Abstract
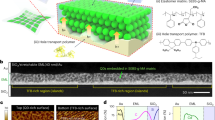
Metronomic (that is, low-dose and long-term) photodynamic therapy (mPDT) for treating internal lesions requires the stable fixation of optical devices to internal tissue surfaces to enable continuous, local light delivery. Surgical suturing—the standard choice for device fixation—can be unsuitable in the presence of surrounding major nerves and blood vessels, as well as for organs or tissues that are fragile, change their shape or actively move. Here, we show that an implantable and wirelessly powered mPDT device consisting of near-field-communication-based light-emitting-diode chips and bioadhesive and stretchable polydopamine-modified poly(dimethylsiloxane) nanosheets can be stably fixed onto the inner surface of animal tissue. When implanted subcutaneously in mice with intradermally transplanted tumours, the device led to significant antitumour effects by irradiating for 10 d at approximately 1,000-fold lower intensity than conventional PDT approaches. The mPDT device might facilitate treatment strategies for hard-to-detect microtumours and deeply located lesions that are hard to reach with standard phototherapy.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Yun, S. H. & Kwok, S. J. J. Light in diagnosis, therapy and surgery. Nat. Biomed. Eng. 1, 0008 (2017).
Agostinis, P. et al. Photodynamic therapy of cancer: an update. CA Cancer J. Clin. 61, 250–281 (2011).
Mackenzie, G. D. et al. How light dosimetry influences the efficacy of photodynamic therapy with 5-aminolaevulinic acid for ablation of high-grade dysplasia in Barrett’s esophagus. Lasers Med. Sci. 23, 203–210 (2008).
Kinsey, J., Cortese, D. & Neel, H. Thermal considerations in murine tumour killing using hematoporphyrin derivative phototherapy. Cancer Res. 43, 1562–1567 (1983).
Horimatsu, T. et al. Tissue damage in the canine normal esophagus by photoactivation with talaporfin sodium (laserphyrin): a preclinical study. PLoS ONE 7, e38308 (2012).
Overholt, B. F. et al. Photodynamic therapy with porfimer sodium for ablation of high-grade dysplasia in Barrett’s esophagus: international, partially blinded, randomized phase III trial. Gastrointest. Endosc. 62, 488–498 (2005).
Wolfsen, H. C. et al. Clinical experience of patients undergoing photodynamic therapy for Barrett’s dysplasia or cancer. Aliment. Pharmacol. Ther. 20, 1125–1131 (2004).
Lam, S. et al. Photodynamic therapy with Photofrin®, a treatment with curative potential for early-stage superficial lung cancer. In Proc. 34th Annual Meeting of the American Society of Clinical Oncology (ASCO, Los Angeles, CA, 1998).
Istomin, Y. et al. Photodynamic therapy of cervical intraepithelial neoplasia grades II and III with Photolon®. Photodiagnosis Photodyn. Ther. 7, 144–151 (2010).
Choi, M. C. et al. Photodynamic therapy for management of cervical intraepithelial neoplasia II and III in young patients and obstetric outcomes. Lasers Surg. Med. 45, 564–572 (2013).
Bisland, S. K. et al. Metronomic photodynamic therapy as a new paradigm for photodynamic therapy: rationale and preclinical evaluation of technical feasibility for treating malignant brain tumours. Photochem. Photobiol. 80, 22–30 (2004).
Bruijn, S. De, Balbas, E. M., Sterenborg, H. J. C. M., French, P. J. & Robinson, D. J. A telemetric light delivery system for metronomic photodynamic therapy (mPDT) in rats. J. Biophotonics 3, 347–355 (2010).
Shin, G. et al. Fully implantable, battery-free wireless optoelectronic devices for spinal optogenetics. Pain 158, 2108–2116 (2017).
Samineni, V. K. et al. Injectable, cellular-scale optoelectronics with applications for wireless optogenetics. Science 340, 211–217 (2013).
Montgomery, K. L. et al. Wirelessly powered, fully internal optogenetics for brain, spinal and peripheral circuits in mice. Nat. Methods 12, 969–974 (2015).
Park, S. I. et al. Soft, stretchable, fully implantable miniaturized optoelectronic systems for wireless optogenetics. Nat. Biotechnol. 33, 1280–1286 (2015).
Fujie, T., Okamura, Y. & Takeoka, S. Ubiquitous transference of a free-standing polysaccharide nanosheet with the development of a nano-adhesive plaster. Adv. Mater. 19, 3549–3553 (2007).
Fujie, T. Development of free-standing polymer nanosheets for advanced medical and health-care applications. Polymer J. 48, 773–780 (2016).
Lee, H., Scherer, N. F. & Messersmith, P. B. Single-molecule mechanics of mussel adhesion. Proc. Natl Acad. Sci. USA 103, 12999–13003 (2006).
Lee, H., Dellatore, S. M., Miller, W. M. & Messersmith, P. B. Mussel-inspired surface chemistry for multifunctional coatings. Science 318, 426–430 (2007).
Zucca, A. et al. Roll to roll processing of ultraconformable conducting polymer nanosheets. J. Mater. Chem. C 3, 6539–6548 (2015).
Fujie, T. et al. Adhesive, flexible, and robust polysaccharide nanosheets integrated for tissue-defect repair. Adv. Funct. Mater. 19, 2560–2568 (2009).
Kim, H. W. et al. Oxygen concentration control of dopamine-induced high uniformity surface coating chemistry. ACS Appl. Mater. Interfaces 5, 233–238 (2013).
Xue, P. et al. Surface modification of poly(dimethylsiloxane) with polydopamine and hyaluronic acid to enhance hemocompatibility for potential applications in medical implants or devices. ACS Appl. Mater. Interfaces 9, 33632 (2017).
Terry, B. S., Passernig, A. C., Hill, M. L., Schoen, J. A. & Rentschler, M. E. Small intestine mucosal adhesivity to in vivo capsule robot materials. J. Mech. Behav. Biomed. Mater. 15, 24–32 (2012).
Kaltenbrunner, M. et al. An ultra-lightweight design for imperceptible plastic electronics. Nature 499, 458–463 (2013).
Taniyama, T., Azuma, I., Aladin, A. A. & Yamamura, Y. Effect of cell-wall skeleton of Mycobacterium bovis BCG on cell-mediated cytotoxicity in tumour-bearing mice. Jpn J. Cancer Res. 66, 705–709 (1975).
Mathews, M. S. et al. The effects of ultra low fluence rate single and repetitive photodynamic therapy on glioma spheroids. Lasers Surg. Med. 41, 578–584 (2009).
Bisland, S. K. et al. Metronomic photodynamic therapy as a new paradigm for photodynamic therapy: rationale and preclinical evaluation of technical feasibility for treating malignant brain tumours. Photochem. Photobiol. 80, 22–30 (2004).
Singh, G. et al. in Photodynamic Therapy: Methods and Protocols 1st edn (ed. Gomer, C. J.) 65–78 (Humana Press, New York, 2010).
Davies, N. & Wilson, B. C. Interstitial in vivo ALA-PpIX mediated metronomic photodynamic therapy (mPDT) using the CNS-1 astrocytoma with bioluminescence monitoring. Photodiagnostics Photodyn. Ther. 4, 202–212 (2007).
Bogaards, A. et al. Fluorescence image-guided brain tumour resection with adjuvant metronomic photodynamic therapy: pre-clinical model and technology development. Photochem. Photobiol. Sci. 4, 438–442 (2005).
Fernandez, J. M. et al. Singlet oxygen generation by photodynamic agents. J. Photochem. Photobiol. B 37, 131–140 (1997).
Hino, H., Murayama, Y. & Nakanishi, M. 5-Aminolevulinic acid-mediated photodynamic therapy using light-emitting diodes of different wavelengths in a mouse model of peritoneally disseminated gastric cancer. J. Surg. Res. 185, 119–126 (2013).
Fleischer, F. et al. Comparison of red and green light in the treatment of Bowen’s disease by photodynamic therapy. Br. J. Dermatol. 143, 767–772 (2000).
Fritsch, C. et al. Green light is effective and less painful than red light in photodynamic therapy of facial solar keratoses. Photodermatol. Photoimmunol. Photomed. 13, 181–185 (1997).
van Duijnhoven, F. H., Aalbers, R. I. J. M., Rovers, J. P., Terpstra, O. T. & Kuppen, P. J. K. The immunological consequences of photodynamic treatment of cancer, a literature review. Immunobiology 207, 105–113 (2003).
Acknowledgements
This work was supported by the Leading Graduate Program in Science and Engineering, Waseda University from MEXT, Top Global University Program, Waseda University from MEXT, JSPS KAKENHI (grant numbers 15H05355, 15K15503 and 17K20116), a Grant-in-Aid for JSPS Fellows (grant number 16J07140), a Precursory Research for Embryonic Science and Technology (PRESTO) grant from the Japan Science and Technology Agency (JPMJPR152A), the Noguchi Institute and the Tanaka Memorial Foundation. The authors thank K. Iwasaki and X. Zhu (Waseda University) for valuable technical advice and X-ray transmission imaging observations; H. Miyazaki, D. Saitoh (National Defense Medical College), M. Kitajima (Waseda University) and F. Greco (Graz University of Technology) for valuable discussions; and W. Kayukawa, Y. Matsushita and T. Takee for technical assistance in cell culture.
Author information
Authors and Affiliations
Contributions
S.T., Y.M. and T.F. jointly supervised this work. K.Y. and I.T. prepared and characterized the PDA–PDMS nanosheets. K.Y., I.K. and H.A. performed the in vivo experiments. K.Y., S.T., Y.M. and T.F. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
This work relates to patent PCT/JP201716283.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Information
Supplementary figures and tables.
Supplementary Video 1
LED emission in two mice implanted with a NFC-based red or green LED device.
Supplementary Video 2
Mouse bearing two red LED devices implanted under the dorsal skin.
Supplementary Video 3
Mouse bearing two green LED devices implanted under the dorsal skin.
Supplementary Video 4
Experimental set-up for a tack test to evaluate the adhesive energy between PDMS and chicken muscle.
Supplementary Video 5
Intradermal injection of cancer cells (Colon-26) in the dorsal skin of a mouse.
Supplementary Video 6
Implanted LED device on the inner surface of the dorsal skin (opened skin) remains in position when the skin is stretched, compressed and twisted.
Supplementary Video 7
Implanted LED device on the inner surface of the dorsal skin (closed skin) remains in position when the skin is stretched, compressed and twisted.
Rights and permissions
About this article
Cite this article
Yamagishi, K., Kirino, I., Takahashi, I. et al. Tissue-adhesive wirelessly powered optoelectronic device for metronomic photodynamic cancer therapy. Nat Biomed Eng 3, 27–36 (2019). https://doi.org/10.1038/s41551-018-0261-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-018-0261-7
This article is cited by
-
Body-conformable light-emitting materials and devices
Nature Photonics (2024)
-
Wearable and Implantable Light-Emitting Diodes and Their Biomedical Applications
Korean Journal of Chemical Engineering (2024)
-
Fully implantable and battery-free wireless optoelectronic system for modulable cancer therapy and real-time monitoring
npj Flexible Electronics (2023)
-
A biodegradable, flexible photonic patch for in vivo phototherapy
Nature Communications (2023)
-
Active tissue adhesive activates mechanosensors and prevents muscle atrophy
Nature Materials (2023)