic disparities in ambient air pollution. Race Soc. Probl. 11, 60–67 (2019).
Mascarenhas, M., Grattet, R. & Mege, K. Toxic waste and race in twenty-first century America: neighborhood poverty and racial composition in the siting of hazardous waste facilities. Environ. Soc. 12, 108–126 (2021).
Rigolon, A., Yañez, E., Aboelata, M. J. & Bennett, R. ‘A park is not just a park’: toward counter-narratives to advance equitable green space policy in the United States. Cities 128, 103792 (2022).
Rigolon, A., Browning, M. H., McAnirlin, O. & Yoon, H. Green space and health equity: a systematic review on the potential of green space to reduce health disparities. Int J. Environ. Res. Public Health 18, 2563 (2021).
Di, Q. et al. Air pollution and mortality in the Medicare population. N. Engl. J. Med. 376, 2513–2522 (2017).
Spiller, E., Proville, J., Roy, A. & Muller, N. Z. Mortality risk from PM2.5: a comparison of modeling approaches to identify disparities across racial/ethnic groups in policy outcomes. Environ. Health Perspect. 129, 127004 (2021).
Krieger, N. Discrimination and health inequities. Int J. Health Serv. 44, 643–710 (2014).
Bailey, Z. D. et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet 389, 1453–1463 (2017).
Williams, D. R. Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J. Health Soc. Behav. 59, 466–485 (2018).
Zang, E. & Kim, N. Intergenerational upward mobility and racial differences in mortality among young adults: evidence from county-level analyses. Health Place 70, 102628 (2021).
Seltenrich, N. The one-two-three punch: exposure, susceptibility, and disease burden among U.S. populations of color. Environ. Health Perspect. 130, 034001 (2022).
Van Horne, Y. O. et al. An applied environmental justice framework for exposure science. J. Expo. Sci. Environ. Epidemiol. https://doi.org/10.1038/s41370-022-00422-z (2022).
Renzi, M. et al. Long-term PM10 exposure and cause-specific mortality in the Latium region (Italy): a difference-in-differences approach. Environ. Health Perspect. 127, 067004 (2019).
Götschi, T. et al. Elemental composition and reflectance of ambient fine particles at 21 European locations. Atmos. Environ. 39, 5947–5958 (2005).
Atkinson, R. W., Mills, I. C., Walton, H. A. & Anderson, H. R. Fine particle components and health—a systematic review and meta-analysis of epidemiological time series studies of daily mortality and hospital admissions. J. Expo. Sci. Environ. Epidemiol. 25, 208–214 (2015).
Kapetanios, G., Pesaran, M. H. & Yamagata, T. Panels with non-stationary multifactor error structures. J. Econ. 160, 326–348 (2011).
Cartographic Boundary Files. United States Census Bureau https://www.census.gov/geographies/mapping-files/time-series/geo/cartographic-boundary.html (2019).
U.S. County Population Data – 1969–2020. The SEER Program https://seer.cancer.gov/popdata/ (2022).
Management, O. O. & Budget Revisions to the standards for the classification of federal data on race and ethnicity. Fed. Regist. 62, 58782–58790 (1997).
Khatana, S. A. M., Werner, R. M. & Groeneveld, P. W. Association of extreme heat and cardiovascular mortality in the United States: a county-level longitudinal analysis from 2008 to 2017. Circulation 146, 249–261 (2022).
Turner, M. C. et al. Long-term ozone exposure and mortality in a large prospective study. Am. J. Respir. Crit. Care Med 193, 1134–1142 (2016).
Pope, C. A. 3rd et al. Relationships between fine particulate air pollution, cardiometabolic disorders, and cardiovascular mortality. Circ. Res. 116, 108–115 (2015).
Di, Q. et al. Daily and annual PM2.5 concentrations for the contiguous United States, 1-km grids, v1 (2000–2016). NASA Socioeconomic Data and Applications Center. (NASA, Accessed 16 August 2022); https://doi.org/10.7927/0rvr-4538
Wei, Y. et al. Causal effects of air pollution on mortality rate in Massachusetts. Am. J. Epidemiol. 189, 1316–1323 (2020).
Di, Q. et al. Assessing NO2 concentration and model uncertainty with high spatiotemporal resolution across the contiguous United States. Environ. Sci. Technol. 54, 1372–1384 (2019).
Di, Q. et al. Daily and annual NO2 concentrations for the contiguous United States, 1-km grids, v1 (2000–2016). NASA Socioeconomic Data and Applications Center. (NASA, Accessed 16 August 2022); https://doi.org/10.7927/f8eh-5864
Requia, W. J. et al. An ensemble learning approach for estimating high spatiotemporal resolution of ground-level ozone in the contiguous U.S. Environ. Sci. Technol. 54, 11037–11047 (2020).
Requia, W. J. et al. Daily 8-hour maximum and annual O3 concentrations for the contiguous United States, 1-km grids, v1 (2000–2016). NASA Socioeconomic Data and Applications Center. (NASA, Accessed 16 August 2022); https://doi.org/10.7927/a4mb-4t86
PRISM Climate Group. PRISM Climate Data Recent Years (Jan 1981–Jan 2022) (2016).
Bai, J. Panel data models with interactive fixed effects. Econometrica 77, 1229–1279 (2009).
Goodman-Bacon, A. Difference-in-differences with variation in treatment timing. J. Econ. 225, 254–277 (2021).
Liu, L., Wang, Y. & Xu, Y. A practical guide to counterfactual estimators for causal inference with time-series cross-sectional data. Am. J. Pol. Sci. https://doi.org/10.1111/ajps.12723 (2022).
Xu, Y. Generalized synthetic control method: causal inference with interactive fixed effects models. Polit. Anal. 25, 57–76 (2017).
Bai, J. & Ng, S. Determining the number of factors in approximate factor models. Econometrica 70, 191–221 (2002).
Bada, O. & Liebl, D. phtt: panel data analysis with heterogeneous time trends in R. J. Stat. Softw. 59, 1–33 (2014).
NCHS Urban-Rural Classification Scheme for Counties. National Center for Health Statistics https://www.cdc.gov/nchs/data_access/urban_rural.htm (2017).
Chen, K. et al. Triggering of myocardial infarction by heat exposure is modified by medication intake. Nat. Cardiovasc Res 1, 727–731 (2022).
Benshaul-Tolonen, A. Local industrial shocks and infant mortality. Econ. J. 129, 1561–1592 (2019).
Ma, Y. et al. CHENlab-Yale/PM2.5_CVD_mortality_US: first release of the repository for PM2.5_CVD_mortality_US project. Zenodo https://doi.org/10.5281/zenodo.8121894 (2023).
Acknowledgements
E.Z. received support from the National Institute on Aging (R21AG074238-01, E.Z.), the National Institute on Minority Health and Health Disparities (1R01MD017298-01, E.Z.), the Research Education Core of the Claude D. Pepper Older Americans Independence Center at Yale School of Medicine (P30AG021342, E.Z.) and the Institution for Social and Policy Studies at Yale University. I.O. received support from the National Institutes on Health Director’s Early Independence Award (DP5OD029636, I.O.). Research reported in this publication was supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number R01MD016054 (K.C.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Y.M. conducted formal analyses and drafted the manuscript. K.C. conceived of and supervised the conduct of this study and edited the manuscript. E.Z. applied and managed the mortality dataset, supervised the statistical analysis and revised the manuscript. I.O. contributed to the writing and manuscript revision. Y.L. and H.K. contributed to the interpretation of results and manuscript revision. All authors reviewed and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Human Behaviour thanks Sebhat Erqou, Srinivasa Katikireddi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Methods 1–3, Figs.1–9, Tables 1–7 and References.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ma, Y., Zang, E., Opara, I. et al. Racial/ethnic disparities in PM2.5-attributable cardiovascular mortality burden in the United States. Nat Hum Behav 7, 2074–2083 (2023). https://doi.org/10.1038/s41562-023-01694-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41562-023-01694-7
This article is cited by
-
Racial disparities in air pollution
Nature Human Behaviour (2023)