Abstract
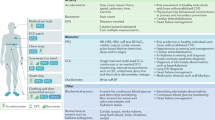
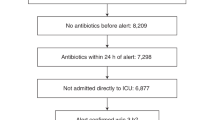
Point-of-care sensors that enable the fast collection of information relevant to a patient’s health state can facilitate improved health access, reduce healthcare costs and improve the quality of healthcare delivery. In the diagnosis of sepsis — defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection, and the leading cause of in-patient death and of hospital readmission in the United States — predicting which infections will lead to life-threatening organ dysfunction and developing specific anti-sepsis treatments remain challenging because of the significant heterogeneity of the host response. Yet the use of point-of-care devices could reduce the time from the onset of a patient’s infection to the administration of appropriate therapeutics. In this Perspective, we describe the current state of point-of-care sensors for the diagnosis and monitoring of sepsis, and outline opportunities in the use of these devices to dramatically improve patient care.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Fleischmann, C. et al. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am. J. Respir. Crit. Care Med. 193, 259–272 (2016).
Fleischmann, C. et al. The global burden of pediatric and neonatal sepsis: a systematic review. Lancet Respir. Med. 6, 223–230 (2018).
Van Dillen, J. et al. Maternal sepsis: epidemiology, etiology and outcome. Curr. Opin. Infect. Dis. 23, 249–254 (2010).
Lagu, T. et al. Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Crit. Care Med. 40, 754–761 (2012).
Gaieski, D. F., Edwards, M., Kallan, K. J. & Carr, B. J. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit. Care Med. 41, 1167–1174 (2013).
Seymour, C. W. et al. Time to treatment and mortality during mandated emergency care for sepsis. N. Engl. J. Med. 376, 2235–2244 (2017).
Alam, N. et al. Prehospital antibiotics in the ambulance for sepsis: a multicentre, open label, randomised trial. Lancet Respir. Med. 6, 40–50 (2018).
Gander, R. M. et al. Impact of blood cultures drawn by phlebotomy on contamination rates and health care costs in a hospital emergency department. J. Clin. Microbiol. 47, 1021–1024 (2009).
Sitdikov, R. A. et al. Target capture system. US patent 9599610 (2014).
Puttaswamy, S., Lee, B. D. & Sengupta, S. Novel electrical method for early detection of viable bacteria in blood cultures. J. Clin. Microbiol. 49, 2286–2289 (2011).
Sengupta, S., Puttaswamy, S. & Chang, H. C. Rapid detection of viable bacteria system and method. US patent 8,635,028 (2014).
FAST technology. Qvella Corporation https://www.qvella.com/technology (2018).
LiDia. DNA Electronics http://www.dnae.com/lidia.html (2018).
Accelerate Pheno system. Accelerate Diagnostics http://acceleratediagnostics.com/products/accelerate-pheno-system/#features (2018).
Niemz, A., Ferguson, T. M. & Boyle, D. S. Point-of-care nucleic acid testing for infectious diseases. Trends Biotechnol. 29, 240–250 (2011).
Singer, M. et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315, 801–810 (2016).
BioMérieux 510(k) Substantial Equivalence Determination Decision Memorandum K162827, VIDAS B·R·A·H·M·S PCT clearance submission to FDA (FDA, 2017).
Faix, J. D. Biomarkers of sepsis. Crit. Rev. Clin. Lab. Sci. 50, 23–36 (2013).
de Jong, E., van Oers, J. A., Beishuizen, A., Vos, P. & Vermeijden, W. J. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect. Dis. 16, 819–827 (2016).
Pierrakos, C. & Vincent, J. L. Sepsis biomarkers: a review. Crit. Care 14, R15 (2010).
Kibe, S., Adams, K. & Barlow, G. Diagnostic and prognostic biomarkers of sepsis in critical care. J. Antimicrob. Chemother. 66, ii33–ii40 (2010).
Schuetz, P. et al. Effect of procalcitonin-guided antibiotic treatment on mortality in acute respiratory infections: a patient level meta-analysis. Lancet Infect. Dis. 18, 95–107 (2018).
Huang, D. T. et al. Procalcitonin-guided use of antibiotics for lower respiratory tract infection. N. Engl. J. Med. 379, 236–249 (2018).
Shapiro, N. I. et al. A prospective, multicenter derivation of a biomarker panel to assess risk of organ dysfunction, shock, and death in emergency department patients with suspected sepsis. Crit. Care Med. 37, 96–104 (2009).
Paulus, P., Jennewein, C. & Zacharowski, K. Biomarkers of endothelial dysfunction: can they help us deciphering systemic inflammation and sepsis? Biomarkers 16, S11–S21 (2011).
Angus, D. C. & Poll, T. Sepsis and septic shock. N. Engl. J. Med. 369, 840–851 (2013).
Hotchkiss, R. S. et al. Sepsis and septic shock. Nat. Rev. Dis. Primers 2, 16045 (2016).
Poll, T. V. D., van de Veerdonk, F. L., Scicluna, B. P. & Netea, M. G. The immunopathology of sepsis and potential therapeutic targets. Nat. Rev. Immunol. 17, 407–420 (2017).
Chauhan, N., Tiwari, S. & Jain, U. Potential biomarkers for effective screening of neonatal sepsis infections: an overview. Microb. Pathog. 107, 234–242 (2017).
Kolaczkowska, E. & Kubes, P. Neutrophil recruitment and function in health and inflammation. Nat. Rev. Immunol. 13, 159–175 (2013).
Seymour, C. W. et al. Delays from first medical contact to antibiotic administration for sepsis. Crit. Care Med. 45, 759–765 (2017).
Pitt, W. G. et al. Rapid separation of bacteria from blood — review and outlook. Biotechnol. Prog. 32, 823–839 (2016).
Mutlu, B. R. et al. Non-equilibrium inertial separation array for high-throughput, large-volume blood fractionation. Sci. Rep. 7, 9915 (2017).
Fachin, F. et al. Monolithic chip for high-throughput blood cell depletion to sort rare circulating tumor cells. Sci. Rep. 7, 10936 (2017).
Martel, J. M. et al. Continuous flow microfluidic bioparticle concentrator. Sci. Rep. 5, 11300 (2015).
Hassan, U., Watkins, N. N., Reddy, B., Damhorst, G. & Bashir, R. Microfluidic differential immuno-capture biochip for specific leukocyte counting. Nat. Protoc. 11, 714–726 (2016).
Hassan, U. et al. A microfluidic biochip for complete blood cell counts at the point-of-care. Technology 3, 201–213 (2015).
Hassan, U. et al. A point-of-care microfluidic biochip for quantification of CD64 expression from whole blood for sepsis stratification. Nat. Commun. 8, 15949 (2017).
Valera, E., Shia, W. W. & Bailey, R. C. Development and validation of an immunosensor for monocyte chemotactic protein 1 using a silicon photonic micro-ring resonator biosensing platform. Clin. Biochem. 49, 121–126 (2016).
Liu, D. et al. A fully integrated distance readout ELISA-chip for point-of-care testing with sample-in-answer-out capability. Biosens. Bioelectron. 96, 332–338 (2017).
Islam, F. et al. An electrochemical method for sensitive and rapid detection of FAM134B protein in colon cancer samples. Sci. Rep. 7, 133 (2017).
Tacke, F. et al. Levels of circulating miR-133a are elevated in sepsis and predict mortality in critically ill patients. Crit. Care Med. 42, 1096–1104 (2014).
Roderburg, C. et al. Circulating microRNA-150 serum levels predict survival in patients with critical illness and sepsis. PLoS ONE 8, e54612 (2013).
Bomsztyk, K. et al. Experimental acute lung injury induces multi-organ epigenetic modifications in key angiogenic genes implicated in sepsis-associated endothelial dysfunction. Crit. Care 19, 225 (2015).
Hur, S. C., Henderson-MacLennan, N. K., McCabec, E. R. B. & Carlo, D. D. Deformability based cell classification and enrichment using inertial microfluidics. Lab Chip 11, 912–920 (2011).
Wang, G. et al. Stiffness dependent separation of cells in a microfluidic device. PLoS ONE 8, e75901 (2013).
Rassaei, L., Olthuis, W., Tsujimura, S., Sudhölter, E. R. & van den Berg, A. Lactate biosensors: current status and outlook. Anal. Bioanal. Chem. 406, 123–137 (2014).
Angus, D. C. Defining sepsis: a case of bounded rationality and fuzzy thinking?. Am. J. Respir. Crit. Care Med. 194, 14–15 (2016).
Ellett, F. et al. Diagnosis of sepsis from a drop of blood by measurement of spontaneous neutrophil motility in a microfluidic assay. Nat. Biomed. Eng. 2, 207–214 (2018).
Jämsä, J., Huotari, V., Savolainen, E. R., Syrjälä, H. & Ala-Kokko, T. Analysis of the temperature affects on leukocyte surface antigen expression. J. Clin. Lab. Anal. 25, 118–125 (2011).
How to find and effectively use predicate devices. US Food and Drug Administration https://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/HowtoMarketYourDevice/PremarketSubmissions/PremarketNotification510k/ucm134571.htm (2017).
Haak, B. W. & Wiersinga, W. J. The role of the gut microbiota in sepsis. Lancet 2, 135–143 (2017).
Dickson, R. P. et al. Enrichment of the lung microbiome with gut bacteria in sepsis and the acute respiratory distress syndrome. Nat. Microbiol. 1, 16113 (2016).
Budden, K. F. et al. Emerging pathogenic links between microbiota and the gut–lung axis. Nat. Rev. Microbiol. 15, 55–63 (2017).
Fired, J. On World Sepsis Day, a call for much-needed research funding. Noozhawk https://www.noozhawk.com/article/dr._jeffrey_fried_world_sepsis_day (2014).
Sepsis: a word to know, a meaning to learn. Sepsis Alliance News https://www.sepsis.org/sepsis-alliance-news/sepsis-word-know-meaning-learn/ (2017).
Acknowledgements
The authors thank B. Davis, J. Kumar, V. Reddi, J. Eardley, E. Iniguez, N. Topudurti, G. Damhorst and I. Taneja for useful discussions around clinical care for septic patients, technology development and data analytics.
Author information
Authors and Affiliations
Contributions
B.R., U.H. and R.B. conceived and designed the article. C.S., T.S.I., D.C.A., L.Y., W.W., K.W. and A.V. helped in identifying the primary clinical needs in sepsis and provided intellectual input on the best solutions to these needs. B.R. and U.H. made the figures and table. All authors provided input and reviewed the article. B.R., U.H. and R.B. edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
B.R., R.B. and U.H. have financial interests in Prenosis Inc. The remaining authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reddy, B., Hassan, U., Seymour, C. et al. Point-of-care sensors for the management of sepsis. Nat Biomed Eng 2, 640–648 (2018). https://doi.org/10.1038/s41551-018-0288-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-018-0288-9
This article is cited by
-
Smartphone-based platforms implementing microfluidic detection with image-based artificial intelligence
Nature Communications (2023)
-
A combined risk model for the multi-encompassing identification of heterogeneities of prognoses, biological pathway variations and immune states for sepsis patients
BMC Anesthesiology (2022)
-
Wearable, wireless, multi-sensor device for monitoring tissue circulation after free-tissue transplantation: a multicentre clinical trial
Scientific Reports (2022)
-
Wearable chemical sensors for biomarker discovery in the omics era
Nature Reviews Chemistry (2022)
-
Micro- and nanosensors for detecting blood pathogens and biomarkers at different points of sepsis care
Microchimica Acta (2022)