Abstract
Information about the decline rate in forced expiratory volume in 1 s (FEV1s) in older adults with COPD is scarce. A total of 4082 community-dwelling older adults from the population-based study Good Aging in Skåne were followed for 12 years and 143 participants developed COPD. The average FEV1s decline is estimated to be 66.3 mL/year, (95% CI [56.4; 76.3]) and 43.3 mL/year (1.7%/year, 95% CI [41.2; 45.5]) for COPD and non-COPD participants, respectively.
Similar content being viewed by others
The forced expiratory volume in 1 s (FEV1s) decline rate in people aged ≥ 65 years ranges from 17.7 to 46.4 mL/year1. The decline rate in FEV1s due to chronic obstructive pulmonary disease (COPD) is accelerated compared to natural decline. In adults aged 48–64 years, conflicting results for the FEV1s annual decline rate in mild to moderate COPD patients have been reported (33–129 mL/year2,3,4,5,6). Studies regarding the lung function decline in early-stage COPD patients diagnosed above 65 years of age are scarce1,7. We aim to estimate the FEV1s annual decline rate in community-dwelling older adults diagnosed with early-stage COPD and to investigate whether it differs from that due to normal aging.
Baseline characteristics are shown in Table 1. One-hundred and forty-three of the 4082 included participants were diagnosed with COPD in standard clinical practice after the baseline visit. The COPD prevalence at the first visit was 5.5% (95% CI [5.0–6.1]). The incidence rate of COPD was 10.6 cases per 1000 person/years (95% CI [9.0; 12.4]).
The average FEV1s decline rate is estimated to be 66.3 mL/year (2.8%/year, 95% CI [56.4; 76.3], p-value < 0.001) and 43.3 mL/year (1.7%/year, 95% CI [41.2; 45.5], p-value < 0.001) for the COPD and non-COPD participants, respectively. Participants diagnosed with COPD have an additional decline of 22.3 mL/year (1.0%/year, 95% CI [12.8; 33.3], p-value < 0.001) compared to non-COPD peers (Supplementary Tables 2, 3, and 4). The estimates are consistent with those obtained in the sensitivity analyses (see Supplementary Table 5). No difference was observed in the mean FEV1s for participants diagnosed before/after 70 years of age (57.2 and 50.0 mL/year, respectively).
The estimated prevalence and incidence of COPD are concordant with previously reported values8,9. As also seen in younger COPD patients2,4,5,10, a large variability in FEV1s was observed. The estimated mean annual FEV1s decline in COPD (66.3 mL/year, 2.8%/year) is in the upper range of previously reported values for younger COPD patients (33–129 ml/year2,3,4,5,6) and larger than the decline rates for older adults reported previously11 (49.1 mL/year and 38.3 mL/year for males and females, respectively). The observed average difference in mean annual decline rate between early-stage COPD and non-COPD participants is −23.0 mL/year. In other words, the contribution of early-stage COPD to the FEV1s decline in older adults is about—1.0%/year.
Lung function is inversely associated with heart and cerebrovascular diseases, neurological deficits, diabetes, and metabolic syndrome. On average, 50% of adults aged ≥ 70 years have at least three chronic diseases12. Thus, the observed decline rate in FEV1s is explained by a combination of loss of lung function due to aging (e.g., worsening of lung elasticity, weakened muscles, decrease surface area for alveolar gas exchange) and co-existing comorbidities.
The interpretation of our results is affected by the study design and the difficulties of establishing an accurate COPD diagnosis in older adults. Healthy participants are over-represented in the study. Patients were diagnosed according to standard clinical routines and there is risk of COPD misclassification13. Interestingly, participants who developed COPD during follow-up, had on average a lower FEV 1s at the first study visit, which could be an indication of underdiagnosis of heart disease, COPD, and/or asthma. Some diagnosed COPD participants had study spirometries within the normal range. Given the large variability observed in spirometries and the fact that most of COPD diagnosed participants are at an early stage of the disease, it is not possible to distinguish misclassified COPD cases from correct diagnosed COPD participants who had a normal spirometry during the study visit. Subjects with comorbidity and inconclusive spirometry results may not have been properly diagnosed in clinical practice. The consequence of this possible misclassification would most likely result in an underestimation of true decline in early onset COPD. Nevertheless, our estimates seem to be robust towards a potential COPD misclassification since concordant results were obtained in a sensitivity analysis where the diagnosis was based solely on study spirometry. We also acknowledge the existence of several COPD phenotypes which might express different trajectories. It was beyond our reach to estimate different decline rates for different COPD phenotypes.
In summary, this study indicates that the FEV1s annual decline rate in early-stage COPD older adults is slightly higher than the decline rate observed in peers without COPD.
Methods
Study population
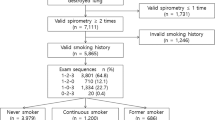
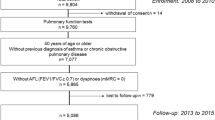
As shown in Fig. 1, data were retrieved from the on-going population-based study Good Aging in Skåne (GÅS)14. Briefly, 60- to 93-year-old subjects living in Skåne, Sweden, are randomly invited using the population register. Participants are offered a thorough physical, medical, and psychological examination and are invited to follow-up examinations at regular intervals until death. To encourage participation of frail adults, the study team performs home visits following the same study protocol. Three waves have been fully recruited with an initial participation rate of approximately 60%. Participants recruited during the first wave in 2001–2004 were 60, 66, 72, 78, 81, 84, 87, 90, or 93 years old. Participants recruited during the second wave in 2006–2013 were 60, 66, or 81 years old. Participants recruited during third wave in 2012–2016 were 60 or 81 years old. A fourth wave is being recruited since 2019 including participants who are 60 or 81 years old. The GÅS study is conducted according to the Declaration of Helsinki and Good Clinical Practice guidelines and is approved by the Lund University Ethics Review Board (LU 744–00). All participants provide written informed consent. In this study, we aim to study early onset progression, and thus to minimize bias participants with a COPD diagnosis at baseline were excluded from the analysis.
Spirometry assessments
Spirometry assessments were performed using a Vitalograph 2120 spirometer (Vitalograph Ltd, Buckingham, UK) according to the American Thoracic Society guidelines15. Bronchodilators were not administrated during the first wave baseline visit. Subjects received 1.0 mg of β2-receptor agonist terbutaline 10 min prior to the spirometry at all other visits.
Identification of comorbidities and definition of COPD
Comorbidities were identified during the medical examination, and by retrieving medical records and diagnosis codes from the Skåne Healthcare Registry16 (see Supplementary Table 1). Information about prescribed medicines was obtained from medical records and self-reported. The COPD diagnosis was retrieved from medical records. Clinically, diagnosis of COPD in the region of Skåne is based on three criteria: spirometry verified obstructivity (FEV1/FVC < 0.7 after bronchodilation), current airway symptoms, and a history of a risk factor for COPD. COPD diagnosis also included emphysema and chronic bronchitis.
COPD was graded according to the Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease (GOLD) classification17 using the spirometries collected during the study visits. In some cases, participants diagnosed with COPD had a normal spirometry during the study visit. Therefore, an additional category level (category 0) was included to accommodate diagnosed subjects whose FEV1s/FVC ratio was ≥ 0.75. The spirometry performed at the study visit was used for the COPD GOLD classification. The reference equations for lower limit of normal are only available for subjects younger than 95 years old and for this calculation, age was truncated at 95 years.
Statistical analysis
The aim of the statistical analysis was to estimate the average annual decline rate in FEV1s in COPD patients at early COPD onset and to compare it to the decline rate in participants without COPD. The annual change in FEV1s was defined as the difference in FEV1s between two consecutive study visits, divided by the time passed between the visits. This model assumes that the annual decline rate is constant over time. A mixed model for repeated measures with random intercept (participants) was implemented. The variables FEV1s, age, sex, smoking status, education, body mass index, heart disease, cerebrovascular disease, asthma, and diabetes (at baseline) were included to mitigate confounding.
Estimating the difference in annual decline rate between participants with and without a COPD diagnosis is challenging since the two groups should only differ in their COPD status. Patients in clinical practice do not perform spirometry examinations in a regular way. Therefore, it could be more likely for a participant with a low FEV1s to get a spirometry examination and thus a COPD diagnosis compared to a participant with higher FEV1s values regardless of their true COPD status. The previous value of FEV1s may affect the likelihood of getting a COPD diagnosis and thus time-varying confounding may be present. In order to minimize bias, sensitivity analyses using a marginal structural mixed model were performed (see Supplementary Table 5). The risk for misclassification in the COPD diagnosis is acknowledged. We, therefore, presented a Supplementary Note about sensitivity analyses where the COPD status was assigned using the spirometry results obtained at the study visits. The statistical software Stata IC 14.2 (StataCorp LLC, Texas, USA) was used.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Data are accessible on request (https://neardb.near-aging.se/study/gas-snac-s).
References
Thomas, E. T., Guppy, M., Straus, S. E., Bell, K. J. L. & Glasziou, P. Rate of normal lung function decline in ageing adults: A systematic review of prospective cohort studies. BMJ Open 9, e028150 (2019).
Bridevaux, P. O. et al. Long-term decline in lung function, utilisation of care and quality of life in modified GOLD stage 1 COPD. Thorax 63, 768–774 (2008).
Leem, A. Y. et al. Longitudinal decline in lung function: A community-based cohort study in Korea. Sci. Rep. 9, 13614 (2019).
Vestbo, J. et al. Changes in forced expiratory volume in 1 second over time in COPD. N. Engl. J. Med. 365, 1184–1192 (2011).
Bhatt, S. P. et al. Association between functional small airway disease and FEV1 decline in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 194, 178–184 (2016).
Chen, S. et al. Risk factors for FEV(1) decline in mild COPD and high-risk populations. Int. J. Chron. Obstruct Pulmon Dis. 12, 435–442 (2017).
Tantucci, C. & Modina, D. Lung function decline in COPD. Int. J. Chron. Obstruct Pulmon Dis. 7, 95–99 (2012).
Atsou, K., Chouaid, C. & Hejblum, G. Variability of the chronic obstructive pulmonary disease key epidemiological data in Europe: Systematic review. BMC Med. 9, 7 (2011).
Terzikhan, N. et al. Prevalence and incidence of COPD in smokers and non-smokers: The Rotterdam Study. Eur. J. Epidemiol. 31, 785–792 (2016).
Whittaker, H. R. et al. Accelerated FEV1 decline and risk of cardiovascular disease and mortality in a primary care population of COPD patients. Eur. Respir. J. https://doi.org/10.1183/13993003.00918-2020 (2021).
Luoto, J., Pihlsgard, M., Wollmer, P. & Elmstahl, S. Relative and absolute lung function change in a general population aged 60–102 years. Eur. Respir. J. https://doi.org/10.1183/13993003.01812-2017 (2019).
Divo, M. J., Martinez, C. H. & Mannino, D. M. Ageing and the epidemiology of multimorbidity. Eur. Respiratory J. 44, 1055–1068 (2014).
Josephs, L., Culliford, D., Johnson, M. & Thomas, M. COPD overdiagnosis in primary care: A UK observational study of consistency of airflow obstruction. npj Prim. Care Respiratory Med. 29, 33 (2019).
Ekström, H. & Elmståhl, S. Pain and fractures are independently related to lower walking speed and grip strength: Results from the population study “Good Ageing in Skåne”. Acta Orthop. 77, 902–911 (2006).
Standardization of Spirometry, 1994 Update. American Thoracic Society. Am. J. Respir. Crit. Care Med. 152, 1107–1136 (1995).
Löfvendahl, S., Schelin, M. E. C. & Jöud, A. The value of the Skåne Health-care Register: Prospectively collected individual-level data for population-based studies. Scand. J. Public Health 48, 56–63 (2019).
Vogelmeier, C. F. et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 Report: GOLD executive summary. Eur. Respiratory J. 49, 1700214 (2017).
Acknowledgements
This study was supported by the Swedish Research Council (grant No 2017-01613), the Medical Faculty at Lund University, and the Skåne county. The funders had no role in the study.
Funding
Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
A.R.: conceptualization, data curation, formal analysis, writing – original draft, writing – review and editing, and supervision; K.E.: conceptualization, writing – review and editing; S.E.: conceptualization, funding acquisition, writing – review and editing, and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rosso, A., Egervall, K. & Elmståhl, S. Annual decline rate in FEV1s in community-dwelling older adults diagnosed with mild to moderate COPD. npj Prim. Care Respir. Med. 32, 30 (2022). https://doi.org/10.1038/s41533-022-00292-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-022-00292-w
This article is cited by
-
Association of systemic anticholinergic medication use and accelerated decrease in lung function in older adults
Scientific Reports (2024)
-
Cognitive decline and risk of dementia in older adults after diagnosis of chronic obstructive pulmonary disease
npj Primary Care Respiratory Medicine (2023)