Abstract
Tobacco control policies can protect child health. We hypothesised that the parallel introduction in 2008 of smoke-free restaurants and bars in the Netherlands, a tobacco tax increase and mass media campaign, would be associated with decreases in childhood wheezing/asthma, respiratory tract infections (RTIs), and otitis media with effusion (OME) presenting in primary care. We conducted an interrupted time series study using electronic medical records from the Dutch Integrated Primary Care Information database (2000–2016). We estimated step and slope changes in the incidence of each outcome with negative binomial regression analyses, adjusting for underlying time-trends, seasonality, age, sex, electronic medical record system, urbanisation, and social deprivation. Analysing 1,295,124 person-years among children aged 0–12 years, we found positive step changes immediately after the policies (incidence rate ratio (IRR): 1.07, 95% CI: 1.01–1.14 for wheezing/asthma; IRR: 1.16, 95% CI: 1.13–1.19 for RTIs; and IRR: 1.24, 95% CI: 1.14–1.36 for OME). These were followed by slope decreases for wheezing/asthma (IRR: 0.95/year, 95% CI: 0.93–0.97) and RTIs (IRR: 0.97/year, 95% CI: 0.96–0.98), but a slope increase in OME (IRR: 1.05/year, 95% CI: 1.01–1.09). We found no clear evidence of benefit of changes in tobacco control policies in the Netherlands for the outcomes of interest. Our findings need to be interpreted with caution due to substantial uncertainty in the pre-legislation outcome trends.
Similar content being viewed by others
Introduction
Tobacco smoking remains the world’s most important preventable cause of morbidity and premature mortality1. Passive exposure to tobacco smoke, or second-hand smoke (SHS) exposure, is responsible for more than one million deaths per year globally, including over 50,000 children under the age of 102. Exposure to SHS also increases the risk of a range of adverse health outcomes in early life, including wheezing/asthma, respiratory tract infections (RTIs), and otitis media with effusion (OME)3,4,5,6,7. Substantial evidence now indicates that children benefit from the implementation of comprehensive tobacco control policies—for example, laws that prohibit smoking in indoor public places and workplaces8,9. In a recent systematic review and meta-analysis, including data on over 27 million children, we demonstrated that the introduction of smoke-free legislation was associated with a −18% decrease in hospital attendance for lower RTIs (95% confidence interval (CI) −33 to −4), and a −10% decrease in hospital attendance for asthma (95% CI −17 to −3) among children8. Effects on childhood OME have been assessed in one study, but no significant changes were found10.
Most of this research has focused on severe childhood health outcomes such as hospitalisations, which reflect only part of the burden of disease caused by tobacco smoke exposure. Children with milder respiratory symptoms are more likely to be diagnosed in primary care. There is inconclusive evidence on whether respiratory health outcomes in primary care are directly affected by tobacco control policies. We are aware of one study that aimed to determine the effects of a comprehensive smoke-free law on adverse paediatric respiratory outcomes in primary care in the UK11. This found no significant changes in wheezing/asthma and RTI diagnoses in children in primary care after the introduction of national comprehensive smoke-free legislation, whereas other studies did find substantial reductions in hospitalisations for these outcomes in England and Scotland12,13,14. From this study, it is unclear whether outcomes in primary care are inherently less affected or not affected by smoke-free laws than outcomes in hospital care, or whether these changes have not been detected due to methodological reasons11.
In the Netherlands, about 7% of all children aged 0–11 were exposed to tobacco smoke in some way in 202015. Although the smoking prevalence among adults has decreased during the last decade, 20% of the adult Dutch population reported to smoke daily or occasionally in 2020, with the highest percentages among people of childbearing age (aged 18–49)15. Following on from regulation introduced in 2004 which prohibited smoking in most enclosed workplaces and public places, the Dutch government introduced legislation in 2008 mandating smoke-free restaurants and bars. This introduction was accompanied by a tobacco tax increase and a mass media campaign. Given the overwhelming evidence linking smoke-free legislation to reduced hospitalisations for respiratory disorders among children, we were interested in whether tobacco control policies also directly affect the actual incidence of these outcomes in primary care. In this study, we examined the hypothesis that the introduction of these tobacco control policies was associated with reductions in the incidence of general practitioner (GP) diagnoses of wheezing/asthma, RTIs, and OME in children aged ≤12 years.
Results
Patient population
Between 2000 and 2016, there were 917,532 person-years at risk for wheezing/asthma, 1,295,124 person-years at risk for RTIs, and 1,245,885 person-years at risk for OME. During these at-risk periods there were 38,430 new diagnoses of wheezing/asthma, 417,597 new diagnoses of RTIs, and 19,266 new diagnoses of OME. When separately examining URTIs and LRTIs, including LRTIs that directly followed an URTI, there were 377,418 URTIs and 48,501 LRTIs. The distribution of person-years at risk and, consequently, the number of new diagnoses for all of our outcomes were heavily skewed towards the post-intervention period: most GP practices joined IPCI after the policies were introduced, resulting in roughly 10 times more person-years included in the post-intervention period (Supplementary Table 1 and Supplementary Fig. 1). Younger children (aged 0–4 years) had higher mean incidence rates of all outcomes (Table 1; Supplementary Table 2). Figures 1–3 display the monthly rates of new wheezing/asthma, RTI, and OME diagnoses over the study period. The seasonal variations of these outcomes within each year appeared to be consistent over the entire study period.
Associations between introduction of policy and outcomes
The 2008 policy changes were associated with an immediate step increase in new wheezing/asthma diagnoses (incidence rate ratio (IRR) 1.07; 95% confidence interval (CI) 1.01–1.14), followed by a slope decrease (IRR 0.95 per year; 95% CI 0.93–0.97) (Table 2). Similarly, for RTI diagnoses there was a temporary increase (IRR 1.16; 95% CI 1.13–1.19), followed by a slope decrease (IRR 0.97 per year; 95% CI 0.96–0.98). For OME incidence, the policy change was associated with both a step increase (IRR 1.24; 95% CI 1.14–1.36), and a slope increase (IRR 1.05 per year; 95% CI 1.01–1.09) (Table 2).
Both URTIs and LRTIs showed a step increase following the 2008 policy change (URTIs: IRR 1.17; 95% CI 1.14–1.20; LRTIs: IRR 1.12; 95% CI 1.05–1.19), again followed by a slope decrease (URTIs: IRR 0.98 per year; 95% CI 0.96–0.99; LRTIs: IRR 0.87 per year; 95% CI 0.85–0.89) (Table 2).
The sensitivity analyses of (1) complete cases only, (2) without urbanisation level and social deprivation, and (3) the data with imputed values for missing entries of urbanisation level and social deprivation provided results similar to the primary analyses (Supplementary Tables 3–5).
Using a counterfactual scenario, we estimated that in the first eight years following the policy change 0.68 new wheezing/asthma diagnoses (95% CI 0.65–0.71) and 0.80 new RTI diagnoses per 1000 person-months were averted (95%CI 0.64-0.97). In contrast, following the policy implementation an additional 0.47 new OME diagnoses per 1000 person-months were made during this period (95% CI 0.46–0.47).
Discussion
A policy change involving implementation of smoke-free hospitality businesses, a mass media campaign, and a tobacco tax increase in the Netherlands was followed by a temporary increase and a subsequent gradual decrease in asthma diagnoses and RTIs in children. This translated into a net reduction in the number of asthma diagnoses and RTIs over the post-implementation period. Unexpectedly, OME diagnoses among children increased following the policy. Our findings need to be interpreted with caution due to the limited amount of data in the pre-legislation period, introducing substantial uncertainty in the pre-legislation trends.
Exposure to tobacco smoke undisputedly leads to higher risk of adverse respiratory outcomes in both children and adults, including RTIs and asthma1,16. There is also substantial evidence that the implementation of comprehensive smoke-free legislation has a positive impact on hospitalisations for RTIs and asthma in both children and adults, with the more comprehensive laws being more effective8,17. The most likely pathways for these effects are reduced SHS exposure in public and in the home environment as a result of behavioural changes in society18.
Although there was a net reduction in the number of asthma and RTI cases following the policy under study, the initial temporary increases in these diagnoses as well as the sustained increase in OME diagnoses are counterintuitive against this background. A number of factors could help explain why this is the case. First, the Dutch tobacco control approach might not have been immediately effective due to its lack of comprehensiveness and its phased approach, as well as lack of compliance19. For example, whereas the WHO urges for restaurants and bars to be completely smoke-free, the Dutch law allowed for indoor smoking rooms, which have been found to be ineffective in protecting from tobacco smoke exposure20,21. Also, one year after the implementation of the smoke-free restaurants and bars law, 36% of smokers still noticed smoking in bars outside the designated smoking areas in the Netherlands, compared to 1.7% in England and 5.4% in Ireland, for example, where the national smoke-free policy included all public places with no exceptions22. Compared to 11 other countries included in the International Tobacco Control Policy Evaluation Project, Dutch people who smoked were at the time also the least knowledgeable or concerned about the harms of tobacco smoking and SHS exposure (in 2010, only 61% of them agreed that cigarette smoke is dangerous to non-smokers compared to 96% of people who smoked in France, 89% in Germany, and 83% in the UK)23. In a previous study assessing perinatal health outcomes in the Netherlands, there was a relative lack of impact of the Dutch smoke-free law as compared to England, where the law had been much more comprehensive and compliance was excellent24,25. Despite this, exposure of young children to tobacco smoke in the home, likely the primary source of exposure, decreased substantially across the study period26,27. In the absence of more detailed trends in tobacco smoke exposure in various places at the time, we lack ability to assess causality of the observed temporal association between the policy change and short-term increases in these respiratory diagnoses.
Previous research suggests that tobacco smoke exposure has a larger impact on RTI severity and asthma exacerbations than on RTI and asthma incidence per se10,28,29. In line with this, studies in England have demonstrated a positive impact of the smoke-free law on paediatric hospital admissions, but not on GP diagnoses for asthma and RTIs11,12,14. In our study, we were limited to the EMR diagnosis and medication codes registered by the GPs, and therefore had limited ability to distinguish between asthma/RTI diagnosis, treatment, or exacerbation. Similarly, we were unable to analyse Dutch national hospital admissions data due to temporal data limitations of the respective database30.
Lastly, other changes over time might have influenced our outcomes of interest that we could not correct for in our analyses. In 2006, the Dutch government introduced a fundamental reform of the health insurance system. Among many changes, this reform led to a change in the remuneration system for GPs31, a gradual increase in the supply and use of EMR systems, and the systematic use of ICPC disease codes and ATC medication codes for reimbursement. Although it is possible or even likely that coding and registering behaviour changed during our study period, we were unable to evaluate whether and how this may have affected our results. In addition, there might have been other changes affecting the incidence of our outcomes of interest over time that we are not aware of. Previous work in this field has demonstrated that lack of accounting for unanticipated breakpoints in time series may produce potentially spurious findings32. Due to the inherent restrictions of our time series as a result of the low number of GP practices contributing data pre-legislation, as outlined earlier, we did not undertake breakpoint detection in the current study.
To the best of our knowledge, this is the first study aimed at determining the association between introduction of tobacco control policies and child health outcomes in primary care in the Netherlands. We analysed over one million person-years of data while adjusting for important individual-level confounders. At the same time, it is important to note that our study has significant constraints. With the intervention being a national policy implementation, we lacked a true control group and were unable to randomise treatment allocation. Even though we have used optimal methods to evaluate this public health intervention, our study design is still quasi-experimental, and therefore inherently subject to bias33. In our attempt to capture the true association between the policy change and our selected outcomes, we adjusted our analyses for potential confounding factors that could have influenced our results. However, our data were particularly unbalanced in relation to the timing of the intervention, with very few GPs and participants contributing data to the pre-legislation period versus the post-legislation period (93,104 versus 824,428 person-years at risk for wheezing/asthma, 123,702 versus 1,171,421 person-years at risk for RTIs, and 120,719 versus 1,125,167 person-years at risk for OME). This complicated proper estimation of the pre-legislation trends and hence limited the ability of our models to reliably determine the intervention effects. In addition to the uncertainty in the parameter estimates caused by the low pre-post data ratio, our results may be biased by temporal changes in registration behaviour by GPs, as outlined earlier. This may have resulted in an underestimation of number of respiratory diseases in children in the pre-intervention period, possibly overestimating the step changes as a result.
In conclusion, there was a modest net reduction in paediatric asthma and RTI diagnoses following a national set of tobacco control policies in the Netherlands. This was however preceded by an unexpected temporary increase in diagnoses and accompanied by a sustained increase in OME diagnoses. Although the exact mechanisms underlying these observations remain unclear, limitations of the underlying data may have biased our findings.
Methods
Study design
We conducted interrupted time series (ITS) analyses to determine the associations between the implementation of the July 2008 Dutch national smoke-free restaurants and bars policy34, and changes in the incidence rates of wheezing/asthma, RTIs, and OME among children.
Setting
We used data from the Integrated Primary Care Information (IPCI) database, a longitudinal database of electronic medical records (EMRs) from primary care practices in the Netherlands. The IPCI database was founded in 1989 and is acclaimed for its comprehensive medical information35. The data in IPCI are an open cohort: GP practices and patients may enter and leave the database at any time. As the EMRs were anonymised, the geographical locations of the patients and GP practices were unknown to the researchers using these data. Details of the IPCI database have been described previously35. To perform the ITS analysis around the key year 2008 (when policy changed), we decided a priori to include data from January 2000 through December 2016.
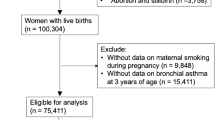
Participants
For our study, children were included if they were aged ≤12 years and were registered with a GP practice in the IPCI database for at least six consecutive months during the study period. Children who entered the GP practice as a newborn (i.e., within 6 months after birth) and who contributed at least 6 months of data were eligible. Participants were followed-up until they turned 13 years of age, changed to a GP practice not registered in IPCI, left the country, or died. The age cut-off of 12 years of age was selected to minimise the potential confounding effect of active smoking among participants.
Outcomes
Our primary outcomes of interest were the monthly incidence of new diagnoses of wheezing/asthma, RTIs, and OME. Our secondary outcomes of interest were the monthly incidence of new diagnoses of upper RTIs (URTI) and lower RTIs (LRTI).
We specified a new diagnosis of wheezing/asthma when a relevant diagnostic International Classification of Primary Care (ICPC) code was recorded in a child’s medical records and/or when a prescription for asthma-related medication was recorded in the medical records of a child who had no previous recording of wheezing/asthma diagnostic codes or asthma-related prescriptions (the relevant ICPC codes are listed in the Online Supplement). Children did not have a new diagnosis if wheezing/asthma was recorded before or on the first day of registration with an IPCI practice, as they were considered to be prevalent cases of wheezing/asthma. Asthma-related medications included selective beta-2 adrenoreceptor agonists, anticholinergics, inhalation corticosteroids, and leukotriene receptor antagonists (for details, see the Online Supplement).
Incident diagnoses of RTIs were specified when an ICPC code for either an URTI or LRTI was recorded in a child’s medical records. As most RTIs among children resolve within 15 days, we considered a new RTI diagnosis only when registered at least 21 days after any prior RTI consultation, to minimise repeated registration of GP visits for the same RTI episode36.
We defined children to have a new OME diagnosis if the relevant ICPC code was recorded in a child’s medical records and there was no prior registration of an OME code in the preceding six months. We applied this six-month window to exclude repeated GP visits for the same episode of OME as around 72% of OME cases (95% CI 68–76) in children are known to resolve spontaneously within 6 months37.
We considered separate diagnoses of URTIs and LRTIs as secondary outcomes. Similar to RTIs in general, we defined multiple visits within 14 days as belonging to the same URTI/LRTI diagnosis. However, if an URTI was followed by a LRTI within 14 days, both the URTI and LRTI were recorded as separate diagnoses.
The GPs used codes from the first edition of the ICPC to register disease diagnoses in EMRs38. Medication codes were registered using the World Health Organization’s (WHO) Anatomical Therapeutic Chemical (ATC) codes39.
Person-time at risk
A child was considered to be at risk for an outcome in a particular month if:
-
The child had no prior registration of an asthma code, including in registration of prior disease history in patients newly entering GP practice (Online Supplement) [for wheezing/asthma]
-
The child had no prior issuing of wheezing/asthma-related medication prescription, including in registration of prior medication history in patients newly entering GP practice (Online Supplement) [for wheezing/asthma]
-
No OME code was registered within the six preceding months (Online Supplement) [for OME].
Main predictor of interest
The intervention was the introduction of a law on 1 July 2008 prohibiting smoking in hospitality venues, i.e., hotels, bars and restaurants, sports, arts and culture venues, amusement arcades, tobacco shops, and international passenger transport34. This law allowed for designated indoor smoking areas34. The law was accompanied by a mass-media campaign and an 8% excise tax increase on tobacco products40.
Confounding factors
In our analyses, we adjusted for the following potential confounders: the underlying time-trend in the outcome, seasonality (i.e. month of diagnosis; categorical), age group (0–4; 5-12 years of age), sex (female; male), EMR software system (HetHIS; Medicom; MicroHIS, MicroHIS Old; Mira; Promedico ASP; Promedico VDF Old; WebHIS Zorgdossier), urbanisation level (urban: ≥1500 inhabitants per km2; rural: <1500 inhabitants per km2), and social deprivation (yes: living in an area in the bottom 5% of that year’s national list of postal codes ranked according to social deprivation; no: in the top 95% of this list).
Due to a high proportion of missing values for urbanisation and social deprivation (i.e. 35% and 13%, respectively), we re-coded missing values into a third category, i.e. urban, rural, missing for urbanisation level, and yes, no, missing for social deprivation. Urbanisation level and social deprivation were completely missing for the years 2000–2003, as registration of postal code only started in 2004.
Statistical methods
Our primary analysis was an ITS negative binomial regression analysis in which we investigated the association between the implementation of the tobacco control policies in 2008 and the change in incidence of each of our outcomes of interest. A negative binomial model (rather than a Poisson model) was adopted to account for over-dispersion (variance > mean) of case incidences over time.
Our models allowed for both an immediate change in level of the outcomes (step change) using a dichotomous time-variant dummy variable, as well as a gradual change in temporal trend of our outcomes (slope change) using an interaction term between the dummy variable and year (continuous). We accounted for seasonality (categorical variable for month) and the underlying temporal incidence trend (year as a continuous variable, centred at 1 July 2008). We modelled the underlying temporal trend via linear, quadratic, and cubic B-splines in separate models to account for possible non-linearity. We selected the optimal model using Aikaike’s and Bayesian Information Criteria (AIC and BIC, respectively). Using comparison of predicted values from our models and counterfactual models with step and slope changes set to zero, we estimated the absolute number of events averted across the post-legislation study period for each outcome. We performed all analyses using Stata SE 15.1 (Statacorp, TX).
Sensitivity analyses
In post hoc sensitivity analyses, we assessed the potential impact of the substantial proportion of children with missing postal code data on our findings via: 1. including only cases with complete data on all covariates, 2. not adjusting for urbanisation level and social deprivation, and 3. imputing values for urbanisation level and social deprivation. For the latter purpose we conducted and analysed 20 imputations of these values based on all the available variables in the dataset, using the Stata commands mi impute monotone (logit) and mi estimate.
Ethical considerations and reporting
The IPCI Governance Board approved this study (no. 03/2015). The IPCI data are not subject to the Medical Research Involving Human Subjects Act (WMO) and therefore do not require approval from a medical research ethics committee. We conducted this study using a pre-specified study protocol. We performed all methods in accordance with the relevant guidelines and regulations. Meta-data and data are property of IPCI. Researchers who are interested can contact the IPCI project team at www.ipci.nl. Our study protocol and statistical codes are available on request from the corresponding author. We used the STROBE and RECORD guidelines to report our findings.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data belong to IPCI and are only available through them. The code syntaxes from the current analyses are available from the corresponding author on reasonable request.
References
U.S. Department of Health and Human Services. Smoking Cessation. A Report of the Surgeon General. (U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Atlanta, GA, 2020).
GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1345–1422 (2017).
Jones, L. L. et al. Parental and household smoking and the increased risk of bronchitis, bronchiolitis and other lower respiratory infections in infancy: systematic review and meta-analysis. Respir. Res. 12, 5 (2011).
Jones, L. L., Hassanien, A., Cook, D. G., Britton, J. & Leonardi-Bee, J. Parental smoking and the risk of middle ear disease in children: a systematic review and meta-analysis. Arch. Pediatr. Adolesc. Med. 166, 18–27 (2012).
Silvestri, M., Franchi, S., Pistorio, A., Petecchia, L. & Rusconi, F. Smoke exposure, wheezing, and asthma development: a systematic review and meta-analysis in unselected birth cohorts. Pediatr. Pulmonol. 50, 353–362 (2015).
Vardavas, C. I. et al. The independent role of prenatal and postnatal exposure to active and passive smoking on the development of early wheeze in children. Eur. Respir. J. 48, 115–124 (2016).
Wang, Z. et al. Effects of secondhand smoke exposure on asthma morbidity and health care utilization in children: a systematic review and meta-analysis. Ann. Allergy Asthma Immunol. 115, 396–401 (2015).
Faber, T. et al. Effect of tobacco control policies on perinatal and child health: a systematic review and meta-analysis. Lancet Public Health 2, e420–e437 (2017).
World Health Organization. Tobacco Control to Improve Child Health and Development: Thematic Brief. https://www.who.int/publications/i/item/9789240022218 (2021).
Dove, M. S., Dockery, D. W. & Connolly, G. N. Smoke-free air laws and asthma prevalence, symptoms, and severity among nonsmoking youth. Pediatrics. 127, 102–109 (2011).
Been, J. V. et al. Smoke-free legislation and the incidence of paediatric respiratory infections and wheezing/asthma: interrupted time series analyses in the four UK nations. Sci. Rep. 5, 15246 (2015).
Been, J. V., Millett, C., Lee, J. T., van Schayck, C. P. & Sheikh, A. Smoke-free legislation and childhood hospitalisations for respiratory tract infections. Eur. Respir. J. 46, 697–706 (2015).
Mackay, D., Haw, S., Ayres, J. G., Fischbacher, C. & Pell, J. P. Smoke-free legislation and hospitalizations for childhood asthma. N. Engl. J. Med. 363, 1139–1145 (2010).
Millett, C., Lee, J. T., Laverty, A. A., Glantz, S. A. & Majeed, A. Hospital admissions for childhood asthma after smoke-free legislation in England. Pediatrics. 131, e495–501 (2013).
RIVM. Roken—Leeftijd en geslacht volwassenen. https://www.vzinfo.nl/roken/leeftijd-en-geslacht-volwassenen (2023).
World Health Organization. WHO report on the global tobacco epidemic 2019: offer help to quit tobacco use. https://www.who.int/publications/i/item/9789241516204 (2019).
Hoffman, S. J. & Tan, C. Overview of systematic reviews on the health-related effects of government tobacco control policies. Bmc Public Health 15, 744 (2015).
Faber, T., Been, J. V., Reiss, I. K., Mackenbach, J. P. & Sheikh, A. Smoke-free legislation and child health. NPJ. Prim. Care Respir. Med. 26, 16067 (2016).
Gonzalez, M. & Glantz, S. A. Failure of policy regarding smoke-free bars in the Netherlands. Eur. J. Public Health 23, 139–145 (2013).
Nebot, M. et al. Environmental tobacco smoke exposure in public places of European cities. Tob. Control 14, 60–63 (2005).
Wagner, J. et al. Environmental tobacco smoke leakage from smoking rooms. J. Occup. Environ. Hyg. 1, 110–118 (2004).
Nagelhout, G. E. et al. Prevalence and predictors of smoking in “smoke-free” bars. Findings from the International Tobacco Control (ITC) Europe Surveys. Soc. Sci. Med. 72, 1643–1651 (2011).
The International Tobacco Control Policy Evaluation Project. ITC Netherlands Survey—March 2011. https://itcproject.s3.amazonaws.com/uploads/documents/ITC_Netherlands_Survey_Report_on_Smokers_Awareness_of_the_Health_Risks_of_Smo.pdf (2011).
Been, J. V. et al. Impact of smoke-free legislation on perinatal and infant mortality: a national quasi-experimental study. Sci. Rep. 5, 13020 (2015).
Peelen, M. J. et al. Tobacco control policies and perinatal health: a national quasi-experimental study. Sci. Rep. 6, 23907 (2016).
Crone, M. R., Nagelhout, G. E., van den Burg, I. & HiraSing, R. A. [Passive smoking in young children in the Netherlands sharply decreased since 1996] Meeroken door kinderen in Nederland sinds 1996 sterk gedaald. Ned. Tijdschr. Geneeskd. 154, A1658 (2010).
Nagelhout, G. E., van den Burg, I., Crone, M. R., Zeegers, T. M. C. & Willemsen, M. C. Meeroken bij kinderen van 0 tot en met 18 jaar (2008–2011). (STIVORO, Den Haag, 2012).
Semple, M. G., Taylor-Robinson, D. C., Lane, S. & Smyth, R. L. Household tobacco smoke and admission weight predict severe bronchiolitis in infants independent of deprivation: prospective cohort study. Plos ONE 6, e22425 (2011).
Wilson, K. M., Pier, J. C., Wesgate, S. C., Cohen, J. M. & Blumkin, A. K. Secondhand tobacco smoke exposure and severity of influenza in hospitalized children. J. Pediatr. 162, 16–21 (2013).
DHD—Zorg voor data. https://www.dhd.nl/Paginas/home.aspx (2023).
te Brake, H., Verheij, R., Abrahamse, H. & de Bakker, D. Bekostiging van de huisartenzorg: vóór en na de stelselwijziging. Monitor 2006. https://www.nivel.nl/nl/publicatie/bekostiging-van-de-huisartsenzorg-voor-en-na-de-stelselwijziging-monitor-2006 (2007).
Been, J. V. et al. Smoke-free legislation and paediatric hospitalisations for acute respiratory tract infections: national quasi-experimental study with unexpected findings and important methodological implications. Tob. Control 27, e160–e166 (2018).
Been, J. V. & Sheikh, A. Investigating the link between smoke-free legislation and stillbirths. Expert Rev. Respir. Med. 10, 109–112 (2016).
Nederlandse overheid. Besluit rookverbod. http://wetten.overheid.nl/BWBR0023770 (2008).
Vlug, A. E. et al. Postmarketing surveillance based on electronic patient records: the IPCI project. Methods Inf. Med. 38, 339–344 (1999).
Thompson, M. et al. Duration of symptoms of respiratory tract infections in children: systematic review. Br. Med. J. 347, f7027 (2013).
Rosenfeld, R. M. & Kay, D. Natural history of untreated otitis media. Laryngoscope 113, 1645–1657 (2003).
Nederlands Huisartsen Genootschap. Registratie-adviezen (ICPC) bij NHG-Standaarden. https://www.nhg.org/themas/artikelen/icpc (2020).
WHO Collaborating Centre for Drug Statistics Methodology. ATC—Structure and Principles. https://www.whocc.no/atc/structure_and_principles/ (2020).
The International Tobacco Control Policy Evaluation Project. ITC Netherlands National Report—June 2010. https://itcproject.s3.amazonaws.com/uploads/documents/ITC_Netherlands_National_Report_Waves_1_to_3_2008-2009_J.pdf (2010).
Acknowledgements
We thank Prof. dr. Johan van der Lei, Dr. Katia Verhamme, and Dr. Marjolein Engelkes for sharing their expertise on the IPCI database. We thank Marcel de Wilde and Mees Mosseveld for their help in extracting the data from the electronic medical records. We also thank Desiree de Jong and Tineke de Ben for their support in getting access to the IPCI computers. Funding: Netherlands Lung Foundation 4.2.14.063JO.
Author information
Authors and Affiliations
Contributions
J.V.B. conceptualised the study, developed the methods, and supervised the entire process. T.F. wrote the study protocol, conducted the data extraction, cleaning, and analysis, and wrote the drafts. L.C. provided expert statistical support. All co-authors contributed to developing the methods, interpreted the findings, and reviewed and commented on the drafts. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Faber, T., Coffeng, L.E., Sheikh, A. et al. Tobacco control policies and respiratory conditions among children presenting in primary care. npj Prim. Care Respir. Med. 34, 11 (2024). https://doi.org/10.1038/s41533-024-00369-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-024-00369-8