Abstract
Incidental Lewy body disease (ILBD) is a neuropathological diagnosis of brains with Lewy bodies without clinical neuropsychiatric symptoms. Dopaminergic deficits suggest a relationship to preclinical Parkinson’s disease (PD). We now report a subregional pattern of striatal dopamine loss in ILBD cases, with dopamine found significantly decreased in the putamen (−52%) and only to a lower extent in the caudate (−38%, not statistically significant); this is similar to the pattern in idiopathic PD in various neurochemical and in vivo imaging studies. We aimed to find out if our recently reported impaired storage of dopamine in striatal synaptic vesicles prepared from striatal tissue of cases with idiopathic PD might be an early or even causative event. We undertook parallel measurements of [3H]dopamine uptake and vesicular monoamine transporter (VMAT)2 binding sites by the specific label [3H]dihydrotetrabenazine on vesicular preparation from caudate and putamen in ILBD. Neither specific uptake of dopamine and binding of [3H]dihydrotetrabenazine, nor mean values of the calculated ratios of dopamine uptake and VMAT2 binding, a measure of uptake rate per transport site, were significantly different between ILBD and controls. ATP-dependence of [3H]dopamine uptake revealed significantly higher rates in putamen than in caudate at saturating concentrations of ATP in controls, a subregional difference lost in ILBD. Our findings support a loss of the normally higher VMAT2 activity in putamen as a contributing factor to the higher susceptibility of the putamen to dopamine depletion in idiopathic PD. Moreover, we suggest ILBD postmortem tissue as a valuable source for testing hypotheses on processes in idiopathic PD.
Similar content being viewed by others
Introduction
Individuals with Lewy bodies or Lewy neurites at autopsy but without clinical findings of parkinsonism or dementia during their lifetime can be subsumed under cases with incidental Lewy body disease (ILBD). They are considered pre-symptomatic Parkinson’s disease (PD) by their nigrostriatal pathological features that are intermediate between those in morphologically normal control persons and those with overt PD1,2. However, there is a range of neurological syndromes with striatal loss of dopamine that are distinct from idiopathic PD, such as multiple system atrophy and progressive supranuclear palsy3,4,5,6, summarized as atypical PD. In neurochemical studies on postmortem brains of patients with idiopathic PD, a characteristic pattern of dopamine loss has been found in the striatum with a nearly complete depletion of dopamine in all subdivisions of the putamen and substantial levels of dopamine remaining in the caudate7. With the progress of in vivo imaging methods, this pattern has also been detected in live patients with various stages of idiopathic PD8,9,10,11,12 and allowed differentiation between idiopathic PD and atypical PD13,14,15,16,17. Although the incidence of idiopathic PD increases with age, and there is an age-dependent reduction in striatal dopamine innervation18, the regional pattern of striatal dopamine loss in normal aging differs substantially from the pattern typically observed in idiopathic PD19. By contrast, 18F-dopa uptake for asymptomatic co-twins of patients with PD already revealed the typical pattern with a small but significant reduction of the dopamine marker in putamen but not in caudate20.
In ILBD, two neurochemical markers of striatal dopamine nerve terminals have been reported to be reduced, the immunoreactivity of tyrosine hydroxylase1,2,21 and the vesicular monoamine transporter 21. However, all striatal findings are based on analysis of the putamen, and there are neither data on the caudate in ILBD in the literature nor on striatal dopamine tissue levels. We therefore set out for analysis of monoamine neurotransmitter tissue levels in both caudate and putamen of cases with ILBD. In a recent study on postmortem striatal tissue of cases with idiopathic PD, we observed a loss of 56% and 90% dopamine transport efficiency in synaptic vesicles of dopamine nerve terminals in the caudate and in the putamen, respectively22. Therefore, we also performed vesicular uptake on the caudate and putamen of our cases in this presumptive preclinical phase of PD.
Results
Monoamine neurotransmitters
Monoamine neurotransmitter levels in striatal tissue of control cases (Fig. 1a–f) displayed the typical concentration range with mean values of serotonin about five times and of dopamine about 150 times higher than that of noradrenaline23,24,25. Whereas noradrenaline and serotonin were either unchanged or insignificantly increased in ILBD (Fig. 1a–d), two-way analysis of variance for the factors disease (ILBD or control) and region (caudate or putamen) revealed a significant decrease of dopamine in the putamen (−52%, t = 3.044, p = 0.007; Fig. 1f), but not in the caudate (−38%) in ILBD (Fig. 1e).
Tissue levels of noradrenaline (a, b), serotonin (c, d), dopamine (e, f), and its metabolites 3,4-dihydroxyphenylacetic acid (g, h) and homovanillic acid (i, j) in caudate (left panels) and putamen (right panels) of control and ILBD subjects. Data are given as single values, means and the error bar s.e.m. in µg/g wet weight. *p < 0.05 vs. control by two-way analysis of variance for the factors disease (ILBD or control) and region (caudate or putamen).
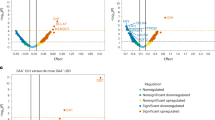
Dopamine uptake by synaptic vesicles prepared from striatal tissue of control (left panels) and ILBD subjects (right panels). Total uptake (closed symbols) and uptake in the presence of reserpine (open symbols) in the putamen (a, b) and in the caudate (c, d) and comparison of total uptake in control (e) and ILBD subjects (f) of the putamen (closed symbols) vs. caudate (open symbols). Synaptic vesicle preparations were incubated with 0.1 µM [3H]dopamine and MgATP at the concentrations indicated at 30 °C for 5 min in the absence or presence of 1 µM reserpine. Data are given as means ± s.e.m. (controls, n = 6; ILBD, n = 4) and additionally single values in (e, f). *p < 0.05 vs. caudate by two-way repeated measures ANOVA for the factors region (caudate or putamen) and ATP (0, 0.1, 0.4, or 2 mM).
Dopamine metabolites
The dopamine metabolites DOPAC and HVA have not been found to change significantly in ILBD, with mean values of ILBD 0.1% and 16% below controls, respectively, in caudate (Fig. 1g, i) and 51% and 26% below controls, respectively, in the putamen (Fig. 1h, j). Molar ratios of HVA/dopamine were quite similar in the caudate and putamen of control cases (caudate, 0.77 ± 0.11; putamen, 0.89 ± 0.20), whereas the respective mean value was strongly but insignificantly increased in the putamen of ILBD with high variation between single cases (caudate, 1.13 ± 0.19; putamen, 4.69 ± 3.28).
Dopamine uptake and DTBZ binding in striatal synaptic vesicles
In order to determine transport efficiency in striatal synaptic vesicles, we isolated vesicular preparations of caudate or putamen tissue following our recent protocol22 and performed parallel dopamine uptake experiments and binding experiments with [3H]DTBZ, a label selective for the vesicular monoamine transporter 2 (VMAT2). The calculated ratio of dopamine uptake to [3H]DTBZ binding reflects the number of transported dopamine molecules per unit time per VMAT2 transport site, a measure of turnover or transport efficiency. There was no significant difference between the putaminal or caudate tissue of controls and ILBD cases neither in dopamine uptake and [3H]DTBZ binding nor in turnover (Table 1).
ATP-dependence of vesicular dopamine transport
There was a considerable variation between single cases of control and ILBD samples, as is often the case in biological assays on postmortem tissue. Therefore, we went for parallel measurements of ATP-dependency of dopamine uptake in the putamen and caudate tissue for each control and each ILBD case at 0, 0.1, 0.4, and 2 mM ATP using a shortened preparation of synaptic vesicles without ATP preincubation. In the absence of ATP, there was no reserpine-sensitive dopamine uptake, whereas uptake was clearly reserpine sensitive at 0.1 mM and higher ATP concentrations, and the uptake stimulatory effect of ATP appeared saturated at a concentration of 2 mM (Fig. 2a–d). A two-way repeated measures ANOVA for the factors region and ATP revealed significantly higher rates of vesicular dopamine uptake in putamen than in caudate at saturating concentrations of ATP in controls (0.4 mM ATP, t = 2.216, p = 0.046; 2 mM ATP, t = 4.561, p < 0.001; Fig. 2e), but not in ILBD where this subregional difference was lost (Fig. 2f).
Discussion
Idiopathic PD is a neurodegenerative disorder where progression spans a period of years and has presumably an asymptomatic preclinical phase before. The assumption of an asymptomatic preclinical phase is already based on early postmortem studies which, quite early after the fundamental discovery of the dopamine loss in PD26, suggest that striatal dopamine changes remain clinically silent until the threshold value of 60–80% dopamine loss is reached27,28. Regression analysis of the decline of pigmented neurons in the substantia nigra in relation to the duration of symptoms results in an estimation of 30% total loss at the time of PD symptom onset29,30. Measurements of the rate of PD progression by assessing striatal [18F]dopa metabolism with PET and UPDRS scoring on two occasions in individual PD patients suggested an average preclinical period between 3 and 7 years31. Since Lewy bodies, besides the death of dopaminergic neurons in the substantia nigra, are considered the hallmark of PD, cases with ILBD might be within this preclinical period given their substantia nigra neuron density being intermediate between control and PD2,32,33. Our findings of striatal dopamine being significantly reduced in putamen but not in caudate of ILBD cases support the evidence that ILBD might be, in fact, the preclinical status of not only parkinsonism in general but idiopathic PD in particular, given the special susceptibility of putamen to loss of dopamine markers in idiopathic PD7,8,9,10,11,12. Given that a recent postmortem study has found pathological α-synuclein in the enteric nervous system rarely without concomitant deposits in the central nervous system in ILBD34, the topographically limited changes in our ILBD cases indicate the vulnerability of dopaminergic terminals as key elements in idiopathic PD supporting a top-down pathological process35. The about 50% reduction of dopamine in putamen seems to be compensated in a way that clinical parkinsonism was absent in ILBD. Dopamine turnover, as determined by the ratio of HVA/dopamine, was increased in the putamen; however, it did not reach significance due to high variation with very high ratios in the two cases of ILBD with the lowest dopamine levels in the putamen. Loss of dopamine due to loss of dopaminergic nerve endings below 50% might be compensated without augmented dopamine synthesis in remaining neurons by concomitant loss of dopamine transporters potentiating volume transmission following the concept of “passive stabilization”36.
Other subregional characteristics in idiopathic PD striatum are a higher loss of dopaminergic innervation in the posterior than anterior putamen and asymmetry of dopaminergic innervation between hemispheres. Corresponding dopamine tissue levels and vesicular transport in ILBD would be highly interesting. However, routine dissection protocols are performed in a way that does not allow such analysis.
In a recent study on vesicular preparations from postmortem striatal tissue of cases with idiopathic PD, we reported a significantly reduced efficiency of vesicular dopamine transport, in particular in the putamen with an uptake rate per transport site reduced by 90% in dopamine nerve terminals. Similarly to this study, transport efficiency was determined by estimating both dopamine transport initial rate and steady-state binding of the specific label [3H]DTBZ to the VMAT2 sites in the preparation of synaptic vesicles of each control and idiopathic PD case and calculating the individual uptake rate per transport site. The observed dopamine transport defect appeared to be a specific feature of PD since it was found absent in tissue from cynomolgus monkeys with a comparable degree of degeneration of nigrostriatal dopaminergic terminals produced by MPTP22.
This defect of vesicular transport in PD can be taken as indicating increased cytosolic dopamine levels in PD striatum in vivo, which in turn would lower the threshold for several pathways of striatal dopaminergic neurodegeneration due to the production of dopamine-derived, cytotoxic reactive species triggering the “toxic-dopamine-cascade”37,38,39. On the other hand, the potential damage of high cytosolic dopamine in substantia nigra compacta compared to reticulata and ventrotegmental area is rescued by the synthesis of neuromelanin40,41. One could reason that similar findings in preclinical cases such as ILBD might indicate them as causative events in the PD disease process. However, in this study, dopamine uptake rates, [3H]DTBZ binding density, and turnover in vesicular preparations from caudate and putamen were not different in ILBD cases from controls, controls which nonetheless were in the same range of controls as in our previous study on PD. The number of control and ILBD cases studied was low; however, there was not even a tendency for reduction of mean values of uptake, binding sites, or turnover in ILBD as compared to control (Table 1), which does not suggest a different outcome with a higher sample size. As the vesicular transport dysfunction in our previous study was from patients with more than eight years of disease duration22, the vesicular transport dysfunction could have been due to secondary change by some more fundamental disturbance.
Since active transport into storage vesicles is driven by a transmembrane pH and electrochemical gradient generated by the vesicular H+-ATPase42, also called V-ATPase43, we reasoned that ATP-dependence of dopamine uptake might give additional insight and performed assays of putaminal and caudate preparations of synaptic vesicles of individual cases in parallel. The concentrations of ATP to stimulate dopamine uptake with saturation at 2 mM were in agreement with a study where ATP-dependence of another ATPase was reported, specifically ATPase activity in vascular membranes44. There was no difference in potency or maximal velocity of uptake between controls and ILBD; however, total dopamine uptake was significantly higher in putamen than in caudate at saturating concentrations of ATP in controls, a difference lost in ILBD. The higher vesicular dopamine uptake in putamen than caudate in head-to-head experiments might explain the higher dopamine tissue level in putamen than caudate in controls (p < 0.015 by paired Student’s t-test) since dopamine tissue levels essentially stem from dopamine within synaptic vesicles where dopamine depends on continuous accumulation by the vesicular monoamine transporter. The loss of the higher activity of the vesicular monoamine transporter in putamen than in caudate in ILBD might be an early event in the development of neurodegeneration in idiopathic PD. Since transport was determined by an accumulation assay, differences in energy-dependent storage might, in principle, contribute to the measured pmol/mgprot/min, although the short incubation time of 5 min, aiming at initial rates, makes this contribution less likely. Storage may, however, be a factor in dopamine tissue levels. Findings on reduced NADH-ubiquinone reductase and NADH cytochrome c reductase activities in the substantia nigra45 and down-regulated genes of subunits of the respiratory chain complex I in nigral dopamine neurons46,47 suggest disrupted energy metabolism in dopamine neurons in PD which might have a higher impact on dopamine in putamen with its higher levels and therefore higher energy-dependence. However, another very recent laser capture microdissection study on neuromelanin-positive cells revealed an upregulation of oxidative phosphorylation pathways in ILBD48, suggesting that reduced vesicular uptake and storage in putamen might be more related to changes in vesicular monoamine transporter 2 or vesicular H+-ATPase.
In conclusion, although our findings cannot rule out that ILBD is only an associated factor of PD, they give new support to the assumption that ILBD might be a preclinical stage of idiopathic PD. Obviously, this stage is only available for examinations postmortem since it is based on a neuropathological analysis. However, quite a few novel hypotheses about the neurodegenerative process in PD have been tested in postmortem tissue from PD patients, such as the increased expression of the vesicular glutamate transporter49, activation of NADPH oxidase 250, or LRRK2 kinase51 in tyrosine hydroxylase positive neurons. ILBD postmortem tissue could be a valuable source for testing these hypotheses in idiopathic PD at an early stage with more validity for a causal role in the progression of the disease.
Methods
Human brain tissue
Tissue for this study was provided by the Newcastle Brain Tissue Resource, with full informed consent of donors. Brain tissue was obtained at autopsy and stored within the Newcastle Brain Tissue Resource (NBTR), with the full written informed consent of the donors, in accordance with the Newcastle University Ethics Board (The Joint Ethics Committee of Newcastle and North Tyneside Health Authority, reference: 08/H0906/136). Samples from the midcaudate (head) and midputamen (Supplementary Fig. 1) from six control subjects (52–88 years; two females, four males) and five ILBD subjects (70–96 years; three females, two males) without evidence in their records of any neurological or psychiatric disorder were stored at −80 °C until analysis. The standardized neuropathological assessment was performed for all cases and included the National Institute on Aging-Alzheimer’s Association (NIA-AA) criteria52 (inclusive of Thal phases of Aβ deposition, Braak staging of neurofibrillary tangle (NFT) pathology and Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) scoring of the density of neuritic plaques) and McKeith Lewy body stage53, LBD-related neuropathological findings of the subjects, diagnosed according to the Lewy Pathology Consensus Criteria54 are shown in Table 2. The mean age (±SEM) of the control and ILBD group (75 ± 6 years, range 52–88 years and 82 ± 5, range 70–96 years, respectively) did not differ significantly, nor did the postmortem delay (=death to autopsy interval; controls: 51 ± 15 h, range: 25–102 h; ILBD: 54 ± 15 h range: 16–98 h).
Determination of monoamine neurotransmitters and dopamine metabolites
Distinct samples of 20–50 mg from caudate and putamen frozen and kept at −80 °C were ultrasonicated from all subjects with an ultrasonic probe sonicator in 25 volumes of ice-cold perchloric acid, sodium bisulfite, and 3,4-dihydroxybenzylamine as internal standard (final concentration 0.1 M, 0.4 mM, and 25 µg/l, respectively). For determination of noradrenaline and dopamine, homogenates were centrifuged at 16,100 × g for 10 min at 4 °C, and 50 µl of supernatant was extracted with alumina oxide (10 g/l) in 1 M Tris-HCl, pH 8.6, and after washing with H2O and desorption with 0.2 ml 0.1 M perchloric acid containing 0.4 mM sodium bisulfite; 100 µl was injected into a high-performance liquid chromatography system with electrochemical detection (HPLC/ED) with a sodium phosphate mobile phase with l-octane sulfonic acid as described previously25,55. For determination of serotonin, 3,4-dihydroxyphenylacetic acid, and homovanillic acid, the supernatant was diluted 1:4 with 0.1 M perchloric acid containing 0.4 mM sodium bisulfite, and 100 µl was injected directly into an HPLC/ED system with a sodium phosphate mobile phase with l-heptane sulfonic acid as described previously25,55.
Preparation of synaptic vesicles
For performing vesicular uptake and [3HDTBZ]-binding from the same preparation, about 140–180 mg of striatal tissue were homogenized in 8 volumes of ice-cold 0.3 M sucrose containing 25 mM Tris (pH 7.4) and 10 µM pargyline, using seven up-down strokes in a glass Teflon Potter-type homogenizer and the whole further procedure was performed at 4 °C. The sucrose-homogenate was centrifuged at 1000 × g for 15 min, and the supernatant was recentrifuged at 20,000 × g for 30 min. The resulting pellet (“P2”) was subjected to osmotic shock by resuspension in 1 ml H2O, frozen for about 15 min, and, after thawing, homogenized in a total of 2 ml H2O. The aqueous samples were centrifuged at 22,000 × g for 15 min, and the osmolarity of the supernatant was readjusted by the addition of 1.3 M potassium phosphate buffer (pH 7.4) in 1/10 the volume. The supernatant of the 20,000 × g centrifugation (see above) was centrifuged at 100,000 × g for 30 min, and the resulting pellet was resuspended in the about 2.17 ml of the 22,000 × g supernatant readjusted to 0.13 M potassium phosphate, thus combining vesicles in the supernatant of the P2 pellet and in the hypoosmotically shocked P2 pellet. After incubation in a total volume of 3 ml assay buffer KP (0.13 M potassium phosphate, pH 7.4) in the presence of 2 mM MgATP in a 30 °C water bath for 4 min and centrifugation at 4 °C at 100,000 × g for 45 min the resulting pellet was resuspended in 4.8 ml KP. On each preparation, 1.5 ml were centrifuged at 4 °C at 153,000 × g for 45 min, and the pellet was resuspended in 100 µl of binding buffer SP (25 mM sodium phosphate, pH 7.7) and frozen at −80 °C until the [3H]DTBZ binding experiment and the rest of the preparation was used for vesicular uptake. Protein content was determined according to the Bradford method by a Bio-Rad assay kit.
For comparison of ATP-dependence of vesicular uptake in putamen vs. caudate, about 200–350 mg striatal tissues were homogenized, volumina were up-scaled accordingly, and the preparation was simplified in a way that the combined vesicles in the supernatant of the P2 pellet and in the hypoosmotically shocked P2 pellet were directly used for uptake experiments.
Vesicular uptake
Uptake was performed in a total volume of 1.5 ml KP containing 0.1 µM [3H]dopamine (New England Nuclear GmbH, Vienna), various concentrations of MgATP (2 mM in the uptake experiments with parallel [3HDTBZ]-binding experiments) and 1 µM reserpine for determination of unspecific uptake as described previously22. Transport was initiated by placing the tubes in a 30 °C water bath and adding 0.5 ml vesicle suspension (obtained from about 15–20 mg striatal tissue) for 5 min. Uptake was terminated by the addition of 2.5 ml ice-cold KP and immediate filtration under vacuum onto Whatman GF/B filter paper pre-soaked in 1% polyethylenimine using a Brandel harvester. The filters were washed twice with an additional 3 ml of cold KP and, after shaking in a liquid scintillation cocktail at 55 °C for 1 h, analyzed for tritium radioactivity in a liquid scintillation counter.
[3H]DTBZ binding
Binding of (±)-a-dihydrotetrabenazine [2-3H] (American Radiolabeled Chemicals, Inc., Hartmann Analytic GmbH, Braunschweig, Germany) was performed on 25 µl thawed preparation in SP at a total volume of 25 µl for 90 min at 30 °C as described previously22.
Data and statistical analysis
Data are reported as mean ± SE. Statistical analysis was done for neurotransmitter tissue levels using two-way analysis of variance for the factors disease (ILBD or control) and region (caudate or putamen) and for comparison of uptake in the putamen and caudate in the various control and ILBD cases using two-way repeated measures ANOVA (two factor repetition) for the factors region (caudate or putamen) and ATP (0, 0.1, 0.4, or 2 mM), both tests followed by pairwise multiple comparison procedures (Holm–Sidak method) after data passed the normality test (Shapiro–Wilk) and the equal variance test (Brown–Forsythe).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data that support the findings of this study are available from the corresponding author.
References
DelleDonne, A. et al. Incidental Lewy body disease and preclinical Parkinson disease. Arch. Neurol. 65, 1074–1080 (2008).
Dickson, D. W. et al. Evidence that incidental Lewy body disease is pre-symptomatic Parkinson’s disease. Acta Neuropathol. 115, 437–444 (2008).
Spokes, E. G., Bannister, R. & Oppenheimer, D. R. Multiple system atrophy with autonomic failure: clinical, histological and neurochemical observations on four cases. J. Neurol. Sci. 43, 59–82 (1979).
Kish, S. J., Chang, L. J., Mirchandani, L., Shannak, K. & Hornykiewicz, O. Progressive supranuclear palsy: relationship between extrapyramidal disturbances, dementia, and brain neurotransmitter markers. Ann. Neurol. 18, 530–536 (1985).
Tong, J. et al. Brain dopamine-stimulated adenylyl cyclase activity in Parkinson’s disease, multiple system atrophy, and progressive supranuclear palsy. Ann. Neurol. 55, 125–129 (2004).
Tong, J. et al. Brain alpha-synuclein accumulation in multiple system atrophy, Parkinson’s disease and progressive supranuclear palsy: a comparative investigation. Brain 133, 172–188 (2010).
Kish, S. J., Shannak, K. & Hornykiewicz, O. Uneven pattern of dopamine loss in the striatum of patients with idiopathic Parkinson’s disease. Pathophysiologic and clinical implications. N. Engl. J. Med. 318, 876–880 (1988).
Nahmias, C., Garnett, E. S., Firnau, G. & Lang, A. Striatal dopamine distribution in Parkinsonian patients during life. J. Neurol. Sci. 69, 223–230 (1985).
Tedroff, J. et al. Striatal kinetics of [11C]-(+)-nomifensine and 6-[18F]fluoro-L-dopa in Parkinson’s disease measured with positron emission tomography. Acta Neurol. Scand. 81, 24–30 (1990).
Turjanski, N. et al. Comparison of striatal 18F-dopa uptake in adult-onset dystonia-parkinsonism, Parkinson’s disease, and dopa-responsive dystonia. Neurology 43, 1563–1568 (1993).
Sawle, G. V., Playford, E. D., Burn, D. J., Cunningham, V. J. & Brooks, D. J. Separating Parkinson’s disease from normality. Discriminant function analysis of fluorodopa F 18 positron emission tomography data. Arch. Neurol. 51, 237–243 (1994).
Jokinen, P. et al. Simple ratio analysis of 18F-fluorodopa uptake in striatal subregions separates patients with early Parkinson disease from healthy controls. J. Nucl. Med. 50, 893–899 (2009).
Brooks, D. J. et al. Differing patterns of striatal 18F-dopa uptake in Parkinson’s disease, multiple system atrophy, and progressive supranuclear palsy. Ann. Neurol. 28, 547–555 (1990).
Otsuka, M. et al. Striatal blood flow, glucose metabolism and 18F-dopa uptake: difference in Parkinson’s disease and atypical Parkinsonism. J. Neurol. Neurosurg. Psychiatry 54, 898–904 (1991).
Otsuka, M. et al. Differentiating between multiple system atrophy and Parkinson’s disease by positron emission tomography with 18F-dopa and 18F-FDG. Ann. Nucl. Med. 11, 251–257 (1997).
Turjanski, N., Lees, A. J. & Brooks, D. J. Dopaminergic function in patients with posttraumatic parkinsonism: an 18F-dopa PET study. Neurology 49, 183–189 (1997).
Stormezand, G. N. et al. Intrastriatal gradient analyses of 18F-FDOPA PET scans for differentiation of Parkinsonian disorders. Neuroimage Clin. 25, 102161 (2020).
Scherman, D. et al. Striatal dopamine deficiency in Parkinson’s disease: role of aging. Ann. Neurol. 26, 551–557 (1989).
Kish, S. J., Shannak, K., Rajput, A., Deck, J. H. & Hornykiewicz, O. Aging produces a specific pattern of striatal dopamine loss: implications for the etiology of idiopathic Parkinson’s disease. J. Neurochem. 58, 642–648 (1992).
Burn, D. J. et al. Parkinson’s disease in twins studied with 18F-dopa and positron emission tomography. Neurology 42, 1894–1900 (1992).
Beach, T. G. et al. Reduced striatal tyrosine hydroxylase in incidental Lewy body disease. Acta Neuropathol. 115, 445–451 (2008).
Pifl, C. et al. Is Parkinson’s disease a vesicular dopamine storage disorder? Evidence from a study in isolated synaptic vesicles of human and nonhuman primate striatum. J. Neurosci. 34, 8210–8218 (2014).
Tong, J., Hornykiewicz, O. & Kish, S. J. Inverse relationship between brain noradrenaline level and dopamine loss in Parkinson disease: a possible neuroprotective role for noradrenaline. Arch. Neurol. 63, 1724–1728 (2006).
Kish, S. J. et al. Preferential loss of serotonin markers in caudate versus putamen in Parkinson’s disease. Brain 131, 120–131 (2008).
Hortnagl, H., Pifl, C., Hortnagl, E., Reiner, A. & Sperk, G. Distinct gradients of various neurotransmitter markers in caudate nucleus and putamen of the human brain. J. Neurochem. 152, 650–662 (2020).
Ehringer, H. & Hornykiewicz, O. [Distribution of noradrenaline and dopamine (3-hydroxytyramine) in the human brain and their behavior in diseases of the extrapyramidal system]. Klin. Wochenschr. 38, 1236–1239 (1960).
Bernheimer, H., Birkmayer, W., Hornykiewicz, O., Jellinger, K. & Seitelberger, F. Brain dopamine and the syndromes of Parkinson and Huntington. Clinical, morphological and neurochemical correlations. J. Neurol. Sci. 20, 415–455 (1973).
Hornykiewicz, O. Biochemical aspects of Parkinson’s disease. Neurology 51, S2–S9 (1998).
Fearnley, J. M. & Lees, A. J. Ageing and Parkinson’s disease: substantia nigra regional selectivity. Brain 114, 2283–2301 (1991).
Ma, S. Y., Roytta, M., Rinne, J. O., Collan, Y. & Rinne, U. K. Correlation between neuromorphometry in the substantia nigra and clinical features in Parkinson’s disease using disector counts. J. Neurol. Sci. 151, 83–87 (1997).
Morrish, P. K., Rakshi, J. S., Bailey, D. L., Sawle, G. V. & Brooks, D. J. Measuring the rate of progression and estimating the preclinical period of Parkinson’s disease with [18F]dopa PET. J. Neurol. Neurosurg. Psychiatry 64, 314–319 (1998).
Ross, G. W. et al. Parkinsonian signs and substantia nigra neuron density in decendents elders without PD. Ann. Neurol. 56, 532–539 (2004).
Dijkstra, A. A. et al. Stage-dependent nigral neuronal loss in incidental Lewy body and Parkinson’s disease. Mov. Disord. 29, 1244–1251 (2014).
Beach, T. G. et al. Vagus nerve and stomach synucleinopathy in Parkinson’s disease, incidental Lewy Body disease, and normal elderly subjects: evidence against the “body-first” hypothesis. J. Parkinsons Dis. 11, 1833–1843 (2021).
Blesa, J., Foffani, G., Dehay, B., Bezard, E. & Obeso, J. A. Motor and non-motor circuit disturbances in early Parkinson disease: which happens first? Nat. Rev. Neurosci. 23, 115–128 (2022).
Bergstrom, B. P. & Garris, P. A. “Passive stabilization” of striatal extracellular dopamine across the lesion spectrum encompassing the presymptomatic phase of Parkinson’s disease: a voltammetric study in the 6-OHDA-lesioned rat. J. Neurochem. 87, 1224–1236 (2003).
Edwards, R. H. Neural degeneration and the transport of neurotransmitters. Ann. Neurol. 34, 638–645 (1993).
Miller, G. W., Gainetdinov, R. R., Levey, A. I. & Caron, M. G. Dopamine transporters and neuronal injury. Trends Pharm. Sci. 20, 424–429 (1999).
Caudle, W. M., Colebrooke, R. E., Emson, P. C. & Miller, G. W. Altered vesicular dopamine storage in Parkinson’s disease: a premature demise. Trends Neurosci. 31, 303–308 (2008).
Sulzer, D. et al. Neuromelanin biosynthesis is driven by excess cytosolic catecholamines not accumulated by synaptic vesicles. Proc. Natl Acad. Sci. USA 97, 11869–11874 (2000).
Liang, C. L., Nelson, O., Yazdani, U., Pasbakhsh, P. & German, D. C. Inverse relationship between the contents of neuromelanin pigment and the vesicular monoamine transporter-2: human midbrain dopamine neurons. J. Comp. Neurol. 473, 97–106 (2004).
Wimalasena, K. Vesicular monoamine transporters: structure-function, pharmacology, and medicinal chemistry. Med. Res. Rev. 31, 483–519 (2011).
Eaton, A. F., Merkulova, M. & Brown, D. The H+-ATPase (V-ATPase): from proton pump to signaling complex in health and disease. Am. J. Physiol. Cell Physiol. 320, C392–C414 (2021).
Shao, E. & Forgac, M. Involvement of the nonhomologous region of subunit A of the yeast V-ATPase in coupling and in vivo dissociation. J. Biol. Chem. 279, 48663–48670 (2004).
Schapira, A. H. et al. Mitochondrial complex I deficiency in Parkinson’s disease. J. Neurochem. 54, 823–827 (1990).
Simunovic, F. et al. Gene expression profiling of substantia nigra dopamine neurons: further insights into Parkinson’s disease pathology. Brain 132, 1795–1809 (2009).
Elstner, M. et al. Expression analysis of dopaminergic neurons in Parkinson’s disease and aging links transcriptional dysregulation of energy metabolism to cell death. Acta Neuropathol. 122, 75–86 (2011).
Tiklova, K. et al. Disease duration influences gene expression in neuromelanin-positive cells from Parkinson’s disease patients. Front. Mol. Neurosci. 14, 763777 (2021).
Steinkellner, T. et al. Dopamine neurons exhibit emergent glutamatergic identity in Parkinson’s disease. Brain 145, 879–886 (2022).
Keeney, M. T. et al. NADPH oxidase 2 activity in Parkinson’s disease. Neurobiol. Dis. 170, 105754 (2022).
Di Maio, R. et al. LRRK2 activation in idiopathic Parkinson’s disease. Sci. Transl. Med. 10, eaar5429 (2018).
Montine, T. J. et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta Neuropathol. 123, 1–11 (2012).
McKeith, I. G. et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology 89, 88–100 (2017).
Attems, J. et al. Neuropathological consensus criteria for the evaluation of Lewy pathology in post-mortem brains: a multi-centre study. Acta Neuropathol. 141, 159–172 (2021).
Blesa, J. et al. The nigrostriatal system in the presymptomatic and symptomatic stages in the MPTP monkey model: a PET, histological and biochemical study. Neurobiol. Dis. 48, 79–91 (2012).
Acknowledgements
Tissue for this study was provided by the Newcastle Brain Tissue Resource, which is funded in part by a grant from the UK Medical Research Council (grant number G0400074) and by Brains for Dementia Research, a joint venture between Alzheimer’s Society and Alzheimer’s Research UK. L.Z. acknowledges the support of the Grigioni Foundation for Parkinson’s Disease (Milan, Italy).
Author information
Authors and Affiliations
Contributions
Conceptualization: C.P.; execution: C.P., H.R.; statistical analysis: C.P.; resources: J.A.; funding acquisition: L.Z.; writing—original draft: C.P.; writing—review & editing: C.P., J.A., L.Z.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pifl, C., Reither, H., Attems, J. et al. Dopamine and vesicular monoamine transport loss supports incidental Lewy body disease as preclinical idiopathic Parkinson. npj Parkinsons Dis. 9, 89 (2023). https://doi.org/10.1038/s41531-023-00514-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41531-023-00514-z
This article is cited by
-
Cortical Lewy body injections induce long-distance pathogenic alterations in the non-human primate brain
npj Parkinson's Disease (2023)