Abstract
Cognitive impairment is a core clinical feature of schizophrenia, exerting profound adverse effects on social functioning and quality of life in a large proportion of patients with schizophrenia. However, the mechanisms underlying the pathogenesis of schizophrenia-related cognitive impairment are not well understood. Microglia, the primary resident macrophages in the brain, have been shown to play important roles in psychiatric disorders, including schizophrenia. Increasing evidence has revealed excessive microglial activation in cognitive deficits related to a broad range of diseases and medical conditions. Relative to that about age-related cognitive deficits, current knowledge about the roles of microglia in cognitive impairment in neuropsychiatric disorders, such as schizophrenia, is limited, and such research is in its infancy. Thus, we conducted this review of the scientific literature with a focus on the role of microglia in schizophrenia-associated cognitive impairment, aiming to gain insight into the roles of microglial activation in the onset and progression of such impairment and to consider how scientific advances could be translated to preventive and therapeutic interventions. Research has demonstrated that microglia, especially those in the gray matter of the brain, are activated in schizophrenia. Upon activation, microglia release key proinflammatory cytokines and free radicals, which are well-recognized neurotoxic factors contributing to cognitive decline. Thus, we propose that the inhibition of microglial activation holds potential for the prevention and treatment of cognitive deficits in patients with schizophrenia. This review identifies potential targets for the development of new treatment strategies and eventually the improvement of care for these patients. It might also help psychologists and clinical investigators in planning future research.
Similar content being viewed by others
Introduction
Schizophrenia, a severe psychiatric disorder, remains an etiological and therapeutic challenge worldwide. Patients with schizophrenia present emotional and behavioral dysfunction, and usually some degree of cognitive deficit1. Cognitive impairment is well recognized as a core clinical feature of this disorder that has profound adverse impacts on the social functioning and quality of life of a majority of patients with schizophrenia1,2. Its trajectory has been shown to be distinct from those of the other clinical features of schizophrenia; it may be pre-existing and worsen abruptly within months before the appearance of psychotic symptoms1,3. No drug is currently available for the treatment of cognitive impairment in patients with schizophrenia. Although the pathological mechanisms underlying this impairment remain to be elucidated, substantial progress has been made in our understanding of causal factors and identification of targets for the development of novel therapeutic or even preventive interventions.
Microglia, together with astroglia, satellite glia, and oligodendroglia, are non-neuronal glial cells in the brain. Scientists are gaining increasing insight into the roles of microglia; they are known to have an immunological heritage and to act as primary resident macrophages, maintaining brain function and playing important roles in complex psychiatric disorders, including schizophrenia4,5. Microglia have immune and multiple non-immune functions essential for brain development and homeostasis. For instance, they directly mediate normal synaptic reorganization (pruning) in the developing brain, thereby playing a critical role in the modulation of synapse plasticity, defined as the ability of neurons to change the strength or efficacy of communication via synaptic transmission5,6. Using an in-vitro model of microglia-mediated synaptic pruning established with patient-derived neural cultures and isolated synaptosomes, Sellgren et al.6 obtained results suggesting that schizophrenia-related risk variants in the C4 locus lead to C4A-mediated excessive complement deposition, which may contribute, at least in part, to increased synaptic pruning mediated by activated microglia in schizophrenia. The exact mechanisms by which microglial activation is related to synaptic pruning and cognitive deficits in schizophrenia remain unclear, and further in-depth research is needed to provide fundamental evidence for the associations being suggested. Synapse plasticity is believed to be among the most fundamental abilities of the brain and a cellular basis for memory and learning5,6. This predominant type of non-neuronal glial cell is thus hypothesized to be linked to the pathogenesis of schizophrenia and the presence of cognitive impairment before or at the time of the first schizophrenic episode4,7. Findings from several studies support this hypothesis. For instance, postmortem histological examination and brain imaging revealed aberrant microglial activated in the brains of patients with schizophrenia, especially in the hippocampus, which is known to be associated with memory8,9,10,11. In addition, levels of key microglia-produced proinflammatory cytokines, including interleukin (IL)−6, tumor necrosis factor-alpha (TNF-α), and IL-1β, were elevated and these higher levels were correlated with poorer cognitive performance in patients with schizophrenia12,13. Rapid progress is being made in understanding the roles of microglia in this context, including abnormal activation, and the identification of microglia-expressed genetic variants and gray matter (GM)-mediated associations. Most recently, Corley and colleagues14 identified microglial-expressed risk-related genetic variants affecting the general cognitive ability, episodic memory, and working memory of patients with schizophrenia. In addition, higher microglial polygenic scores (PGSs), used to measure schizophrenia risk–associated microglial gene expression, were associated with greater cognitive impairment and lower gray matter volumes (GMVs) in patients with schizophrenia and in a large independent sample of UK Biobank participants (n = 134,827)14. These findings provide direct evidence of the contribution of genes expressed in the microglia to cognitive impairment in schizophrenia14. Research on correlations of microglial gene expression, molecular pathways, and brain structural and functional imaging findings with cognitive impairment is still in its infancy, and further in-depth investigation of the underlying mechanisms may aid the development of novel treatments for cognitive impairment in patients with schizophrenia.
We conducted this review to highlight recent findings regarding the roles of resident immune cells in the brain and microglia in cognitive deficits relevant to schizophrenia, and to discuss the aberrant activation of microglia even in the premorbid phase of schizophrenia. The gaining of insight into the pathological mechanisms underlying cognitive impairment in schizophrenia is a high research priority in the field, and discoveries have the potential to be translated into novel preventive and therapeutic measures. As the translation of such findings into therapeutics may involve the overcoming of certain challenges and the resolution of scientific issues, we also discuss future research directions to accelerate therapeutic development. Thus, this review may help physicians and clinical investigators in the field plan future research.
Cognitive impairment in schizophrenia
The German psychiatrist Emil Kraepelin (1856–1926) initially described cognitive impairment in patients with schizophrenia as dementia praecox15. Although cognitive impairment has not been included as a diagnostic criterion for schizophrenia in major guidelines (e.g., the International Classification of Diseases and Diagnostic and Statistical Manual of Mental Disorders), it is a well-documented core symptom of the disorder, as demonstrated by multiple lines of evidence, including but not limited to (1) the detection of cognitive decline relative to the premorbid status in up to 98% of patients with schizophrenia15,16, (2) the detection of cognitive deficits of varying severity in multiple domains in patients with schizophrenia2,15, and (3) the presence of cognitive impairment in the premorbid stage and at the onset of psychosis before treatment with antipsychotic medications in these patients17. Cognitive impairment has been found to progress in the first 3 years after the initiation of treatment with currently available antipsychotic agents and after remission in patients with schizophrenia18,19,20, suggesting that schizophrenia-related cognitive impairment has a course distinct from that of psychotic symptoms in these patients. The magnitude of cognitive impairment in schizophrenia varies across the premorbid phase, the time of the first psychotic episode, during treatment (or lack thereof) with antipsychotic medication, and after remission.
Neurocognitive dysfunction is a common symptom of schizophrenia, bipolar disorder (BD), and major depressive disorder (MDD), and comparisons of its profile and severity in these conditions have been extensive and have yielded somewhat mixed results. Cognitive deficits have been consistently found to be more severe and prevalent (affecting >80% of individuals) in patients with schizophrenia than in those with BD and MDD15,21,22,23,24,25,26,27. Furthermore, cognitive impairment in patients with schizophrenia usually precedes the first psychotic episode and subsequent diagnosis of the disease28,29. In contrast, better and worse premorbid cognitive performance has been associated with an increased risk of BD30,31,32. The reason underlying this difference is poorly understood. In a recent genome-wide analysis of a large sample of patients with schizophrenia (n = 82,315), those with BD (n = 51,710), and control individuals (n = 269,867), Smeland et al.22 revealed substantial overlap and distinctiveness of genetic factors related to cognitive performance in the former two groups. The majority (81%) of schizophrenia risk alleles correlated with lesser cognitive performance, whereas 75% of BD risk alleles were related to better cognitive performance22. This important study demonstrated the genetic basis, at least in part, of the shared but distinct cognitive impairment in patients with schizophrenia and those with BD22.
Schizophrenia-related cognitive impairment commonly affects seven domains of cognition: processing speed, attention and concentration, working memory, verbal learning and memory, visual learning and memory, reasoning and problem solving, and social cognition15,33,34,35. In a recent comprehensive examination of the findings of previous meta-analyses and systematic reviews, Gebreegziabhere and colleagues15 found that processing speed, working memory, and verbal learning and memory were more impaired than other cognitive domains, and that greater cognitive impairment was associated with poorer insight and functionality, in patients with schizophrenia. At present, the underlying mechanisms remain unclear. Functional imaging and neuropsychological findings have linked the loss of GMV to cognitive impairment in patients with schizophrenia19,20. In contrast to the age-related cognitive impairment occurring in Alzheimer’s disease, the impairment occurring in schizophrenia is often characterized by a greater loss of GMV than of white matter volume (WMV)19,20. The differences in the domains of cognition affected, the magnitude of cognitive impairment, and brain structural and functional changes may mean that the pathological mechanisms implicated in schizophrenia-related cognitive impairment differ from those implicated in other forms of such impairment.
Hypothetical explanations for schizophrenia-associated cognitive impairment involve the aberrant activation of microglial cells4,5. In view of the emerging link of microglial activation to cognitive impairment in schizophrenia, we next focus on current insights into the roles of microglia and potential underlying mechanisms.
Progress in understanding the roles of microglia in cognitive impairment in schizophrenia
The past two decades have witnessed a revolutionary discovery and subsequent advances in our understanding of microglia, including the association of pro-inflammatory polarization and excessive microglial activation with synaptic pruning in juveniles. Synaptic pruning is the process of eliminating extra neurons and synaptic connections and is essential for the maintenance of normal brain development, particularly in the early postnatal period and adolescence in animals and humans. Extensive synapse elimination in the cerebral cortex usually occurs in late adolescence36. Exaggerated synaptic pruning by microglia has been proposed to be a key contributing factor and potentially involved in the pathogenesis of schizophrenia6,37,38. The roles of microglia in the development and worsening of cognitive impairment and other symptoms of schizophrenia are increasingly being uncovered4,5. Substantial progress has been made in determining how microglial cells are activated, how homeostasis is modulated, and how microglial activation influences synaptic pruning, synapse plasticity, and the phagocytosis of apoptotic cells in the brain4,5,7.
Microglial activation in schizophrenia
Bloomeld and colleagues39 showed that the binding ratio of the second-generation translocator protein (TSPO) radioligand [11 C] peripheral benzodiazepine receptor 28 (PBR28), a noninvasive measure reflecting the number of activated microglia on brain positron emission tomography (PET), was significantly greater in the GM of patients with schizophrenia and individuals at ultra-high risk of psychosis (i.e., unmedicated individuals with sub-clinical symptoms) than in matched healthy controls. Moreover, this ratio correlated positively with the severity of symptoms in patients with schizophrenia39. Similarly, another PET study showed increased TSPO ([11 C]PBR28) binding in patients with schizophrenia, correlated negatively with the GM volume40. These studies provided evidence that microglial activity is increased in individuals with schizophrenia and those at ultra-high risk of psychosis, and that microglia-mediated neuroinflammation is associated with the risk of psychosis, and possibly schizophrenia, development in later life39,40. However, PET studies conducted with different TSPO radioligands have yielded different results for patients with schizophrenia and individuals at high risk of psychosis40,41,42. For instance, Hafizi et al. performed PET imaging study using TSPO radioligand found no difference in the microglial activity of untreated patients experiencing their first psychotic episodes and healthy controls41 in a study in which [18 F]FEPPA was used as the radioligand. In addition to the radioligand difference, such differences may be related to the examination of small samples and the inclusion of patients taking atypical antipsychotics or with schizophrenia of different stages.
More recently, Gober et al.43 examined microglial activity and morphological alterations postmortem in the brains of 16 patients with schizophrenia and 13 controls through density quantification and three-dimensional reconstruction for multiple regions of interest (temporal, frontal, and subcortical WM regions; cingulate cortical GM; and anterior corpus callosum). They revealed increased microglial density in the cortical GM, temporal, and frontal regions in patients with schizophrenia43. The main morphological alterations detected in these patients were region-dependent increases in microglial soma size43. In another postmortem study, De Picker et al. reported that the expression of microglial Fc gamma (Fcγ) receptors, including CD64 (Fcγ RI) and CD64/human leukocyte antigen-DR isotype, was increased in the dorsal prefrontal cortex of patients with schizophrenia44. Considering this finding, together with earlier postmortem brain imaging and histological findings from various research groups8,10,11,13, which may be affected by limitations and are inconsistent, we are inclined to infer that microglial activation is abnormally excessive in a subset of patients with schizophrenia.
Potential role of microglial activation in schizophrenia-related cognitive deficits
Microglial activation is a hallmark of neuroinflammation that occurs predominantly in brain regions related closely to memory, such as the hippocampus8,9,10,11. Activated microglia produce and secrete key proinflammatory cytokines, including IL-6, IL-1β, and TNF-α12,13. They also release free radicals, such as reactive oxygen and nitrogen species, which are well-recognized toxic factors contributing to cognitive degeneration. Based on this knowledge, a better understanding of the pathophysiological mechanisms of microglial activation and related neuroinflammation in schizophrenia is anticipated to lead to the identification of microglia-targeting novel therapeutics. In view of the high degree of schizophrenia heritability, which accounts for approximately 60–80% of cases of this disorder, genome-wide association studies have been conducted. The largest such study to date resulted in the identification of 108 schizophrenia-associated genetic loci, including a major histocompatibility complex locus on chromosome 6, related most significantly to schizophrenia45. Most recently, Corley and colleagues14 identified microglia-expressed risk-related genetic variants affecting three cognitive domains (general cognitive ability, episodic memory, and working memory) in patients with schizophrenia. They reported that higher microglial PGSs, used as a measure of schizophrenia risk–associated microglial gene expression, were associated with worse cognitive impairment and lesser GMVs in patients with schizophrenia14. These findings provide direct evidence that microglia-expressed genes contribute to cognitive impairment in schizophrenia14.
Microglial activation has been linked clearly to schizophrenia-related cognitive dysfunction, and rapid progress has been made in the identification of microglia-expressed genetic variants and the GM-mediated association between microglial activation and cognitive impairment in schizophrenia. In contrast to age-related cognitive impairments, such as Alzheimer’s disease, in which roughly three times more WMV than GMV is lost, the loss of GMV is the predominant brain structural change in schizophrenia. Research on correlations of microglia-expressed genes, molecular pathways, and brain structural and functional imaging alterations with cognitive impairment is in its infancy, and such investigation may facilitate the elucidation of pathological mechanisms and thereby aid the development of novel schizophrenia treatments.
Roles of microglial gene expression in microglial activation–mediated cognitive deficits, especially memory impairment, in schizophrenia
Corley et al.14 were the first to profile all microglia-expressed genes and variations and to assess their associations with cognitive function in patients with schizophrenia relative to that in matched healthy controls. They identified complement-related genes associated with cognition in schizophrenia14, consistent with previous findings46,47,48,49,50. Earlier genetic association studies revealed that complement component 446,47, the complement-regulating genes CUB and Sushi Multiple Domains 1 and 249, and complement factor H, a regulator of the complement activation gene cluster50, were associated with cognitive function, especially memory, in patients with schizophrenia. Excessive microglial activation, but not tau pathology, has also been observed to adversely affect memory function in patients with Alzheimer’s disease, with an independent association between aberrant microglial activation and memory impairment51; this excessive activation has been demonstrated to co-occur with brain structural changes and memory deficits52. Corley et al.14 calculated PGSs, estimates of the genetic risk of a disease or trait, for the schizophrenia-related microglial gene set (SZ-PGSs). These scores predicted variation in measures of cognition (e.g., full-scale IQ, performance IQ, memory) relative to healthy controls across three domains: general cognitive ability, episodic memory, and working memory14. Furthermore, higher microglial SZ-PGSs correlated with worse cognitive performance and the strongest association was observed for memory14. These results are in line with the previous finding that memory function impairment is the most consistently observed schizophrenia-related cognitive impairment53. These studies have provided scientific evidence supporting the association between greater microglial polygenic risk and worse cognitive performance, especially memory function, in patients with schizophrenia. Unlike microglial SZ-PGSs, astroglial SZ-PGSs were not associated with cognitive performance in patients with schizophrenia14, suggesting that this association is specific to microglia. Few studies to date have involved the examination of the relationship between brain structure and microglial abnormalities; Corley et al.’s14 findings suggest that microglial overactivation is linked to brain structural (i.e., GMV) and functional (i.e., cognitive processing) changes, and that the GMV mediates the association between microglial SZ-PGSs and cognitive performance. Numerous neuroimaging findings support the notion that abnormal GMV alterations in the whole brain form the neural basis of cognitive impairment1,53. We found that the baseline global GMV in drug-naïve patients experiencing their first episodes of schizophrenia was associated with the severity of cognitive deterioration after 2 years of treatment with antipsychotic drugs18. Collectively, these findings suggest that the GMV mediates the association between the microglial SZ-PGS and cognitive impairment in schizophrenia.
Antipsychotic drugs may affect microglial activation in patients with schizophrenia
At present, evidence from clinical studies is insufficient to determine the effect of antipsychotic drugs on the cognitive ability of patients with schizophrenia. In a recent study, we demonstrated that global GMV alterations at baseline in drug-naïve patients experiencing their first episodes of schizophrenia were associated with the severity of cognitive alterations [evaluated using the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) consensus cognitive battery and global deficit score] after 2 years of antipsychotic treatment, and that cognitive impairment had worsened from baseline in these patients after antipsychotic therapy of adequate dosage and duration18.
Clinical data have not clarified the effect of antipsychotic agents on microglial cells in the brain.54 In-vivo neuroimaging and postmortem studies of patients with schizophrenia, as well as animal models of schizophrenia, have suggested that antipsychotic agent exposure affects the microglia in the brain54. For instance, Cotel et al. reported that chronic exposure to clinically comparable antipsychotic (i.e., haloperidol and olanzapine) doses may alter the density and morphology of microglia in the rat brain55. The molecular mechanisms underlying these effects, and the clinical relevance of the observed beneficial and side effects of antipsychotic drug regimens, remain unclear; further investigation is warranted54,55.
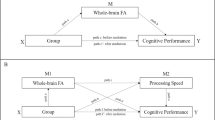
We propose a potential mechanism of action underlying the relationship between microglial activation and cognitive impairment in patients with schizophrenia (Fig. 1). Stressful psychological and medical (e.g., viral infection, traumatic brain injury) events, which usually precede the onset of psychotic symptoms in patients with schizophrenia and are considered to be important environmental risk factors for the disease, may induce the activation of resting microglia, which release proinflammatory cytokines and free radicals, demonstrated to cause brain structural abnormalities (i.e., GMV loss, especially in memory-processing brain regions)56,57,58,59. Genetic factors may also increase the risk of microglial activation in schizophrenia60,61,62,63,64,65,66. The microglia-related genes and genetic variants associated with schizophrenia are summarized in Table 1. Inhibition of microglial activity could be achieved via microglial inhibitors, such as minocycline and other natural products, or the targeting of microglia-expressed receptors, including the glucagon-like peptide-1 receptor (GLP-1R) and α7 nicotinic acetylcholine receptor (α7nAChR) agonists. This approach holds promise as a potential therapeutic intervention to improve cognition in patients with schizophrenia.
Microglial activation in the brain is induced by various stressful events, mainly psychological stress and events such as viral infection or traumatic brain injury, which usually occur prior to the onset of psychotic symptoms in schizophrenia. In addition, genetic factors [i.e., complement component (C4) variation and those affecting microglial cells in schizophrenia] may increase the risk of excessive microglial activation. Activated microglia produce and release key pro-inflammatory cytokines and free radicals, which have been shown to cause brain structural abnormalities; higher levels of these substances are associated with lower gray matter volumes, especially in brain regions responsible for memory and other cognitive functions. Microglial activation may thus be an important contributor to the development and progression of cognitive impairment in schizophrenia. Its inhibition through the use of microglial inhibitors, such as minocycline and natural products, or the targeting of microglia-expressed receptors, such as with GLP-1R or α7nAChR agonists, holds promise as a potential therapeutic intervention to improve the cognitive function of patients with schizophrenia. GLP-1R, glucagon-like peptide-1 receptor; α7nAChR, α7 nicotinic acetylcholine receptor; IL, interleukin; TNF, tumor necrosis factor.
Implications for preventive and therapeutic strategies, and future research directions
Mild to severe cognitive impairment, which affects the majority of patients with schizophrenia, including those taking antipsychotic agents, poses mechanistic and therapeutic challenges15,18,67,68. The mechanisms underlying the development and progression of cognitive deficits in patients with schizophrenia are complex. Recent advances in the understanding of the connection between excessive microglial activation, especially in brain regions involved in memory, and schizophrenia-associated cognitive impairment have provided evidence that the suppression of such activation or remodeling of activated microglia may improve cognitive performance in patients with schizophrenia. We also postulate that the inhibition of microglial activation may prevent the development of cognitive decline before the manifestation of psychotic-like symptoms in individuals at high risk of schizophrenia, such as those with first-degree relatives with the disease. Based on the most recent findings that the microglial SZ-PGS predicts variation in measures of cognition across three domains (general cognitive ability, episodic memory, and working memory), and that it correlates inversely with cognitive ability, especially memory function, the most commonly impaired cognitive domain in patients with schizophrenia14, the exploration of whether the inhibition of microglial activation in individuals at high risk (according to the SZ-PGS) can prevent the development of cognitive decline at the time of the first psychotic episode, in the prodromal stage, or even before psychotic-like symptom onset would be worthwhile.
Microglial inhibitors, including minocycline and natural products (e.g., apigenin, fisetin, and curcumin), show promise in the treatment of cognitive impairment associated with neuropsychiatric disorders, including schizophrenia69. Minocycline, a classical semi-synthetic tetracycline antibiotic with good brain infusion, is used most widely to inhibit microglial overactivation. Clinical studies have demonstrated that the use of minocycline as an add-on drug in combination with antipsychotic medications alleviates negative symptoms (lessening or absence of thoughts and behaviors in relation to interest, motivation, and/or emotional expression) in patients with schizophrenia70,71,72,73,74,75. In an animal model of schizophrenia, minocycline improved the cognitive impairment induced by MK-801, an N-methyl-D-aspartate (NMDA) receptor antagonist75. However, concerns have been raised about the detrimental effects of the minocycline treatment, including the promotion of extensive neuronal cell death, disruption of subventricular zone neurogenesis, and induction of synaptic pruning in early postnatal and adolescent rodent brains74.
The adverse effects of the inhibition of microglial activation on cognitive impairment might be diminished by the targeting of microglia-expressed receptors (e.g., GLP-1R and α7nAChR agonists), although few studies on this topic have been conducted with patients with schizophrenia or animal models of the disease. Activated microglial cells are of two subtypes with distinct polarization states: the inflammation-induced M1 phenotype and the immunoregulatory M2 phenotype76,77. The modulation of microglial polarization has been demonstrated to attenuate neural inflammation–associated pathological events78. However, whether microglial phenotype remodeling has a beneficial impact on schizophrenia-related cognitive impairment remains unexplored.
GLP-1, an endogenous enteric peptide, has been shown to play roles in human health and disease through the facilitation of insulin secretion79. Various GLP-1R agonists cross the blood–brain barrier, reduce neuronal inflammation, and protect against the cognitive symptoms of Alzheimer’s disease80,81. In in-vitro and in-vivo studies, Qian and colleagues82 showed that a GLP-1R agonist changed activated M1 microglia to the M2 subtype, and thus is a potential therapeutic agent for the attenuation of cognitive impairment in patients with schizophrenia.
α7nAChR is expressed widely in neurons and microglia in the brain83. As the activation of microglia-expressed α7nAChR induces anti-inflammatory effects, this receptor has been proposed as a promising target for the prevention and treatment of cognitive impairment in patients with psychiatric disorders such as schizophrenia83,84. In a phase-II clinical trial, Keefe and colleagues85 assessed the efficacy of encenicline, a selective α7nAChR agonist, in the treatment of cognitive impairment in patients with schizophrenia. The cognitive performance was evaluated using the Overall Cognition Index as the primary endpoint and the Schizophrenia Cognition Rating Scale total score; MATRICS Consensus Cognitive Battery score; Positive and Negative Syndrome Scale total, subscale, and cognition factor scores; and Schizophrenia Cognition Rating Scale global rating as secondary endpoints85. A 12-week encenicline regimen appeared to improve cognition in a clinically meaningful manner relative to placebo85. In two phase-III clinical trials, however, encenicline failed to achieve the primary CogState overall cognition index endpoint in patents with schizophrenia86. As the C4 genetic variant is associated with a high risk of microglial activation, clinical trials examining the efficacy of encenicline in improving cognitive impairment in patients with schizophrenia and this variant should be conducted.
Sodium benzoate, a metabolite of cinnamon and widely used food preservative, has been shown to reduce the microglial inflammatory response in mice87. In randomized, double-blind, placebo-controlled clinical trials, adjunct treatment with sodium benzoate (1 g/day) alone and in combination with sarcosine resulted in improved cognition (processing speed and visual learning), with good tolerance and favorable safety profiles, in patients with schizophrenia88,89.
Future directions for microglia-targeting strategies involve the examination of the therapeutic potential of drugs such as minocycline and GLP-1R agonists such as tirzepatide (a dual agonist of the receptors of two insulin-sensitizing polypeptides, GLP-1 and glucose-dependent insulinotrophic polypeptide, recently approved as an adjunct to diet and exercise for the treatment of diabetes, obesity, and non-alcoholic fatty liver disease) in terms of the remodeling of activated microglia from the M1 to the M2 phenotype Future clinical studies should also be conducted with suitable cohorts of patients with schizophrenia, such as those with the C4 variant, associated with a high risk of microglial activation. In view of sex differences in the epidemiology and pathology of schizophrenia, the incidence of which is moderately higher in males than in females, sex-specific genetic factors need to be considered when planning future etiological and clinical studies of cognitive impairment in patients with this disease.
Conclusions
In conclusion, microglia, a unique lineage of macrophages in the brain, play at least a partial role in cognitive impairment in schizophrenia. Although current knowledge about the role of microglial activation in the onset, development, and worsening of cognitive deficits in patients with schizophrenia remains very limited, we propose a hypothetical mechanism of the action of microglia in the pathogenesis of cognitive impairment in schizophrenia based on existing findings (Fig. 1). Stressful events (i.e., psychological stress), known as important environmental risk factors for schizophrenia, may trigger the activation of resting microglia. These activated cells produce proinflammatory cytokines and free radicals, which may be associated with key brain structural changes, mainly in the GMV, particularly in memory-processing areas of the brain. Thus, microglial activation may be an important factor for cognitive impairment in schizophrenia. Its inhibition through the use of microglial inhibitors or targeting of microglia-expressed receptors could be a novel strategy for the treatment or prevention of cognitive deficits in patients with schizophrenia. In future clinical studies, investigation of the therapeutic effects of the inhibition of microglial activation in more suitable cohorts of patients with schizophrenia or individuals with first-degree relatives with schizophrenia and a high risk of microglial activation, such as those with the complement component C4 variant, would be of interest.
References
Jauhar, S., Johnstone, M. & McKenna, P. J. Schizophrenia. Lancet. 399, 473–486 (2022).
Heinrichs, R. W. & Zakzanis, K. K. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 12, 426–445 (1998).
Lewandowski, K. E., Cohen, B. M. & Ongur, D. Evolution of neuropsychological dysfunction during the course of schizophrenia and bipolar disorder. Psychol. Med. 41, 225–241 (2011).
Ormel, P. R. et al. A characterization of the molecular phenotype and inflammatory response of schizophrenia patient-derived microglia-like cells. Brain Behav. Immun. 90, 196–207 (2020).
Salter, M. W. & Stevens, B. Microglia emerge as central players in brain disease. Nat. Med. 23, 1018–1027 (2017).
Sellgren, C. M. et al. Increased synapse elimination by microglia in schizophrenia patient-derived models of synaptic pruning. Nat. Neurosci. 22, 374–385 (2019).
Howes, O. D. & McCutcheon, R. Inflammation and the neural diathesis-stress hypothesis of schizophrenia: a reconceptualization. Transl. Psychiatry. 7, e1024 (2017).
Doorduin, J. et al. Neuroinflammation in schizophrenia-related psychosis: a PET study. J. Nucl. Med. 50, 1801–1807 (2009).
Trépanier, M. O., Hopperton, K. E., Mizrahi, R., Mechawar, N. & Bazinet, R. P. Postmortem evidence of cerebral inflammation in schizophrenia: a systematic review. Mol. Psychiatry. 21, 1009–1026 (2016).
Hill, S. L., Shao, L. & Beasley, C. L. Diminished levels of the chemokine fractalkine in post-mortem prefrontal cortex in schizophrenia but not bipolar disorder. World J. Biol. Psychiatry. 22, 94–103 (2021).
Petrasch-Parwez, E. et al. Lateralization of increased density of Iba1-immunopositive microglial cells in the anterior midcingulate cortex of schizophrenia and bipolar disorder. Eur. Arch. Psychiatry Clin. Neurosci. 270, 819–828 (2020).
Wu, D. et al. Association of peripheral cytokine levels with cerebral structural abnormalities in schizophrenia. Brain Res. 1724, 146463 (2019).
Fillman, S. G. et al. Elevated peripheral cytokines characterize a subgroup of people with schizophrenia displaying poor verbal fluency and reduced Broca’s area volume. Mol. Psychiatry 21, 1090–1098 (2016).
Corley, E. et al. Microglial-expressed genetic risk variants, cognitive function and brain volume in patients with schizophrenia and healthy controls. Transl. Psychiatry 11, 490 (2021).
Gebreegziabhere, Y., Habatmu, K., Mihretu, A., Cella, M. & Alem, A. Cognitive impairment in people with schizophrenia: an umbrella review. Eur. Arch. Psychiatry Clin. Neurosci. 272, 1139–1155 (2022).
Keefe, R. S., Eesley, C. E. & Poe, M. P. Defining a cognitive function decrement in schizophrenia. Biol. Psychiatry 57, 688–691 (2005).
Fatouros-Bergman, H., Cervenka, S., Flyckt, L., Edman, G. & Farde, L. Meta-analysis of cognitive performance in drug-naïve patients with schizophrenia. Schizophr Res. 158, 156–162 (2014).
Zhuo, C. et al. Baseline global brain structural and functional alterations at the time of symptom onset can predict subsequent cognitive deterioration in drug-naïve first-episode schizophrenia patients: evidence from a follow-up study. Front. Psychiatry 13, 1012428 (2022).
McCleery, A. & Nuechterlein, K. H. Cognitive impairment in psychotic illness: prevalence, profile of impairment, developmental course, and treatment considerations. Dialogues Clin. Neurosci. 21, 239–248 (2019).
Allen, D. N., Goldstein, G. & Warnick, E. A consideration of neuropsychologically normal schizophrenia. J Int. Neuropsychol. Soc. 9, 56–63 (2003).
González-Blanch, C. et al. Cognitive functioning in the early course of first-episode schizophrenia spectrum disorders: timing and patterns. Eur. Arch. Psychiatry Clin. Neurosci. 256, 364–371 (2006).
Smeland, O. B. et al. Genome-wide analysis reveals extensive genetic overlap between schizophrenia, bipolar disorder, and intelligence. Mol. Psychiatry 25, 844–853 (2020).
Smeland, O. B., Frei, O., Dale, A. M. & Andreassen, O. A. The polygenic architecture of schizophrenia - rethinking pathogenesis and nosology. Nat Rev Neurol. 16, 366–379 (2020).
Green, M. F. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry. 67, 3–8 (2006).
Kahn, R. S. & Keefe, R. S. Schizophrenia is a cognitive illness: time for a change in focus. JAMA Psychiatry 70, 1107–1112 (2013).
Simonsen, C. et al. Neurocognitive dysfunction in bipolar and schizophrenia spectrum disorders depends on history of psychosis rather than diagnostic group. Schizophr. Bull. 37, 73–83 (2011).
Barch, D. M. Neuropsychological abnormalities in schizophrenia and major mood disorders: similarities and differences. Curr. Psychiatry Rep. 11, 313–319 (2009).
Fusar-Poli, P. et al. Cognitive functioning in prodromal psychosis: a meta-analysis. Arch Gen Psychiatry. 69, 562–571 (2012).
Reichenberg, A. et al. Static and dynamic cognitive deficits in childhood preceding adult schizophrenia: a 30-year study. Am. J. Psychiatry 167, 160–169 (2010).
Gale, C. R. et al. Is bipolar disorder more common in highly intelligent people? A cohort study of a million men. Mol. Psychiatry 18, 190–194 (2013).
Tiihonen, J. et al. Premorbid intellectual functioning in bipolar disorder and schizophrenia: results from a cohort study of male conscripts. Am. J. Psychiatry 162, 1904–1910 (2005).
MacCabe, J. H. et al. Excellent school performance at age 16 and risk of adult bipolar disorder: national cohort study. Br. J. Psychiatry 196, 109–115 (2010).
Bowie, C. R. & Harvey, P. D. Cognition in schizophrenia: impairments, determinants, and functional importance. Psychiatr. Clin. North Am. 28, 613–633 (2005).
Braff, D. L. Information processing and attention dysfunctions in schizophrenia. Schizophr. Bull. 19, 233–259 (1993).
Kayman, D. J. & Goldstein, M. F. Cognitive deficits in schizophrenia. Curr. Transl. Geriatr. Gerontol. Rep. 1, 45–52 (2012).
Petanjek, Z. et al. Extraordinary neoteny of synaptic spines in the human prefrontal cortex. Proc. Natl Acad. Sci. USA 108, 13281–13286 (2011).
Cannon, T. D. How schizophrenia develops: cognitive and brain mechanisms underlying onset of psychosis. Trends Cogn. Sci. 19, 744–756 (2015).
Sekar, A. et al. Schizophrenia risk from complex variation of complement component 4. Nature 530, 177–183 (2016).
Bloomfield, P. S. et al. Microglial activity in people at ultra high risk of psychosis and in schizophrenia: an [(11)C]PBR28 PET brain imaging study. Am. J. Psychiatry 173, 44–52 (2016).
Selvaraj, S. et al. Brain TSPO imaging and gray matter volume in schizophrenia patients and in people at ultra high risk of psychosis: An [(11)C]PBR28 study. Schizophr. Res. 195, 206–214 (2018).
Hafizi, S. et al. Imaging microglial activation in untreated first-episode psychosis: a pet study with [(18)F]FEPPA. Am J Psychiatry. 174, 118–124 (2017).
Conen, S. et al. Neuroinflammation as measured by positron emission tomography in patients with recent onset and established schizophrenia: implications for immune pathogenesis. Mol. Psychiatry 26, 5398–5406 (2021).
Gober, R. et al. Microglia activation in postmortem brains with schizophrenia demonstrates distinct morphological changes between brain regions. Brain Pathol. 32, e13003 (2022).
De Picker, L. J. et al. Immune environment of the brain in schizophrenia and during the psychotic episode: A human post-mortem study. Brain Behav. Immun. 97, 319–327 (2021).
Schizophrenia Working Group of the Psychiatric Genomics Consortium. Biological insights from 108 schizophrenia-associated genetic loci. Nature 511, 421–427 (2014).
Donohoe, G. et al. Genetically predicted complement component 4A expression: effects on memory function and middle temporal lobe activation. Psychol. Med. 48, 1608–1615 (2018).
Holland, J. F. et al. Beyond C4: analysis of the complement gene pathway shows enrichment for IQ in patients with psychotic disorders and healthy controls. Genes Brain Behav. 18, e12602 (2019).
Donohoe, G. et al. Neuropsychological effects of the CSMD1 genome-wide associated schizophrenia risk variant rs10503253. Genes Brain Behav. 12, 203–209 (2013).
Athanasiu, L. et al. A genetic association study of CSMD1 and CSMD2 with cognitive function. Brain Behav. Immun. 61, 209–216 (2017).
Zhang, C., Lv, Q., Fan, W., Tang, W. & Yi, Z. Influence of CFH gene on symptom severity of schizophrenia. Neuropsychiatr. Dis. Treat. 13, 697–706 (2017).
Zou, J. et al. Microglial activation, but not tau pathology, is independently associated with amyloid positivity and memory impairment. Neurobiol Aging. 85, 11–21 (2020).
Malpetti, M. et al. Microglial activation and tau burden predict cognitive decline in Alzheimer’s disease. Brain 143, 1588–1602 (2020).
Khalil, M., Hollander, P., Raucher-Chéné, D., Lepage, M. & Lavigne, K. M. Structural brain correlates of cognitive function in schizophrenia: a meta-analysis. Neurosci. Biobehav. Rev. 132, 37–49 (2022).
Dinesh, A. A., Islam, J., Khan, J., Turkheimer, F. & Vernon, A. C. Effects of antipsychotic drugs: cross talk between the nervous and innate immune system. CNS Drugs 34, 1229–1251 (2020).
Cotel, M. C. et al. Microglial activation in the rat brain following chronic antipsychotic treatment at clinically relevant doses. Eur. Neuropsychopharmacol. 25, 2098–2107 (2015).
Holland, J. F. et al. Effects of early life adversity on immune function and cognitive performance: results from the ALSPAC cohort. Soc. Psychiatry Psychiatr. Epidemiol. 55, 723–733 (2020).
Moussa-Tooks, A. B. et al. Cerebellar structure and cognitive ability in psychosis. Biol. Psychiatry 92, 385–395 (2022).
Shelton, H. W. et al. The effects of a novel inhibitor of tumor necrosis factor (TNF) alpha on prepulse inhibition and microglial activation in two distinct rodent models of schizophrenia. Behav. Brain Res. 406, 113229 (2021).
Lesh, T. A. et al. Cytokine alterations in first-episode schizophrenia and bipolar disorder: relationships to brain structure and symptoms. J. Neuroinflammation 15, 165 (2018).
Dean, B. et al. Different changes in cortical tumor necrosis factor-α-related pathways in schizophrenia and mood disorders. Mol Psychiatry. 18, 767–773 (2013).
Francisco, R. D., Fernando, V., Norma, E., Madai, M. E. & Marcelo, B. Glial changes in schizophrenia: Genetic and epigenetic approach. Indian J Psychiatry. 64, 3–12 (2022).
Kadasah, S., Arfin, M., Rizvi, S., Al-Asmari, M. & Al-Asmari, A. Tumor necrosis factor-α and -β genetic polymorphisms as a risk factor in Saudi patients with schizophrenia. Neuropsychiatr. Dis. Treat. 13, 1081–1088 (2017).
Suchanek-Raif, R. et al. Association Study of Tumor Necrosis Factor Receptor 1 (TNFR1) gene polymorphisms with schizophrenia in the polish population. Mediators Inflamm. 2017, 6016023 (2017).
Venugopal, D. et al. Impact of antipsychotic treatment on methylation status of Interleukin-6 [IL-6] gene in Schizophrenia. J. Psychiatr. Res. 104, 88–95 (2018).
Xiu, M. et al. The TNF-alpha gene −1031T>C polymorphism is associated with onset age but not with risk of schizophrenia in a Chinese population. Neuropsychology. 33, 482–489 (2019).
Zakharyan, R. et al. Interleukin-6 promoter polymorphism and plasma levels in patients with schizophrenia. Tissue Antigens 80, 136–142 (2012).
Harvey, P. D. et al. Cognitive dysfunction in schizophrenia: an expert group paper on the current state of the art. Schizophr. Res. Cogn. 29, 100249 (2022).
Huang, B. J. et al. Neurocognitive trajectories and their clinical implications in first-episode schizophrenia after one year of antipsychotic treatment. Schizophr. Res. 241, 292–297 (2022).
Bai, Z., Chen, G., Li, W., Hou, Y. & Li, N. Natural Inhibitors on Over-Activation of Microglia from Herbals. Chem Pharm Bull (Tokyo). 67, 640–647 (2019).
Miyaoka, T. et al. Possible antipsychotic effects of minocycline in patients with schizophrenia. Prog. Neuropsychopharmacol. Biol. Psychiatry 31, 304–307 (2007).
Chaudhry, I. B. et al. Minocycline benefits negative symptoms in early schizophrenia: a randomised double-blind placebo-controlled clinical trial in patients on standard treatment. J. Psychopharmacol. 26, 1185–1193 (2012).
Liu, F. et al. Minocycline supplementation for treatment of negative symptoms in early-phase schizophrenia: a double blind, randomized, controlled trial. Schizophr. Res. 153, 169–176 (2014).
Kelly, D. L. et al. Adjunctive minocycline in clozapine-treated schizophrenia patients with persistent symptoms. J. Clin. Psychopharmacol. 35, 374–381 (2015).
Inta, D., Lang, U. E., Borgwardt, S., Meyer-Lindenberg, A. & Gass, P. Microglia activation and schizophrenia: lessons from the effects of minocycline on postnatal neurogenesis, neuronal survival and synaptic pruning. Schizophr. Bull. 43, 493–496 (2017).
Levkovitz, Y., Levi, U., Braw, Y. & Cohen, H. Minocycline, a second-generation tetracycline, as a neuroprotective agent in an animal model of schizophrenia. Brain Res. 1154, 154–162 (2007).
Hu, X. et al. Microglial and macrophage polarization—new prospects for brain repair. Nat. Rev. Neurol. 11, 56–64 (2015).
Akhmetzyanova, E., Kletenkov, K., Mukhamedshina, Y. & Rizvanov, A. Different Approaches to Modulation of Microglia Phenotypes After Spinal Cord Injury. Front Syst Neurosci. 13, 37 (2019).
Zhuang, X. et al. Molecular hydrogen attenuates sepsis-induced neuroinflammation through regulation of microglia polarization through an mTOR-autophagy-dependent pathway. Int. Immunopharmacol. 81, 106287 (2020).
Andersen, A., Lund, A., Knop, F. K. & Vilsbøll, T. Glucagon-like peptide 1 in health and disease. Nat. Rev. Endocrinol. 14, 390–403 (2018).
Shan, Y. et al. The glucagon-like peptide-1 receptor agonist reduces inflammation and blood-brain barrier breakdown in an astrocyte-dependent manner in experimental stroke. J. Neuroinflammation 16, 242 (2019).
Talbot, K. & Wang, H. Y. The nature, significance, and glucagon-like peptide-1 analog treatment of brain insulin resistance in Alzheimer’s disease. Alzheimers Dement. 10, S12–S25 (2014).
Qian, Z. et al. Activation of glucagon-like peptide-1 receptor in microglia attenuates neuroinflammation-induced glial scarring via rescuing Arf and Rho GAP adapter protein 3 expressions after nerve injury. Int. J. Biol. Sci. 18, 1328–1346 (2022).
Xu, Z. Q., Zhang, W. J., Su, D. F., Zhang, G. Q. & Miao, C. Y. Cellular responses and functions of α7 nicotinic acetylcholine receptor activation in the brain: a narrative review. Ann. Transl. Med. 9, 509 (2021).
Shi, S. et al. Gx-50 Inhibits Neuroinflammation via α7 nAChR Activation of the JAK2/STAT3 and PI3K/AKT Pathways. J. Alzheimers Dis. 50, 859–871 (2016).
Keefe, R. S. et al. Randomized, double-blind, placebo-controlled study of encenicline, an α7 nicotinic acetylcholine receptor agonist, as a treatment for cognitive impairment in schizophrenia. Neuropsychopharmacology 40, 3053–3060 (2015).
Garay, R. P. et al. Therapeutic improvements expected in the near future for schizophrenia and schizoaffective disorder: an appraisal of phase III clinical trials of schizophrenia-targeted therapies as found in US and EU clinical trial registries. Expert Opin. Pharmacother. 17, 921–936 (2016).
Brahmachari, S., Jana, A. & Pahan, K. Sodium benzoate, a metabolite of cinnamon and a food additive, reduces microglial and astroglial inflammatory responses. J. Immunol. 183, 5917–5927 (2009).
Lane, H. Y. et al. Add-on treatment of benzoate for schizophrenia: a randomized, double-blind, placebo-controlled trial of D-amino acid oxidase inhibitor. JAMA Psychiatry 70, 1267–1275 (2013).
Lin, C. Y. et al. Adjunctive sarcosine plus benzoate improved cognitive function in chronic schizophrenia patients with constant clinical symptoms: a randomised, double-blind, placebo-controlled trial. World J. Biol. Psychiatry 18, 357–368 (2017).
Funding
This work was supported by grants from the National Natural Science Foundation of China (81871052, 82171503 to CJZ); the Key Projects of the Natural Science Foundation of Tianjin, China (17JCZDJC35700 to CJZ); the Tianjin Health Bureau Foundation (2014KR02 to CJZ).
Author information
Authors and Affiliations
Contributions
All authors have made substantial and intellectual contributions to researching data for this article, to discussions of content, and to writing the manuscript. Chunjun Zhuo, Chunhua Zhou, and XS were involved in the conception, drafting, reviewing, and revising of the manuscript. HT, DJ, GC, CC, ZC, JP, LC performed the literature search and the extraction of the data. All authors contributed to and have approved the final paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhuo, C., Tian, H., Song, X. et al. Microglia and cognitive impairment in schizophrenia: translating scientific progress into novel therapeutic interventions. Schizophr 9, 42 (2023). https://doi.org/10.1038/s41537-023-00370-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-023-00370-z