Abstract
The incidence of invasive pneumococcal disease (IPD) caused by infection with the pathogen Streptococcus pneumoniae (Spn) has been on a downward trend for decades due to worldwide vaccination programs. Despite the clinical successes observed, the Center for Disease Control (CDC) reports that the continued global burden of S. pneumoniae will be in the millions each year, with a case-fatality rate hovering around 5%. Thus, it is a top priority to continue developing new Spn vaccination strategies to harness immunological insight and increase the magnitude of protection provided. As emphasized by the World Health Organization (WHO), it is also crucial to broaden the implementation of vaccines that are already obtainable in the clinical setting. This review focuses on the immune mechanisms triggered by existing pneumococcal vaccines and provides an overview of the current and upcoming clinical strategies being employed. We highlight the associated challenges of serotype selectivity and using pneumococcal-derived proteins as alternative vaccine antigens.
Similar content being viewed by others
Introduction
Of the many bacterial pathogens responsible for widespread human illness, Streptococcus pneumoniae continues to be a significant threat, despite the introduction of vaccine programs to abrogate the spread of the disease four decades ago. Widespread asymptomatic colonization of the bacterium within the host nasopharynx gives rise to invasive disease as the body’s immune system has a reduced ability to act against the virulence factors of Spn, primarily the capsular polysaccharide (CPS) that coats the outer surface1. The distinct chemical structure of each CPS defines the approximately 100 serotypes known to comprise Spn as a species2. The heterogeneity in the monosaccharide building blocks and how they are linked and modified by the bacterium allows for specific antibody binding to each CPS, hence serotyping2,3. While regional differences exist in dominant serotype colonization and infection, 20 to 25 predominant serotypes are responsible for approximately 90% of IPD cases4,5.
IPD caused by Spn infection can take multiple clinical manifestations throughout the host, depending on the anatomical location bacterial pathogenesis occurs. Most commonly observed is lung infection leading to pneumonia, as the opportunistic bacteria spread through horizontal dissemination from the nasopharynx and colonize without immune clearance6. Continued propagation leads to more severe pathologies, with acute infection in the blood leading to septicemia or bacteremia and spinal cord and brain infections leading to meningitis6,7. These severe pathologies occur in nearly one-third of patients hospitalized with Spn infection, with survivors experiencing further sequelae, including the increased occurrence of neurological and cardiovascular defects and reduced lifespan8. Additionally, coinfection with IPD in hospitalized influenza or COVID patients significantly increases intensive care and fatalities9,10,11. A systematic analysis of lower respiratory infections found the global burden of Spn in 2016 to be an estimated 15 cases per 100,000 persons per year, or 1.1 million deaths resultant of pneumococcal infection12. Given the dire issue of IPD morbidity and mortality worldwide, preventing colonization through vaccination remains a high priority.
This review covers the current strategies used to develop pneumococcal vaccines and the findings related to their immune mechanisms. Additionally, we explore the clinical and manufacturing challenges associated with these vaccines. Finally, we highlight alternative protective antigens with the potential to provide broad protection in future clinical preparations.
Immune mechanisms induced by pneumococcal vaccines
Phagocytosis is the primary mechanism for the immune clearance of pneumococcal colonization by the host13,14. CPSs help bacterial pathogens evade immune-mediated clearance by inhibiting complement activation and preventing phagocytosis15,16. On the other hand, their surface exposure and distinct chemical structures allow for the exploitation of CPSs in vaccine design as antigens to induce opsonophagocytic killing of bacteria and elicit protective immune responses against encapsulated bacterial pathogens13,14. Serotype-specific, antibody-mediated protection from pneumococcal disease was established as early as the beginning of the 20th century, with modern vaccination programs seeing incredible success in the clinical space by seeking to eliminate the colonization of specific serotypes17,18. This goal has been pursued by building immunity against the CPS expressed on the surface of serotypes found to be most burdensome. The earliest iterations of this vaccine used purified, bacterial-derived CPS to activate the immune system, which is incapable of initiating the adaptive immune response and thus limited the vaccine’s effectiveness to eliciting predominantly short-living, low-affinity IgM antibody responses that are significantly reduced after six months in most serotypes, and back to baseline immunity within 24 months19,20.
The immunological mechanism harnessed using CPS alone as the antigen meant a specific clone of B cell capable of CPS recognition through its B cell receptor leads to the secretion of IgM antibodies19. However, most pure CPSs cannot trigger T cell help to induce antibody class switching, affinity maturation, and memory B and T cell production, all important for effective and prolonged protection19,21,22,23. An important milestone in vaccine design has been the introduction of conjugation technology in clinical vaccine programs24,25. The covalent conjugation of the CPS to an immunogenic carrier protein yielded what is now known as glycoconjugate vaccines24,25. Glycoconjugate vaccines induce an adaptive immune response targeting the CPS, IgM to IgG antibody class switching, affinity maturation, and immune memory, and are significantly more protective than pure polysaccharide vaccines26,27. While these vaccines have drastically reduced pneumococcal diseases globally, their variable immunogenicity, batch-to-batch inconsistency, and heterogeneous compositions manifested significant clinical shortcomings24,25. For example, numerous studies have shown that serotype 3 is highly unresponsive to the current pneumococcal multi-valent conjugate vaccine PCV1328,29,30,31, and incidence rates of serotype 3 continue to rise32. While Spn3 accounts for more than 10% (and increasing) of morbidity associated with IPD, it is responsible for approximately 25% of sepsis caused by Spn, and even more dramatically, IPD caused by serotype 3 has a 30% higher mortality rate than other serotypes33,34,35. Recent epidemiology work in Germany reveals serotype 3 as the most prevalent serotype identified in cases of community-acquired pneumonia, all of which required hospitalization36. Another epidemiology work in Portugal evaluated the impact of continued PCV13 vaccine use in pediatric IPD and reported serotype 3 as the most frequently detected serotype37. The need to modernize their design and development processes and generate structurally and functionally homogenous vaccines with increased efficacy offered opportunities to elucidate molecular and cellular mechanisms of how they induce adaptive humoral immune responses24,25.
A comprehensive elucidation of glycoconjugate vaccine-induced immune mechanisms was reported over a decade ago by ref. 38. According to this model, glycoconjugate vaccines stimulate strong adaptive immune responses through carbohydrate-specific T cells, or Tcarbs38,39. By covalently attaching CPS to an immunogenic protein, a shift in the immunological mechanism harnessed occurs, with the conjugate molecule being trafficked to the endolysosomes and degraded through the activity of reactive oxygen or nitrogen species as well as enzymatic hydrolysis, ultimately resulting in discrete glyco-epitopes that bind to the major histocompatibility complex protein, MHCII, and are presented by antigen-presenting cells for CD4 + T helper cell recognition38,39,40. This processing and presentation event is possible as the carrier protein contains sequences capable of association with MHCII, and the depolymerized CPS epitopes covalently bound to the peptide fragments on the MHCII groove enable the presentation of CPS to CD4 + T cells with a T cell receptor recognizing processed CPS as its epitope38,40. The immune synapse formed between the B and T cell facilitates the adaptive immune response through the differentiation of B cells to high-affinity IgG-producing plasma cells and memory cell formation13. The initial mechanistic study on glycoconjugate vaccines was followed by additional studies that strengthened and further elaborated the Tcarb-mediated immune responses induced by glycoconjugate vaccines41,42,43. In one study, glycoconjugates of serotype 3 Streptococcus pneumoniae CPS (Pn3P) were employed to provide evidence for the functional roles of Pn3P-specific CD4 + T cells that induce Pn3P-specific immunoglobulin responses in a Tcarb-dependent manner40. More recently, glycoconjugate vaccines composed of Vi antigen from Salmonella typhi, Group B Streptococcus type 1b, and H. influenza type b were shown to induce Tcarb-mediated adaptive humoral immune responses41. In the same study, conjugates of group C polysaccharide from Neisseria meningitidis failed to induce humoral immunity through Tcarbs due to complete depolymerization of the poly-sialic acid structure during antigen processing.
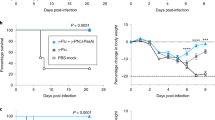
Elucidating the immune mechanisms to facilitate a protective immune response forms the knowledge basis for a forward-thinking approach to new-generation vaccine design. One example of knowledge-based vaccine design exploiting the antigen processing and presentation mechanisms elicited by glycoconjugate vaccines came from our studies, where we proposed the initial Tcarb model38. A prototype glycoconjugate vaccine designed to enrich for MHCII glyco-epitopes elicited up to two orders of magnitude higher IgG titers compared to a traditional glycoconjugate preparation and complete protection in a mouse challenge study.
Correlates of protection
Vaccine efficacy and the degree to which protection is garnered against specific serotypes must have a normalized metric to quantify immunity and determine noninferiority between the different vaccines manufactured. These metrics are collectively known as correlates of protection and are used to measure the degree of humoral response and the functional capability of the antibodies produced after vaccination44. The simplest quantifiable method to evaluate vaccine efficacy is by determining the robustness in the humoral response generated at predetermined time points throughout the vaccination schedule. This is typically performed through an Enzyme-Linked Immunosorbent Assay, or ELISA, where the particular CPS antigen or strain of Spn is immobilized and incubated with vaccinated serum, allowing for the serotype-specific antibodies to bind. ELISA provides a broad readout for the concentration and classes of CPS-specific antibodies produced through vaccination. Opsonophagocytosis is the primary mechanism of immune clearance against Spn and the current gold standard metric of pneumococcal vaccine efficiency is the Opsonophagocytic Killing Assay (OPKA, sometimes also referred to as OPA), in which the efficiency of immune-mediated killing elicited by vaccination is gauged14. In this assay, the specific serotype of interest is co-cultured with phagocytic cells and immunized serum that will lead the immune cells to engulf and kill the bacteria. Using these correlates of protection is how vaccine noninferiority criteria are met, with preclinical and clinical studies being performed against current standards of care to measure if the humoral and functional response generated through vaccination is comparable in animal models and humans.
Development of current clinical pneumococcal vaccines
One of the earliest iterations of an Spn vaccine, Pneumovax® PPSV23, came into the market in 1983 and was formulated as a multivalent vaccine using purified Spn CPSs isolated from the 23 serotypes responsible for the majority of IPD cases (Table 1)45. It was found to be efficient in adult and elderly populations, but poorly immunogenic in children and immunocompromised patients and had the drawback of requiring multiple doses as the efficacy of vaccine-elicited protection would wane without the ability to generate T cell-dependent immunity. The lack of protective immunity in the populations at highest risk of IPD and the variable responses and waning of immunity over time in the elderly represented an important challenge concerning vaccine-elicited protection against Spn46,47. In 2000, the multivalent Prevnar™ PCV7 was introduced to protect against the seven most virulent serotypes of S. pneumoniae through the preparation of individual serotype conjugates that are prepared and combined into multivalent formulations. Using purified CPSs that are first chemically modified to enable covalent attachment to CRM197, a genetically detoxified form of diphtheria toxin, the first commercially available conjugate vaccine against Spn was generated (Table 1). Updated versions of PCV7 have been released, covering additional serotypes from the 13-valent PCV13 up to the most recent 20-valent PCV20 (Table 1). Other carrier proteins have been explored, with the 10-valent Synflorix™ an example of a clinically available PCV that uses multiple carriers in its formulation, tetanus toxoid, and protein D from nontypeable H. influenzae.
In preparing these PCVs, there is a need for the chemical modification of CPS to an activated state prior to covalent attachment to the protein carrier due to the lack of reactive chemical handles on nearly all CPS used by Spn. Most conjugate formulations are developed by the initial oxidation of cyclic diol structures found within the CPS, using sodium periodate to modify the CPS and form reactive aldehyde groups capable of undergoing reductive amination with the surface-exposed lysine residues on a protein carrier to form a permanent bond48. This empirical method of conjugate formation and the large size of bacterially derived CPS leads to large globular structures as a lattice of CPS and carrier protein is formed through chemical attachment, limiting the degree of analytical approaches that can be used to define and characterize conjugates and evaluate clinical readiness49,50. In this regard, conjugates are analyzed for non-conjugated protein and polysaccharide content, and a ratio of protein to polysaccharide is determined to establish batch-to-batch consistency. Manufactured vaccines may have significant variability in physiochemical properties due to the different carrier proteins and the conjugation chemistry employed by each manufacturer. Additionally, the structural heterogeneity of conjugate vaccine products may arise among different batches of the same vaccine due to the inherent complexity of chemical conjugation strategies.
Recent developments in pneumococcal vaccine technology
In most iterations of current pneumococcal conjugate vaccines used in the clinic, an empirical approach is used to generate the molecules by activating the CPS for its covalent attachment to carrier proteins48. While this synthesis route works, it has shortcomings, such as overlooking the tentatively deleterious role the chemical activation of CPS can play, and that non-specific conjugation to the carrier can lead to a product that does not enable MHC presentation of key antigens51,52. The desire to combat the challenges with the current conjugation methodologies and enable better physiochemical characterization have prompted companies and academic research groups to explore the development of rationally defined and designed conjugate molecules. In the current clinical space, advances toward combating these shortcomings are being made with new formulations and phase trials to enhance conjugate vaccines' immune potential and structural homogeneity (Table 1).
Pneumosil is a recently developed and approved 10-valent conjugate vaccine comparable to other marketed PCVs in efficacy that uses an activation method that is not dependent on periodate oxidation, thereby potentially reducing the possible damage to CPS antigens that oxidation may have53. Conjugate preparations are made using CPS conjugated through 1-cyano-4-dimethylaminopyridinium tetrafluoroborate (CDAP) chemistry to CRM197, an approach that does not permanently alter the chemical structure of CPS outside of the points of conjugation54,55. This has the benefit of not significantly altering important physiochemical characteristic of the CPS.
Another strategy in development, VAX-24, tackles 24 serotypes through the preparation of conjugates using click chemistry functionalized CPS and the proprietary carrier eCRM, a CRM197 that has been modified to be expressed with replacement of lysine residues along the surface-exposed T cell epitopes into a non-canonical amino acid capable of specific reaction with the derivatized CPS56. This approach allows for the inclusion of site-selective conjugation that does not interfere with protein folding, thus keeping key tertiary structure features while enriching for CPS conjugate epitope sites57. Pre-clinical trials comparing VAX-24 to PCV13 and PPSV23, the standards of care at the time, illustrated comparable levels of humoral immune response and robust correlates of protection in animal models58. VAX-24 recently finished Phase 2 trials and has been designated as Breakthrough Therapy by US Food and Drug Administration (FDA) going into Phase 3, thus representing the value of analytically defined conjugate molecules. Critical T cell epitopes are claimed to be left undisturbed by the ability to specifically conjugate the CPS to the carrier at key points while minimizing conjugate heterogeneity and maximizing protein to polysaccharide content, all previously noted considerations that need to be addressed in the next generation of conjugate vaccines25.
AFX3772 is another versatile vaccine formulation that uses novel CPS and carrier modification to elicit protection against IPD in 24 serotypes, including Spn protein antigens59. The foundation of this approach is to use the Multiple Antigen-Presenting System (MAPS™) and generate macromolecular complexes consisting of biotin-modified CPS noncovalently attached to rhizavidin-fused carrier proteins. The strong interaction between biotin and rhizavidin functionally fuses the two components akin to a traditional conjugate but with a higher degree of control and versatility towards what is included in the complex59. In a combined Phase 1/2 study to evaluate safety and efficacy in healthy adults, AFX3772 exhibited a more robust antibody response than those generated upon vaccination with PCV13 and PPSV23 while maintaining a similar safety profile60. Due to the positive findings from this combined trial, the FDA granted AFX3772 the designation of Breakthrough Therapy as a preventative against IPD to adults aged 50 and older.
The vaccine candidates described thus far require a laborious process of individual isolation of the CPS antigen from bacteria, expression of the carrier structure to which it will be attached, subsequent modification and conjugation, and purification of a finalized product. To streamline the conjugation process and significantly decrease the cost of generating conjugate molecules, an alternative strategy is being explored in the preclinical space called Protein Glycan Coupling Technology, or bioconjugation. This approach clones the bacterial machinery for expressing the CPS, the carrier, and the enzyme that covalently attaches the two into E. coli to generate vaccine molecules, which are then capable of being purified and used directly, a strategy that has been used against other pathogenic bacteria previously61. In the context of Spn, it incorporates an oligosaccharyltransferase termed PglS that enables the covalent attachment of glucose-reducing end glycan structures, the most commonly found amongst CPS serotypes, onto a carrier protein that has a site for attachment by PglS62. This approach has the added benefit of a more homogenous conjugate identity, with the CPS attaching at the specific epitope sites PglS uses and through a singular attachment point on each polysaccharide’s reducing end. Evidence for the efficacy has been demonstrated through the generation of trivalent formulations that can generate a humoral immune response equal to PCV13, with a further study thoroughly characterizing the protection from sepsis and prevention of colonization of serotype 863,64.
Serotype selection in clinical formulations
Determination of the specific serotypes selected for inclusion in commercial formulations is an essential consideration in combating IPD, as there is some known heterogeneity in the reported prevalence and distribution of the serotypes on a global scale. Insight into the incidence rates caused by specific strains is critical in manufacturing vaccines, as this will drive vaccine policy and protective coverage. Overall, seven serotypes (1, 5, 6A, 6B, 14, 19F, and 23F) have been found to be the most common IPD-causing strains, with global analyses illustrating that two-thirds of all cases are isolates of these strains65. By further increasing the number of serotypes covered in PCV formulations, most strains responsible for IPD can be targeted. Prevnar 13®, the 13-valent PCV, was able to cover 76% of strains responsible for children under the age of five, with an estimated 78% reduction in IPD vaccine-related serotypes after introduction in the United States65. The updated 20-valent iteration now covers approximately 90% of total IPD serotypes66. The regional burden of particular serotypes varies, with current formulations more specifically protecting North American and European populations, whereas Asian and African IPD cases are due to a wider variety of serotypes65. Considerations must be made regarding what serotypes are selected for, as the current cumulative approach of continually adding serotypes in formulation does not account for possible evolutionary dynamics or the possible dampening of the immune response as the breadth of antigens introduced each vaccine increases. Further limitations exist outside the approach used to generate conjugate molecules and the selection of serotypes in formulations that drive vaccine policy12,67.
Serotype replacement is a phenomenon known to occur in response to vaccination as the current formulations are all dependent on targeting combinations of serotypes, with little to no meaningful amount of cross-protection elicited towards those not included68,69. While incidence rates and geographical trends play a major role in selecting serotypes to be included in the vaccine preparations, it results in a shift of Spn population dynamics as non-vaccine serotypes flourish and evolve outside of the natural fluctuations that are expected70,71. Most observations in this regard come from trends after the first-generation pneumococcal conjugate vaccines that targeted a smaller number of serotypes, as the later 13-, 15-, and 20-valent formulations have only more recently been made available. In one such study following a cohort of 383 children that had received the 7-valent conjugate vaccine, the overall carriage of Spn within the nasopharynx did not dramatically alter over time, but rather an increase in the non-vaccine serotypes compensated for the dramatic decrease in the serotypes vaccinated against72. Further, in a comprehensive analysis of pneumococcal isolates spanning pre- and post-PCV7 introduction by the CDC, it was found that a 1.5-fold increase of non-vaccine serotypes occurred over three years73. In the limited data looking at overall pneumococcal incidence before and after the introduction of the 7- and 13-valent conjugate vaccine, it was found that a small number of non-included serotypes rapidly increased to causing 40% of IPD occurrence, despite a relatively small degree of colonization previously74. While these trends do not dramatically impact the morbidity of IPD, it is critical to consider serotype selection and fluctuation in clinical preparations moving forward.
An additional topic of concern relative to serotype selection is the occurrence of capsular switching due to variable genotypic information within a serotype and the ability to share DNA between strains, resulting in differential expression of the CPS75. The ability of Spn to carry differing genetic information that resulted in distinct CPS was first described decades ago before it was fully understood what a genetic cassette was76. In most cases of CPS expression, a specific gene locus containing multiple genes related to capsule production occurs, with the diversity found across Spn as a species a consequence of mutation over time and intraspecies recombination77. Introducing a selective pressure in the form of serotype-specific vaccination can result in changes in CPS induction to enable the survival of the Spn and continual colonization, and has been observed in multiple studies, albeit in small numbers70,78,79,80. While capsular switching does not significantly threaten overall vaccine efficacy, it can exacerbate the rise of non-vaccine serotypes and represents a larger risk in antibiotic gene transfer amongst Spn serotypes81.
Alternative pneumococcal antigens
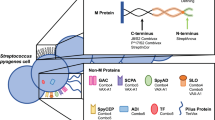
Despite the successes witnessed in the clinical space using CPS-containing vaccines, the serotype-directed approach has a major shortcoming: it can only protect against the individual serotypes accounted for in formulations. The outstanding serotype coverage obstacle is further compounded by the recent rise of non-encapsulated Spn strains that can colonize, albeit with no direct correlation to increased IPD cases in most circumstances82. With these considerations in mind, employing vaccine candidates based on conserved Spn surface proteins as the driving immunogen is an important area of focus that would expand the breadth of strain coverage while limiting the occurrence of capsular switching events. Towards this goal, multiple Spn surface proteins that could be harnessed as vaccine targets have been explored and thoroughly reviewed elsewhere83. Representative conserved vaccine candidates employed in clinical trials are summarized in Table 2 and below83,84.
The longest studied of pneumococcal protein immunogens is the cholesterol-dependent cytolysin, pneumolysin (PLY)85. PLY has been observed in nearly every IPD-causing strain, emphasizing the value such a vaccine target could bring to the clinical space86. The full-length PLY protein was found to provide protection against multiple Spn serotypes but exhibited cytotoxic behavior, leading to the exploration of detoxified mutants87,88. Genetically and chemically detoxified PLY derivatives (i.e., dPLY and PlyD), along with the immunogenic domains of the protein, are explored as vaccine targets, with positive results observed against several strains in early pre-clinical trials and clinical trials (Table 2)89,90,91,92,93,94,95.
Choline-binding proteins are major bacterial virulence factors, pneumococcal surface protein A (PspA) being among the most studied protein vaccine candidates as nearly all the clinically isolated Spn strains have been found to express it96,97. However, its large heterogeneity observed in domain sequences results in variability between clinical isolates98. Using conserved sequences amongst closely related domain clades and multivalent protein formulations, protective efficacy has been shown in early animal models and clinical trials to further drive PspA as a strong candidate for an alternative multi-serotype immunogen99,100.
Another major avenue of interest is the pneumococcal histidine triad protein D (PhtD) surface protein. First isolated and tested more than two decades ago, it was found to protect against sepsis in three highly virulent strains of Spn101. A strong push to use PhtD in the clinic led to phase trials both as a standalone immunogen and in concert with other protein targets, with results indicating the strong possibility of use in a protective vaccine102,103,104.
Using multiple protein antigens the most success has been found in the clinic, with successful early-stage clinical trials showing protection against specific serotypes of Spn83. These results, together with the expectedly lower cost of production, make Spn antigens an appealing vaccine candidate, especially when multiple are used together, albeit the issue of serotype non-inferiority against standard conjugate vaccines must be overcome. Expanding on the goal of developing a conserved/universal pneumococcal protein vaccine has led to the adaptation of a reverse vaccinology approach, wherein bioinformatics tools are applied to the Streptococcus pneumoniae genome to identify novel and tentatively immunogenic proteins105,106. These studies have shown promise in the discovery of new and promiscuous protein antigens capable of antibody generation specific to Spn but will need to be further refined and scrutinized given a lack of protection in murine sepsis challenge in vivo. The envisioned potential of this approach could work in concert with other important avenues of vaccinology research, including the emergent use of novel delivery systems that broaden the administration routes available and can act as a self-adjuvant107,108, which has been explored in one pre-clinical study using PspA100.
Discussion
The introduction of pneumococcal conjugate vaccine programs has profoundly impacted mortality and disease severity of IPD, with the need to push these programs further and address the limitations that have begun to arise. One remaining challenge lies in the methodology in which conjugate preparations are generated, in most cases working in an empirical approach to synthesize PCV products without taking insight from the immunological mechanisms at work. In these vaccines, there is an element of randomness in terms of where on the carrier protein and CPS conjugation is going to occur, with the issue further compounded by the as-of-yet unknown effect that polysaccharide size, chemical identity, and post-conjugation conformation play on immune responses25,41. The current conjugation methods add an additional degree of uncertainty, as there is no systematic assessment looking at all the different chemical approaches amongst the different serotypes and the relevance that linker molecules or degree of attachment can play in getting the CPS to be recognized by the B and T cells.
The selection of carrier protein employed plays a key role, as it enables the shift to an adaptive immune response, but with multiple carriers being used in the clinic, it isn’t clear if there is an ideal choice or how much the carrier itself is going to contribute to the protective action of the vaccines. Understanding carrier protein immune responses and thus enabling the use of carrier-derived peptide epitopes in developing novel knowledge-based vaccines may help combat persisting problems in glycoconjugate vaccine design. A potential concern is carrier-induced epitope suppression (CIES)109,110,111, wherein antibody response to the polysaccharide portion of the glycoconjugate vaccine can be inhibited due to pre-existing immune response to the carrier protein from prior immunizations. We postulate that reconstructing carrier proteins to form endolysosome-cleavable strings of polypeptides and their conjugation with polysaccharides is a novel approach to tackling CIES and the structural and functional heterogeneity of current conjugate vaccines. Toward this goal, we isolated and characterized new human MHCII-binging peptide epitopes derived from the two important vaccine immunogens TT and CRM197112. Harnessing carrier-derived peptides to generate multivalent carriers may yield knowledge-based, structurally, and functionally well-defined conjugate vaccines with robust, highly controlled, cost-effective production processes.
As an alternative or complementary strategy to conjugate vaccines, pneumococcal protein vaccines are being pursued in preclinical and clinical settings. These vaccines are designed to overcome the challenges associated with serotype-dependent PCVs and are postulated to work in conjunction with the conjugate vaccines currently employed in clinical practice. A serotype-independent protein vaccine has various advantages. It can be a cheaper option for children in developing countries, cover a wider range of geographical serotypes that cause IPD, and provide a new or alternative way to prevent recurrent infections. In the realm of manufacturing, it is imperative to note that protein-based antigens do not encounter the same hindrances associated with structural differences and variations between batches that are commonly observed in conjugate vaccines. Analytical and structural characterization tools such as mass spectrometry, NMR, and X-ray crystallography would allow for better characterization of protein vaccine products.
On the other hand, protein immunogens have several significant potential limitations as vaccine targets. First, they may or may not be present in most/all clinical isolates. Even if expressed in most clinical isolates, they may have significant sequence heterogeneity, rendering them poorly conserved. Another potential limitation of protein immunogens is their accessibility to opsonic antibodies on the bacterial surface. OPA is a major antibody-mediated immune response against extracellular bacterial pathogens, which makes CPSs an ideal vaccine target due to their accessibility to antibody binding. Along the same lines, protein immunogens mostly contain non-repeating conformational epitopes for antibody binding, making it challenging to raise protective antibody-mediated immunity, compared to CPSs, which possess repeating, conformationally less-restricted antigenic determinants. These limitations of protein immunogens may partially explain the difficulty in developing protein-based vaccines against extracellular bacterial pathogens. Regarding successful protein-based bacterial vaccine targets, non-toxic diphtheria and tetanus toxin variants effectively target the secreted toxins and inherently overcome the obstacles many protein vaccine targets face.
As a plausible conserved vaccine target, glycoproteins can offer the benefits of both polysaccharides and proteins by combining their antigenic and immunogenic properties. In S. pneumoniae, the Pneumococcal Serine-Rich Repeat Protein (PsrP) was established as a major virulence factor through large-scale mutagenesis screenings for lung infection113 and subsequently studied as a pathogenicity island114. PsrP is a very large, highly glycosylated, mucin-like adhesin that expands beyond the capsule115. Recently, multiple glycosyltransferases (GTs) responsible for PsrP glycosylation were shown to significantly impact PsrP’s biofilm formation and adhesion properties and lung infection in mice by intratracheal challenge115. Most recently, we investigated the prevalence and homology of PsrP globally, using the genomes of 13,454 clinically isolated pneumococci from the Global Pneumococcal Sequencing Project116. We found PsrP to be present in at least 50% of all strains, ranging up to over 70%, and it is heavily expressed in both vaccine and non-vaccine serotypes. Thus, formulating a new PsrP glycoprotein vaccine may serve the goal of a specific immune response that can provide broad protection against IPD globally. New and innovative conserved vaccine designs are being developed through preclinical research and clinical trials. These advancements, from animal testing to human testing, show potential for developing next-generation vaccines.
One area that requires particular attention is the introduction of new in vivo or ex vivo models for evaluating glycoconjugate vaccines. Current animal models with surrogate markers of protection (i.e., antibody titers and opsonophagocytic activity) can be inadequate and unreliably predictive of the responses of the target diverse human populations. Employing in vivo humanized mouse models to identify key helper T cell populations essential for vaccine efficacy may be highly important and innovative. Thankfully, the field of humanized mouse models is very rapidly progressing117. Alternatively, identifying human helper T cell populations essential for conjugate vaccine efficacy as a new immune correlate of protection may help tackle the obstacles associated with the limited current correlates of protection. To this end, understanding the molecular and cellular immune mechanisms induced by conjugate vaccines may yield a new immune correlate of protection to assess clinical vaccine products for their protective efficacy.
Overall, the brisk pace of development for pneumococcal vaccines has been remarkable, with numerous academic and industrial groups further elevating our understanding of how to control IPD worldwide. For many years, glycoconjugate vaccine formation was an unsystematic process of attaching immune-eliciting protein to the carbohydrate one wished to generate a response against. The current industry goals with novel vaccine strategies are primarily to develop distinct conjugation platforms with better-controlled chemistry and demonstrate non-inferiority, and not necessarily to garner new knowledge or improve on the efficacy of current conjugate vaccines. Understanding how conjugate vaccines work (i.e., what makes them antigenic and immunogenic) and why the current vaccines fail are critical parameters to achieve truly protective, widely applicable, and accessible vaccines against bacterial pathogens. By understanding the mechanism and process glycoconjugate vaccines undergo to elicit an immune response, a forward-thinking approach to future vaccines can begin. The goal is to develop a vaccine platform that is applicable to many microbial glycans because it is based on the basic immunologic mechanisms responsible for glycoconjugate processing, presentation, and T-helper cell reactivity. Our contribution towards this goal has been to establish new chemical and enzymatic conjugation strategies to develop chemoselective and structurally well-defined conjugative vaccines51,118,119; identify and characterize new human CD4 + T cell epitopes from vaccine immunogens112; develop a new structural model for the ligand binding of CPS specific protective antibodies120, and develop new chemical and enzymatic strategies to modulate CPSs for their optimum conjugation with carrier immunogens121,122,123. As the greater understanding of what drives immunological efficacy in PCVs grows, these insights can be further applied in the continued innovation in knowledge-based vaccine design.
References
Kadioglu, A., Weiser, J. N., Paton, J. C. & Andrew, P. W. The role of Streptococcus pneumoniae virulence factors in host respiratory colonization and disease. Nat. Rev. Microbiol. 6, 288–301 (2008).
Geno, K. A. et al. Pneumococcal capsules and their types: past, present, and future. Clin. Microbiol. Rev. 28, 871–899 (2015).
Jauneikaite, E. et al. Current methods for capsular typing of Streptococcus pneumoniae. J. Microbiol. Methods 113, 41–49 (2015).
Aliberti, S., Mantero, M., Mirsaeidi, M. & Blasi, F. The role of vaccination in preventing pneumococcal disease in adults. Clin. Microbiol. Infect. 20, 52–58 (2014).
Suaya, J. A. et al. Streptococcus pneumoniae serotype distribution and antimicrobial nonsusceptibility trends among adults with pneumonia in the United States, 2009‒2017. J. Infect. 81, 557–566 (2020).
Brooks, L. R. K. & Mias, G. I. Streptococcus pneumoniae’s virulence and host immunity: aging, diagnostics, and prevention. Front. Immunol. 9, 1366 (2018).
Chen, H. et al. Prognostic factors for mortality in invasive pneumococcal disease in adult: a system review and meta-analysis. Sci. Rep. 11, 11865 (2021).
Luck, J. N., Tettelin, H. & Orihuela, C. J. Sugar-coated killer: serotype 3 pneumococcal disease. Front. Cell. Infect. Microbiol. 10, 613287 (2020).
Santos, A. P. et al. Bacterial Co-Infection in patients with COVID-19 hospitalized (ICU and Not ICU): review and meta-analysis. Antibiotics 11, 894 (2022).
Hsing, T.-Y. et al. Clinical characteristics of influenza with or without Streptococcus pneumoniae co-infection in children. J. Formos. Med. Assoc. 121, 950–957 (2022).
Barman, T. K. et al. Lethal synergy between SARS-CoV-2 and Streptococcus pneumoniae in hACE2 mice and protective efficacy of vaccination. JCI Insight 7, https://doi.org/10.1172/jci.insight.159422 (2022).
Troeger, C. et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 18, 1191–1210 (2018).
Duke, J. A. & Avci, F. Y. Immunological mechanisms of glycoconjugate vaccines. In: Carbohydrate-based vaccines: from concept to clinic. (ed Prasad, K.) Ch 3, 61–74 ACS (Publications, 2018).
Paschall, A. V., Middleton, D. R. & Avci, F. Y. Opsonophagocytic killing assay to assess immunological responses against bacterial pathogens. J Visual. Exp. 146, e59400 (2019).
AlonsoDeVelasco, E., Verheul, A. F., Verhoef, J. & Snippe, H. Streptococcus pneumoniae: virulence factors, pathogenesis, and vaccines. Microbiol. Rev. 59, 591–603 (1995).
Casadevall, A. & Pirofski, L. A. Virulence factors and their mechanisms of action: the view from a damage-response framework. J. Water Health 7, S2–S18 (2009).
Wantuch, P. L. & Avci, F. Y. Invasive pneumococcal disease in relation to vaccine type serotypes. Hum. Vaccines Immunother. 15, 874–875 (2019).
Grabenstein, J. D. & Klugman, K. P. A century of pneumococcal vaccination research in humans. Clin. Microbiol. Infect. 18, 15–24 (2012).
Avci, F. & Kasper, D. How Bacterial carbohydrates influence the adaptive immune system. Annu. Rev. Immunol. 28, 107–130 (2010).
Momoyo, A. et al. Safety and immunogenicity of sequential administration of PCV13 followed by PPSV23 in pneumococcal vaccine-naïve adults aged ≥ 65 years: comparison of booster effects based on intervals of 0.5 and 1.0 year. Vaccine 41, 1042–1049 (2023).
Coutinho, A. & Möller, G. B cell mitogenic properties of thymus-independent antigens. Nat. New Biol. 245, 12–14 (1973).
Barrett, D. J. Human immune responses to polysaccharide antigens: an analysis of bacterial polysaccharide vaccines in infants. Adv. Pediatr. 32, 139–158 (1985).
Weintraub, A. Immunology of bacterial polysaccharide antigens. Carbohydr. Res. 338, 2539–2547 (2003).
Avci, F. Novel strategies for development of next-generation glycoconjugate vaccines. Curr. Top. Med. Chem. 13, 2535–2540 (2013).
Avci, F. et al. Glycoconjugates: what it would take to master these well-known yet little-understood immunogens for vaccine development. MSphere 4, e00520–00519 (2019).
Guttormsen, H., Wetzler, L., Finberg, R. & Kasper, D. Immunologic memory induced by a glycoconjugate vaccine in a murine adoptive lymphocyte transfer model. Infect. Immun. 66, 2026–2032 (1998).
Wessels, M. et al. Stimulation of protective antibodies against type Ia and Ib group B streptococci by a type Ia polysaccharide-tetanus toxoid conjugate vaccine. Infect. Immun. 61, 4760–4766 (1993).
Linley, E., Bell, A., Gritzfeld, J. F. & Borrow, R. Should Pneumococcal Serotype 3 Be Included in Serotype-Specific Immunoassays? Vaccines (Basel) 7, https://doi.org/10.3390/vaccines7010004 (2019).
Silva-Costa, C. et al. Pediatric complicated pneumonia caused by streptococcus pneumoniae serotype 3 in 13-Valent pneumococcal conjugate vaccinees, Portugal, 2010-2015. Emerg. Infect. Dis. 24, 1307–1314 (2018).
Horacio, A. N. et al. Serotype 3 remains the leading cause of invasive pneumococcal disease in adults in Portugal (2012-2014) despite continued reductions in other 13-Valent conjugate vaccine serotypes. Front. Microbiol. 7, 1616 (2016).
Horacio, A. N., Lopes, J. P., Ramirez, M. & Melo-Cristino, J., Portuguese Group for the Study of Streptococcal, I. Non-invasive pneumococcal pneumonia in Portugal–serotype distribution and antimicrobial resistance. PLoS One 9, e103092 (2014).
Wijayasri, S. et al. The shifting epidemiology and serotype distribution of invasive pneumococcal disease in Ontario, Canada, 2007-2017. PLoS One 14, e0226353 (2019).
Martens, P., Worm, S. W., Lundgren, B., Konradsen, H. B. & Benfield, T. Serotype-specific mortality from invasive streptococcus pneumoniae disease revisited. BMC Infect. Dis. 4, 21 (2004).
Briles, D. E., Crain, M. J., Gray, B. M., Forman, C. & Yother, J. Strong association between capsular type and virulence for mice among human isolates of Streptococcus pneumoniae. Infect. Immun. 60, 111–116 (1992).
Weinberger, D. M. et al. Association of serotype with risk of death due to pneumococcal pneumonia: a meta-analysis. Clin. Infect. Dis. 51, 692–699 (2010).
Forstner, C. et al. Pneumococcal conjugate serotype distribution and predominating role of serotype 3 in German adults with community-acquired pneumonia. Vaccine 38, 1129–1136 (2020).
Silva-Costa, C. et al. Dominance of vaccine serotypes in pediatric invasive pneumococcal infections in Portugal (2012-2015). Sci. Rep. 9, 6 (2019).
Avci, F. Y., Li, X., Tsuji, M. & Kasper, D. L. A mechanism for glycoconjugate vaccine activation of the adaptive immune system and its implications for vaccine design. Nat. Med. 17, 1602–1609 (2011).
Avci, F., Li, X., Tsuji, M. & Kasper, D. Isolation of carbohydrate-specific CD4(+) T cell clones from mice after stimulation by two model glycoconjugate vaccines. Nat. Protoc. 7, 2180–2192 (2012).
Middleton, D. R., Sun, L., Paschall, A. V. & Avci, F. Y. T cell–mediated humoral immune responses to type 3 capsular polysaccharide of Streptococcus pneumoniae. J. Immunol. 199, 598–603 (2017).
Sun, X., Stefanetti, G., Berti, F. & Kasper, D. L. Polysaccharide structure dictates mechanism of adaptive immune response to glycoconjugate vaccines. Proc. Natl. Acad. Sci. USA 116, 193–198 (2019).
Sterrett, S. et al. Peripheral CD4 T follicular cells induced by a conjugated pneumococcal vaccine correlate with enhanced opsonophagocytic antibody responses in younger individuals. Vaccine 38, 1778–1786 (2020).
Zhang, F., Thompson, C., Ma, N., Lu, Y.-J. & Malley, R. Carrier proteins facilitate the generation of Antipolysaccharide immunity via multiple mechanisms. Mbio 13, e03790–03721 (2022).
Plotkin, S. A. Correlates of protection induced by vaccination. Clin. Vaccin. Immunol. 17, 1055–1065 (2010).
Pilishvili, T. & Bennett, N. M. Pneumococcal disease prevention among adults: strategies for the use of pneumococcal vaccines. Vaccine 33, D60–D65 (2015).
Nuorti, J. P. & Whitney, C. G. Prevention of pneumococcal disease among infants and children — Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 59, 1–18 (2010).
Niederman, M. S. et al. Efficacy and effectiveness of a 23-valent polysaccharide vaccine against invasive and noninvasive pneumococcal disease and related outcomes: a review of available evidence. Expert Rev. Vaccines 20, 243–256 (2021).
Lees, A., Puvanesarajah, V. & Frasch, C. E. Conjugation chemistry. In: Pneumococcal vaccines: the impact of conjugate vaccines, (ed Siber, G.) 161–174, (Wiley, Hoboken, NY 2008).
Frasch, C. E. Preparation of bacterial polysaccharide–protein conjugates: analytical and manufacturing challenges. Vaccine 27, 6468–6470 (2009).
Berti, F. & Adamo, R. Antimicrobial glycoconjugate vaccines: an overview of classic and modern approaches for protein modification. Chem. Soc. Rev. 47, 9015–9025 (2018).
Duke, J. A. et al. Harnessing galactose oxidase in the development of a chemoenzymatic platform for glycoconjugate vaccine design. J. Biol. Chem. 298, 101453 (2022).
Adamo, R. et al. Synthetically defined glycoprotein vaccines: current status and future directions. Chem. Sci. 4, 2995–3008 (2013).
Temple, B. et al. Effect of a 2+ 1 schedule of ten-valent versus 13-valent pneumococcal conjugate vaccine on pneumococcal carriage: results from a randomised controlled trial in Vietnam. Vaccine 39, 2303–2310 (2021).
Lees, A., Nelson, B. L. & Mond, J. J. Activation of soluble polysaccharides with 1-cyano-4-dimethylaminopyridinium tetrafluoroborate for use in protein—polysaccharide conjugate vaccines and immunological reagents. Vaccine 14, 190–198 (1996).
Micoli, F., Romano, M. R., Carboni, F., Adamo, R. & Berti, F. Strengths and weaknesses of pneumococcal conjugate vaccines. Glycoconj. J. 40, 135–148 (2023).
Kang, M., Lu, Y., Chen, S. & Tian, F. Harnessing the power of an expanded genetic code toward next-generation biopharmaceuticals. Curr. Opin. Chem. Biol. 46, 123–129 (2018).
Kitowski, A., Corzana, F. & Bernardes, G. J. Precise protein conjugation technology for the construction of homogenous glycovaccines. Drug Discov. Today: Technol. 38, 69–75 (2020).
Fairman, J. et al. Non-clinical immunological comparison of a Next-Generation 24-valent pneumococcal conjugate vaccine (VAX-24) using site-specific carrier protein conjugation to the current standard of care (PCV13 and PPV23). Vaccine 39, 3197–3206 (2021).
Zhang, F., Lu, Y.-J. & Malley, R. Multiple antigen-presenting system (MAPS) to induce comprehensive B-and T-cell immunity. Proc. Natl. Acad. Sci. 110, 13564–13569 (2013).
Gurunadh, R. C. et al. Phase 1/2 study of a novel 24-valent pneumococcal vaccine in healthy adults aged 18 to 64 years and in older adults aged 65 to 85 years. Vaccine 40, 4190–4198 (2022).
Iwashkiw, J. A., Vozza, N. F., Kinsella, R. L. & Feldman, M. F. Pour some sugar on it: the expanding world of bacterial protein O‐linked glycosylation. Mol. Microbiol. 89, 14–28 (2013).
Harding, C. M. & Feldman, M. F. Glycoengineering bioconjugate vaccines, therapeutics, and diagnostics in E. coli. Glycobiology 29, 519–529 (2019).
Aceil, J. et al. Immunogenicity and protective efficacy of a prototype pneumococcal bioconjugate vaccine. Vaccine 40, 6107–6113 (2022).
Harding, C. M. et al. A platform for glycoengineering a polyvalent pneumococcal bioconjugate vaccine using E. coli as a host. Nat. Commun. 10, 891 (2019).
Johnson, H. L. et al. Systematic evaluation of serotypes causing invasive pneumococcal disease among children under five: the pneumococcal global serotype project. PLoS Med. 7, e1000348 (2010).
Klein, N. P. et al. A phase 3, randomized, double-blind study to evaluate the immunogenicity and safety of 3 lots of 20-valent pneumococcal conjugate vaccine in pneumococcal vaccine-naive adults 18 through 49 years of age. Vaccine 39, 5428–5435 (2021).
Vashishtha, V. Sero-epidemiology of Streptococcal pneumoniae in developing countries and Issues related to vaccination Vipin M Vashishtha, Puneet Kumar, Amol Mittal. J. Pediatr. Sci. 5, e49 (2010).
Weinberger, D. M., Malley, R. & Lipsitch, M. Serotype replacement in disease after pneumococcal vaccination. Lancet 378, 1962–1973 (2011).
Hausdorff, W. P., Hoet, B. & Schuerman, L. Do pneumococcal conjugate vaccines provide any cross-protection against serotype 19A? BMC Pediatr. 10, 1–7 (2010).
Croucher, N. J. et al. Rapid pneumococcal evolution in response to clinical interventions. Science 331, 430–434 (2011).
Wantuch, P. L. & Avci, F. Y. Current status and future directions of invasive pneumococcal diseases and prophylactic approaches to control them. Hum. Vaccin Immunother. 14, 2303–2309 (2018).
Veenhoven, R. et al. Effect of conjugate pneumococcal vaccine followed by polysaccharide pneumococcal vaccine on recurrent acute otitis media: a randomised study. Lancet 361, 2189–2195 (2003).
Beall, B. et al. Pre-and postvaccination clonal compositions of invasive pneumococcal serotypes for isolates collected in the United States in 1999, 2001, and 2002. J. Clin. Microbiol. 44, 999–1017 (2006).
Shamez, N. L. et al. Rapid increase in non-vaccine serotypes causing invasive pneumococcal disease in England and Wales, 2000–17: a prospective national observational cohort study. Lancet Infect. Dis. 18, 441–451 (2018).
Long, S. S. Capsules, clones, and curious events: pneumococcus under fire from polysaccharide conjugate vaccine. Clin. Infect. Dis. 41, 30–34 (2005).
Griffith, F. The significance of pneumococcal types. J. Hyg. (Lond.) 27, 113–159 (1928).
Wyres, K. L. et al. Pneumococcal capsular switching: a historical perspective. J. Infect. Dis. 207, 439–449 (2013).
Scott, J. R. et al. Pneumococcal sequence type replacement among American Indian children: a comparison of pre- and routine-PCV7 eras. Vaccine 30, 2376–2381 (2012).
Porat, N. et al. Emergence of penicillin-nonsusceptible Streptococcus pneumoniae clones expressing serotypes not present in the antipneumococcal conjugate vaccine. J. Infect. Dis. 190, 2154–2161 (2004).
Jefferies, J. M., Smith, A., Clarke, S. C., Dowson, C. & Mitchell, T. J. Genetic analysis of diverse disease-causing pneumococci indicates high levels of diversity within serotypes and capsule switching. J. Clin. Microbiol. 42, 5681–5688 (2004).
Dagan, R. & Klugman, K. P. Impact of conjugate pneumococcal vaccine on antibiotic resistance. Lancet Infect. Dis. 8, 785–795 (2008).
Park, I. H., Geno, K. A., Sherwood, L. K., Nahm, M. H. & Beall, B. Population-based analysis of invasive nontypeable pneumococci reveals that most have defective capsule synthesis genes. PLoS One 9, e97825 (2014).
Aceil, J. & Avci, F. Y. Pneumococcal surface proteins as virulence factors, immunogens, and conserved vaccine targets. Front. Cell. Infect. Microbiol. 12, 832254 (2022).
van de Garde, M. D. B., van Westen, E., Poelen, M. C. M., Rots, N. Y. & van Els, C. Prediction and validation of immunogenic domains of pneumococcal proteins recognized by human CD4(+) T Cells. Infect. Immun. 87, e00098–00019 (2019).
Paton, J. C., Lock, R. A. & Hansman, D. J. Effect of immunization with pneumolysin on survival time of mice challenged with Streptococcus pneumoniae. Infect. Immun. 40, 548–552 (1983).
Kanclerski, K. & Möllby, R. Production and purification of Streptococcus pneumoniae hemolysin (pneumolysin). J. Clin. Microbiol. 25, 222–225 (1987).
Alexander, J. E. et al. Immunization of mice with pneumolysin toxoid confers a significant degree of protection against at least nine serotypes of Streptococcus pneumoniae. Infect. Immun. 62, 5683–5688 (1994).
García-Suárez, M. D. M. et al. Protection against pneumococcal pneumonia in mice by monoclonal antibodies to pneumolysin. Infect. Immun. 72, 4534–4540 (2004).
Chen, A. et al. Multivalent pneumococcal protein vaccines comprising pneumolysoid with epitopes/fragments of CbpA and/or PspA Elicit Strong and broad protection. Clin. Vaccin Immunol. 22, 1079–1089 (2015).
Hermand, P. et al. Preclinical evaluation of a chemically detoxified pneumolysin as pneumococcal vaccine antigen. Hum. Vaccines Immunother. 13, 220–228 (2017).
Thanawastien, A. et al. Preclinical in vitro and in vivo profile of a highly-attenuated, broadly efficacious pneumolysin genetic toxoid. Vaccine 39, 1652–1660 (2021).
Kamtchoua, T. et al. Safety and immunogenicity of the pneumococcal pneumolysin derivative PlyD1 in a single-antigen protein vaccine candidate in adults. Vaccine 31, 327–333 (2013).
Odutola, A. et al. Immunogenicity of pneumococcal conjugate vaccine formulations containing pneumococcal proteins, and immunogenicity and reactogenicity of co-administered routine vaccines - a phase II, randomised, observer-blind study in Gambian infants. Vaccine 37, 2586–2599 (2019).
Odutola, A. et al. Efficacy of a novel, protein-based pneumococcal vaccine against nasopharyngeal carriage of Streptococcus pneumoniae in infants: a phase 2, randomized, controlled, observer-blind study. Vaccine 35, 2531–2542 (2017).
Odutola, A. et al. Reactogenicity, safety and immunogenicity of a protein-based pneumococcal vaccine in Gambian children aged 2-4 years: a phase II randomized study. Hum. Vaccin Immunother. 12, 393–402 (2016).
Crain, M. J. et al. Pneumococcal surface protein A (PspA) is serologically highly variable and is expressed by all clinically important capsular serotypes of Streptococcus pneumoniae. Infect. Immun. 58, 3293–3299 (1990).
Sempere, J. et al. Pneumococcal choline-binding proteins involved in virulence as vaccine candidates. Vaccines 9, 181 (2021).
McDaniel, L. S., McDaniel, D. O., Hollingshead, S. K. & Briles, D. E. Comparison of the PspA sequence from Streptococcus pneumoniae EF5668 to the previously identified PspA sequence from strain Rx1 and ability of PspA from EF5668 to elicit protection against pneumococci of different capsular types. Infect. Immun. 66, 4748–4754 (1998).
Mukerji, R. et al. The diversity of the proline-rich domain of pneumococcal surface protein A (PspA): potential relevance to a broad-spectrum vaccine. Vaccine 36, 6834–6843 (2018).
Nakahashi-Ouchida, R. et al. A nanogel-based trivalent PspA nasal vaccine protects macaques from intratracheal challenge with pneumococci. Vaccine 39, 3353–3364 (2021).
Adamou, J. E. et al. Identification and characterization of a novel family of pneumococcal proteins that are protective against Sepsis. Infect. Immun. 69, 949–958 (2001).
Seiberling, M. et al. Safety and immunogenicity of a pneumococcal histidine triad protein D vaccine candidate in adults. Vaccine 30, 7455–7460 (2012).
Brooks, W. A., Chang, L.-J., Sheng, X. & Hopfer, R. Safety and immunogenicity of a trivalent recombinant PcpA, PhtD, and PlyD1 pneumococcal protein vaccine in adults, toddlers, and infants: A phase I randomized controlled study. Vaccine 33, 4610–4617 (2015).
Odutola, A. et al. Immunogenicity of pneumococcal conjugate vaccine formulations containing pneumococcal proteins, and immunogenicity and reactogenicity of co-administered routine vaccines – a phase II, randomised, observer-blind study in Gambian infants. Vaccine 37, 2586–2599 (2019).
Talukdar, S., Zutshi, S., Prashanth, K. S., Saikia, K. K. & Kumar, P. Identification of potential vaccine candidates against Streptococcus pneumoniae by reverse vaccinology approach. Appl. Biochem. Biotechnol. 172, 3026–3041 (2014).
Lohany Dias, M. et al. Reverse and structural vaccinology approach to design a highly immunogenic multi-epitope subunit vaccine against Streptococcus pneumoniae infection. Infect. Genet. Evol. 85, 104473 (2020).
Tada, R. et al. Nasal vaccination with pneumococcal surface protein A in combination with cationic liposomes consisting of DOTAP and DC-chol confers antigen-mediated protective immunity against Streptococcus pneumoniae infections in mice. Int. Immunopharmacol. 61, 385–393 (2018).
Fukuyama, Y. et al. Nanogel-based pneumococcal surface protein A nasal vaccine induces microRNA-associated Th17 cell responses with neutralizing antibodies against Streptococcus pneumoniae in macaques. Mucosal Immunol. 8, 1144–1153 (2015).
Schutze, M. P., Leclerc, C., Jolivet, M., Audibert, F. & Chedid, L. Carrier-induced epitopic suppression, a major issue for future synthetic vaccines. J. Immunol. 135, 2319–2322 (1985).
Etlinger, H. M. et al. Use of prior vaccinations for the development of new vaccines. Science 249, 423–425 (1990).
Falugi, F. et al. Rationally designed strings of promiscuous CD4+ T cell epitopes provide help to Haemophilus influenzae type b oligosaccharide: a model for new conjugate vaccines. Eur. J. Immunol. 31, 3816–3824 (2001).
Wantuch, P. L. et al. Isolation and characterization of new human carrier peptides from two important vaccine immunogens. Vaccine 38, 2315–2325 (2020).
Hava, D. L. & Camilli, A. Large-scale identification of serotype 4 Streptococcus pneumoniae virulence factors. Mol. Microbiol. 45, 1389–1406 (2002).
Obert, C. et al. Identification of a candidate Streptococcus pneumoniae core genome and regions of diversity correlated with invasive pneumococcal disease. Infect. Immun. 74, 4766–4777 (2006).
Middleton, D. R., Aceil, J., Mustafa, S., Paschall, A. V. & Avci, F. Y. Glycosyltransferases within the psrP locus facilitate pneumococcal virulence. J. Bacteriol. 203, https://doi.org/10.1128/JB.00389-20 (2021).
Aceil, J., Venkat, A., Pan, E., Kannan, N. & Avci, F. Y. Prevalence and Homology of the Pneumococcal Serine-Rich Repeat Protein at the Global Scale. Microbiol. Spectr. 11, e03252–22 (2023).
Mian, S. A., Anjos-Afonso, F. & Bonnet, D. Advances in human immune system mouse models for studying human hematopoiesis and cancer immunotherapy. Front. Immunol. 11, 619236 (2020).
Cheng, S. et al. Glycoconjugate synthesis using chemoselective ligation. Org. Biomol. Chem. 17, 2646–2650 (2019).
Duke, J. A. et al. Development and Immunogenicity of a prototype multivalent Group B Streptococcus bioconjugate vaccine. ACS Infect. Dis. 7, 3111–3123 (2021).
Ozdilek, A. et al. A structural model for the ligand binding of pneumococcal serotype 3 capsular Polysaccharide-specific protective antibodies. MBio 12, e0080021 (2021).
Wantuch, P. L. et al. Characterization of the beta-glucuronidase Pn3Pase as the founding member of glycoside hydrolase family GH169. Glycobiology 31, 266–274 (2021).
Middleton, D. R. et al. Identification and characterization of the Streptococcus pneumoniae type 3 capsule-specific glycoside hydrolase of Paenibacillus species 32352. Glycobiology 28, 90–99 (2018).
Li, G. et al. Profiling pneumococcal type 3-derived oligosaccharides by high resolution liquid chromatography-tandem mass spectrometry. J. Chromatogr. A 1397, 43–51 (2015).
Platt, H. et al. Safety, tolerability, and immunogenicity of a 21-valent pneumococcal conjugate vaccine, V116, in healthy adults: phase 1/2, randomised, double-blind, active comparator-controlled, multicentre, US-based trial. Lancet Infect. Dis. 23, 233–246 (2023).
Leroux-Roels, I. et al. Adjuvant system AS02V enhances humoral and cellular immune responses to pneumococcal protein PhtD vaccine in healthy young and older adults: randomised, controlled trials. Vaccine 33, 577–584 (2015).
Bologa, M. et al. Safety and immunogenicity of pneumococcal protein vaccine candidates: monovalent choline-binding protein A (PcpA) vaccine and bivalent PcpA-pneumococcal histidine triad protein D vaccine. Vaccine 30, 7461–7468 (2012).
Acknowledgements
This work was supported by National Institutes of Health grants R01AI123383, R01AI152766, and R41AI157287.
Author information
Authors and Affiliations
Contributions
Both authors contributed to the manuscript’s conceptualization, literature search, and writing.
Corresponding author
Ethics declarations
Competing interests
J.A.D. is employed by Sanofi, which develops pneumococcal vaccines.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duke, J.A., Avci, F.Y. Emerging vaccine strategies against the incessant pneumococcal disease. npj Vaccines 8, 122 (2023). https://doi.org/10.1038/s41541-023-00715-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41541-023-00715-w