Abstract
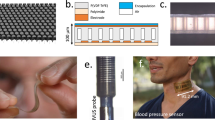
The high stiffness of intravenous needles can cause tissue injury and increase the risk of transmission of blood-borne pathogens through accidental needlesticks. Here we describe the development and performance of an intravenous needle whose stiffness and shape depend on body temperature. The needle is sufficiently stiff for insertion into soft tissue yet becomes irreversibly flexible after insertion, adapting to the shape of the blood vessel and reducing the risk of needlestick injury on removal, as we show in vein phantoms and ex vivo porcine tissue. In mice, the needles had similar fluid-delivery performance and caused substantially less inflammation than commercial devices for intravenous access of similar size. We also show that an intravenous needle integrated with a thin-film temperature sensor can monitor core body temperature in mice and detect fluid leakage in porcine tissue ex vivo. Temperature-responsive intravenous needles may improve patient care.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The main data supporting the results in this study are available within the paper and its Supplementary Information. The raw and analysed datasets generated during the study are available for research purposes from the corresponding authors on reasonable request. Source data for the figures are provided with this paper.
References
Boras, B. et al. Preclinical characterization of an intravenous coronavirus 3CL protease inhibitor for the potential treatment of COVID19. Nat. Commun. 12, 6055 (2021).
Ma, F. et al. Neurotransmitter-derived lipidoids (NT-lipidoids) for enhanced brain delivery through intravenous injection. Sci. Adv. 6, eabb4429 (2020).
FDA approves first treatment for COVID-19. US Food and Drug Administration https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-covid-19 (2020).
Wei, F., Chen, W. & Lin, X. A clinical rule for the difficulty prediction on scalp intravenous access in infants (SIAI) from emergency room. Sci. Rep. 10, 6624 (2020).
Finfer, S., Myburgh, J. & Bellomo, R. Intravenous fluid therapy in critically ill adults. Nat. Rev. Nephrol. 14, 541–557 (2018).
Samson, A. et al. Intravenous delivery of oncolytic reovirus to brain tumor patients immunologically primes for subsequent checkpoint blockade. Sci. Transl. Med. 10, eaam7577 (2018).
Zingg, W. & Pittet, D. Peripheral venous catheters: an under-evaluated problem. Int. J. Antimicrob. Agents 34, S38–S42 (2009).
Rickard, C. M., McCann, D., Munnings, J. & McGrail, M. R. Routine resite of peripheral intravenous devices every 3 days did not reduce complications compared with clinically indicated resite: a randomised controlled trial. BMC Med. 8, 53 (2010).
Jin, J. et al. The optimal choice of medication administration route regarding intravenous, intramuscular, and subcutaneous injection. Patient Prefer. Adherence 9, 923–942 (2015).
Malach, T. et al. Prospective surveillance of phlebitis associated with peripheral intravenous catheters. Am. J. Infect. Control 34, 308–312 (2006).
Duffy, B. L. & Lee, J. S. Intravenous access: a comparison of two methods. Anaesth. Intensive Care 11, 135–137 (1983).
Weiss, D., Yaakobovitch, H., Tal, S., Nyska, A. & Rotman, O. M. Novel short peripheral catheter design for prevention of thrombophlebitis. J. Thromb. Haemost. 17, 39–51 (2019).
Abolfotouh, M. A., Salam, M., Bani-Mustafa, A., White, D. & Balkhy, H. H. Prospective study of incidence and predictors of peripheral intravenous catheter-induced complications. Ther. Clin. Risk Manag. 10, 993–1001 (2014).
Miliani, K. et al. Peripheral venous catheter-related adverse events: evaluation from a multicentre epidemiological study in France (the CATHEVAL Project). PLoS ONE 12, e0168637 (2017).
Kim, J. T., Park, J. Y., Lee, H. J. & Cheon, Y. J. Guidelines for the management of extravasation. J. Educ. Eval. Health Prof. 17, 21 (2020).
Al-Benna, S., O’Boyle, C. & Holley, J. Extravasation injuries in adults. ISRN Dermatol. 2013, 856541 (2013).
Webster, J., Osborne, S., Rickard, C. M. & Marsh, N. Clinically‐indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst. Rev. 2019, CD007798 (2019).
Alexandrou, E. et al. International prevalence of the use of peripheral intravenous catheters. J. Hosp. Med. 10, 530–533 (2015).
Wallis, M. C. et al. Risk factors for peripheral intravenous catheter failure: a multivariate analysis of data from a randomized controlled trial. Infect. Control Hosp. Epidemiol. 35, 63–68 (2014).
Weber, P. W. et al. Modifying peripheral IV catheters with side holes and side slits results in favorable changes in fluid dynamic properties during the injection of iodinated contrast material. AJR Am. J. Roentgenol. 193, 970–977 (2009).
Xu, Y. et al. Hydrogel-coated needles prevent puncture site bleeding in arteriovenous fistula and arteriovenous grafts in rats. Biomed. Pharmacother. 143, 112113 (2021).
Yu, H. et al. Water-insoluble polymeric guanidine derivative and application in the preparation of antibacterial coating of catheter. ACS Appl. Mater. Interfaces 10, 39257–39267 (2018).
Travessa, D., Ferrante, M. & den Ouden, G. Diffusion bonding of aluminium oxide to stainless steel using stress relief interlayers. Mater. Sci. Eng. A 337, 287–296 (2002).
Phua, S. L. et al. Reinforcement of polyether polyurethane with dopamine-modified clay: the role of interfacial hydrogen bonding. ACS Appl. Mater. Interfaces 4, 4571–4578 (2012).
Ebnesajjad, S. in Fluoroplastics 2nd edn, Vol. 2 (ed Ebnesajjad, S.) 216–235 https://doi.org/10.1016/B978-1-4557-3197-8.00009-2 (William Andrew Publishing, 2015).
Li, C., Guan, G., Reif, R., Huang, Z. & Wang, R. K. Determining elastic properties of skin by measuring surface waves from an impulse mechanical stimulus using phase-sensitive optical coherence tomography. J. R. Soc. Interface 9, 831–841 (2012).
Alfulayw, K. H., Al-Otaibi, S. T. & Alqahtani, H. A. Factors associated with needlestick injuries among healthcare workers: implications for prevention. BMC Health Serv. Res. 21, 1074 (2021).
Beltrami, E. M., Williams, I. T., Shapiro, C. N. & Chamberland, M. E. Risk and management of blood-borne infections in health care workers. Clin. Microbiol. Rev. 13, 385–407 (2000).
Khan Afridi, A. A., Kumar, A. & Sayani, R. Needle stick injuries—risk and preventive factors: a study among health care workers in tertiary care hospitals in Pakistan. Glob. J. Health Sci. 5, 85–92 (2013).
Schuurmans, J., Lutgens, S. P., Groen, L. & Schneeberger, P. M. Do safety engineered devices reduce needlestick injuries? J. Hosp. Infect. 100, 99–104 (2018).
WHO Guideline on the Use of Safety-Engineered Syringes for Intramuscular, Intradermal and Subcutaneous Injections in Health Care Settings (World Health Organization, 2016).
Harb, A. C. et al. Safety engineered injection devices for intramuscular, subcutaneous and intradermal injections in healthcare delivery settings: a systematic review and meta-analysis. BMC Nurs. 14, 71 (2015).
Byun, S.-H., Sim, J. Y., Agno, K.-C. & Jeong, J.-W. Materials and manufacturing strategies for mechanically transformative electronics. Mater. Today Adv. 7, 100089 (2020).
Byun, S.-H. et al. Mechanically transformative electronics, sensors, and implantable devices. Sci. Adv. 5, eaay0418 (2019).
Lin, Y., Genzer, J. & Dickey, M. D. Attributes, fabrication, and applications of gallium-based liquid metal particles. Adv. Sci. 7, 2000192 (2020).
Elbourne, A. et al. Antibacterial liquid metals: biofilm treatment via magnetic activation. ACS Nano 14, 802–817 (2020).
Lu, Y. et al. Transformable liquid-metal nanomedicine. Nat. Commun. 6, 10066 (2015).
Chen, M. et al. Self-powered multifunctional sensing based on super-elastic fibers by soluble-core thermal drawing. Nat. Commun. 12, 1416 (2021).
Yan, W. et al. Thermally drawn advanced functional fibers: new frontier of flexible electronics. Mater. Today 35, 168–194 (2020).
Qu, Y. et al. Superelastic multimaterial electronic and photonic fibers and devices via thermal drawing. Adv. Mater. 30, 1707251 (2018).
Wen, X. et al. Flexible, multifunctional neural probe with liquid metal enabled, ultra-large tunable stiffness for deep-brain chemical sensing and agent delivery. Biosens. Bioelectron. 131, 37–45 (2019).
Ebrahimi, A. P. Mechanical properties of normal and diseased cerebrovascular system. J. Vasc. Interv. Neurol. 2, 155–162 (2009).
Bai, M.-Y., Chang, Y.-C. & Chu, J. P. Preclinical studies of non-stick thin film metallic glass-coated syringe needles. Sci. Rep. 10, 20313 (2020).
Hauzenberger, J. R. et al. Systematic in vivo evaluation of the time-dependent inflammatory response to steel and Teflon insulin infusion catheters. Sci. Rep. 8, 1132 (2018).
Jeong, J.-W. et al. Wireless optofluidic systems for programmable in vivo pharmacology and optogenetics. Cell 162, 662–674 (2015).
I. Mechanical properties of catheters. Acta Radiol. Diagn. 4, 11–22 https://doi.org/10.1080/05678066609170493 (1966).
Makvandi, P. et al. Engineering microneedle patches for improved penetration: analysis, skin models and factors affecting needle insertion. Nanomicro. Lett. 13, 93 (2021).
Kataoka, H. et al. Measurement of the tip and friction force acting on a needle during penetration. In Proc. 5th Medical Image Computing and Computer-Assisted Intervention (MICCAI 2002) (eds Dohi, T. & Kikinis, R.) 216–223 (Springer, 2002).
Elastosil RT 623 A/B datasheet version 1.3 (Wacker Chemie, 2014).
Sylgard 184 silicone elastomer datasheet reference number 10-1204A-01 (Dow Corning, 1998).
Summerfield, A., Meurens, F. & Ricklin, M. E. The immunology of the porcine skin and its value as a model for human skin. Mol. Immunol. 66, 14–21 (2015).
Chitnis, G. D. et al. A resistance-sensing mechanical injector for the precise delivery of liquids to target tissue. Nat. Biomed. Eng. 3, 621–631 (2019).
Yu, Y. et al. Biocompatibility and in vivo operation of implantable mesoporous PVDF-based nanogenerators. Nano Energy 27, 275–281 (2016).
KoreaVaccine catalogue (KoreaVaccine, 2016).
Nathwani, R. A., Pais, S., Reynolds, T. B. & Kaplowitz, N. Serum alanine aminotransferase in skeletal muscle diseases. Hepatology 41, 380–382 (2005).
Mazzaccara, C. et al. Age-related reference intervals of the main biochemical and hematological parameters in C57BL/6J, 129SV/EV and C3H/HeJ mouse strains. PLoS ONE 3, e3772 (2008).
Harrison, S. D. Jr, Burdeshaw, J. A., Crosby, R. G., Cusic, A. M. & Denine, E. P. Hematology and clinical chemistry reference values for C57BL/6 X DBA/2 F1 mice. Cancer Res. 38, 2636–2639 (1978).
Haney, E. M. et al. in Screening for Lipid Disorders in Children and Adolescents (Agency for Healthcare Research and Quality (US), 2007).
Guo, H. et al. Advanced materials in wireless, implantable electrical stimulators that offer rapid rates of bioresorption for peripheral axon regeneration. Adv. Funct. Mater. 31, 2102724 (2021).
Kim, B. J. & Meng, E. Micromachining of parylene C for bioMEMS. Polym. Adv. Technol. 27, 564–576 (2016).
Gordon, C. J. The mouse thermoregulatory system: its impact on translating biomedical data to humans. Physiol. Behav. 179, 55–66 (2017).
Choi, W.-M. et al. Experimental applications of in situ liver perfusion machinery for the study of liver disease. Mol. Cells 42, 45–55 (2019).
Li, X. F. et al. Size–temperature phase diagram of gallium. EPL 94, 16001 (2011).
Fink, E. L., Kochanek, P. M., Clark, R. S. B. & Bell, M. J. Fever control and application of hypothermia using intravenous cold saline. Pediatr. Crit. Care Med. 13, 80–84 (2012).
Obořilová, A., Mayer, J., Pospı́šil, Z. & Kořı́stek, Z. Symptomatic intravenous antipyretic therapy: efficacy of metamizol, diclofenac, and propacetamol. J. Pain Symptom Manage. 24, 608–615 (2002).
Schell-Chaple, H. M., Liu, K. D., Matthay, M. A., Sessler, D. I. & Puntillo, K. A. Effects of IV acetaminophen on core body temperature and hemodynamic responses in febrile critically ill adults: a randomized controlled trial. Crit. Care Med. 45, 1199–1207 (2017).
Richmond, V. L., Davey, S., Griggs, K. & Havenith, G. Prediction of core body temperature from multiple variables. Ann. Occup. Hyg. 59, 1168–1178 (2015).
Sessler, D. I., Warner, D. S. & Warner, M. A. Temperature monitoring and perioperative thermoregulation. Anesthesiology 109, 318–338 (2008).
Moons, C. P., Hermans, K., Remie, R., Duchateau, L. & Odberg, F. Intraperitoneal versus subcutaneous telemetry devices in young Mongolian gerbils (Meriones unguiculatus). Lab. Anim. 41, 262–269 (2007).
Lim, R., Damalerio, R. B., Bong, C. L., Tan, S. K. & Cheng, M.-Y. Novel conformal skin patch with embedded thin-film electrodes for early detection of extravasation. Sensors 21, 3429 (2021).
Bicen, A. O., West, L. L., Cesar, L. & Inan, O. T. Toward non-invasive and automatic intravenous infiltration detection: evaluation of bioimpedance and skin strain in a pig model. IEEE J. Transl. Eng. Health Med. 6, 4100207 (2018).
Shekalim, A. Method and device for detecting extravasation. US patent 6,425,878 B1 (2002).
Ross, P. A., Lerman, J. & Coté, C. J. in A Practice of Anesthesia for Infants and Children 6th edn (eds Coté, C. J. et al.) 1175–1203.e8 https://doi.org/10.1016/B978-0-323-42974-0.00052-5 (Elsevier, 2019).
ANSI/ASHRAE/ASHE Addendum A to ANSI/ASHRAE/ASHE Standard 170-2017 Ventilation of Healthcare Facilities (ASHRAE, 2020).
ISO 10993-1:2018 Biological Evaluation of Medical Devices—Part 1: Evaluation and Testing within a Risk Management Process (International Organization for Standardization, 2018).
Samant, P. P. & Prausnitz, M. R. Mechanisms of sampling interstitial fluid from skin using a microneedle patch. Proc. Natl Acad. Sci. USA 115, 4583–4588 (2018).
Liu, Y. et al. Morphing electronics enable neuromodulation in growing tissue. Nat. Biotechnol. 38, 1031–1036 (2020).
Sunwoo, S. H. et al. Chronic and acute stress monitoring by electrophysiological signals from adrenal gland. Proc. Natl Acad. Sci. USA 116, 1146–1151 (2019).
Reeder, J. et al. Mechanically adaptive organic transistors for implantable electronics. Adv. Mater. 26, 4967–4973 (2014).
Gupta, S. & Madoff, D. C. Image-guided percutaneous needle biopsy in cancer diagnosis and staging. Tech. Vasc. Interv. Radiol. 10, 88–101 (2007).
Marticorena, R. M. & Donnelly, S. M. Impact of needles in vascular access for hemodialysis. J. Vasc. Access 17, S32–S37 (2016).
Series safety data sheet SDS no. 823A (Smooth-On, 2023); https://www.smooth-on.com/msds/files/BD_DS_Eco_Equ_EZB_EZS_Psy_MS_OOMOO_Reb_ST_SS_Soma_Sol_Sorta.pdf
Stingl, J. et al. Morphology and some biomechanical properties of human liver and spleen. Surg. Radiol. Anat. 24, 285–289 (2002).
Karimi, A., Shojaei, A. & Tehrani, P. Measurement of the mechanical properties of the human gallbladder. J. Med. Eng. Technol. 41, 541–545 (2017).
Mattei, G. & Ahluwalia, A. Sample, testing and analysis variables affecting liver mechanical properties: a review. Acta Biomater. 45, 60–71 (2016).
Karimi, A. & Shojaei, A. Measurement of the mechanical properties of the human kidney. IRBM 38, 292–297 (2017).
Dahms, Piechota, Dahiya, Lue & Tanagho Composition and biomechanical properties of the bladder acellular matrix graft: comparative analysis in rat, pig and human. Br. J. Urol. 82, 411–419 (1998).
Egorov, V. I., Schastlivtsev, I. V., Prut, E. V., Baranov, A. O. & Turusov, R. A. Mechanical properties of the human gastrointestinal tract. J. Biomech. 35, 1417–1425 (2002).
Byun, S.-H. et al. Design strategy for transformative electronic system toward rapid, bidirectional stiffness tuning using graphene and flexible thermoelectric device interfaces. Adv. Mater. 33, 2007239 (2021).
Li, C., Huang, Z. & Wang, R. K. Elastic properties of soft tissue-mimicking phantoms assessed by combined use of laser ultrasonics and low coherence interferometry. Opt. Express 19, 10153–10163 (2011).
Kobayashi, Y. et al. Use of puncture force measurement to investigate the conditions of blood vessel needle insertion. Med. Eng. Phys. 35, 684–689 (2013).
Kalidasan, V. et al. Wirelessly operated bioelectronic sutures for the monitoring of deep surgical wounds. Nat. Biomed. Eng. 5, 1217–1227 (2021).
Nagle, R., Schreiber, K. & Said, T. An evaluation of the effect of a kinked cannula on intravenous cannula flow rates. Bahrain Med. Bull. 37, 175–177 (2015).
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (NRF-2021R1A2C4001483 and NRF-2020M3C1B8A01111568 to J.-W.J.; NRF-2021R1A2C3004589 to W.-I.J.).
Author information
Authors and Affiliations
Contributions
K.-C.A. and J.-W.J. conceptualized the project and designed the experiments for overall technology development. K.-C.A., S.-H.B., S.O., S.L., H.K. and S.C. fabricated and prepared the devices, discussed conceptual illustration, and captured the photographs for proof-of-concept demonstration and set-up. K.Y., K.K. and W.-I.J. designed and performed the experiments, collected data and analysed results in the in vivo biocompatibility and fluid-delivery tests. K.-C.A. and K.Y. performed the in vivo temperature sensing under the supervision of W.-I.J. and J.-W.J. K.-C.A., K.Y., W.-I.J. and J.-W.J. performed the investigation, analysed the data and wrote the results. K.-C.A. and J.-W.J. were responsible for conceptual drawings and data representation. K.-C.A., K.Y., W.-I.J. and J.-W.J. wrote the article. W.-I.J. and J.-W.J. acquired funding and supervised the project. W.-I.J. and J.-W.J. are co-senior authors. All authors discussed the results and contributed to revision of the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Biomedical Engineering thanks Giuseppe Barillaro, Eoin O’Cearbhaill and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
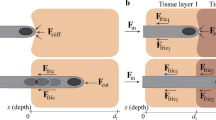
Extended Data Fig. 1 Stiffness- and shape-integrity of P-CARE needle under warm temperature.
a, Image of the temperature-controlled experimental set-up in cross section view. b, Plot of time before the needle becomes soft at various temperatures. The plot legends are as follows: blue, the needle is inside the polystyrene box with icepacks; grey, the needle is taken out from the polystyrene box without icepacks; red, the needle is taken out from the polystyrene box with icepacks. The inset shows the magnified plots for the softening time at indicated outside temperatures. Data are presented as mean values ± SD (n = 3 samples). c, Images showing the physical condition of the needle inside the polystyrene box with icepacks, externally heated to 50 °C, (left) needle inside the polystyrene box before heating, (middle) needle inside the polystyrene after 10 hrs of heating on a hotplate (50 °C) in a closed chamber, (right) needle taken out from the insulated box with icepack after 10 hrs of heating at 50 °C. Scale bar, 1 cm. d, Images of the integrated pig skin-transparent multi-layer tissue phantom with artificial vein setup, (left) side view image of the skin-multi-layer transparent tissue phantom, (left, inset) actual image of porcine skin showing small superficial veins in an upside-down view, ~1.5 mm thickness, (right) schematic illustration of integrated pig skin-transparent multi-layer tissue phantom created by using PDMS-oil (10:1 by weight), 13 mm total thickness. Scale bar, 1 cm. e, Images of the rigid insertion of the needle into porcine skin followed by fluid delivery into a customized vein-transparent tissue phantom with an external temperature of 35 °C, highlighting that a rigid insertion through pig skin using P-CARE needle is possible. Scale bars, 5 mm.
Extended Data Fig. 2 P-CARE needle after insertion and fluid delivery.
a, Image after retracting the softened P-CARE needle from tissue phantom, demonstrating a gravity-bent and completely softened needle after use for an advance safe-handling needle disposal. b, Plot of thermal response during the freezing process of the softened P-CARE needle after usage (that is, rigid insertion). The solidification of the softened needle occurs when the needle was exposed to temperature of −5 °C. At this temperature, it takes about 29.45 s for the gallium needle to solidify (tc), verifying that the softened needle after use (that is, withdrawn from the soft tissue after rigid insertion) will indefinitely exhibit a low modulus of elasticity when use at a healthcare facility (20–24 °C), making the needle completely non-reusable after first usage.
Extended Data Fig. 3 Characterization of nanomembrane temperature sensor integrated in P-CARE needle.
a, Relative resistance change as a function of temperature, showing that the phase state of P-CARE needle (rigid or soft) has no significant effect on the sensing performance (Tambient= 20 °C) within physiological temperature range (30 to 42 °C). Note that the same sample was measured repeatedly (n = 3 trials). b, Relative resistance change as a function of time, exhibiting that the encapsulated P-CARE needle sensor has a comparable thermal response time (~9 s) with the one of an encapsulation-free thin-film sensor of the same design when immersed in the same medium (Tmedium= 37 °C, Tambient= 25 °C). The slight difference between sensor output is attributed to the polymeric encapsulation of the device. c, Relative resistance change as a function of time of P-CARE needle immersed in a medium of varying temperature (30, 37 and 50 °C). d, Relative resistance change as a function of increasing or decreasing medium temperature, demonstrating no significant device hysteresis within physiological temperature range. Note that the same sample was measured repeatedly (n = 3 trials). e, Plot of sensor output as a function of radius of curvature, indicating electrical stability during bending. f, Relative resistance change as a function of insertion depth into a medium with constant temperature. The result exhibits that the sensor output is independent of insertion depth as needle advances deeper (75% of total needle length is immersed, which is similar to the conventional practice in IV needle placement in a healthcare setting) into a temperature-controlled environment (Tmedium = 36 °C; Tambient = 24 °C; θ = ~ 30°). Error bars show the mean ± standard deviation (n = 3 samples).
Supplementary information
Supplementary Information
Supplementary figures, tables and references.
Source data
Source Data Fig. 2
Source data.
Source Data Fig. 3
Source data.
Source Data Fig. 4
Source data.
Source Data Fig. 5
Source data.
Source Data Extended Data Fig. 1
Source data.
Source Data Extended Data Fig. 2
Source data.
Source Data Extended Data Fig. 3
Source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Agno, KC., Yang, K., Byun, SH. et al. A temperature-responsive intravenous needle that irreversibly softens on insertion. Nat. Biomed. Eng (2023). https://doi.org/10.1038/s41551-023-01116-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41551-023-01116-z
This article is cited by
-
A needle that softens on intravenous insertion
Nature Biomedical Engineering (2023)
-
A study on the fabrication of metal microneedle array electrodes for ECG detection based on low melting point Bi–In–Sn alloys
Scientific Reports (2023)