Abstract
Astronauts on the International Space Station are exposed to levels of atmospheric carbon dioxide (CO2) above typical terrestrial levels. We explored the possibility that increased levels of ambient CO2 further stimulate bone resorption during bed rest. We report here data from 2 ground-based spaceflight analog studies in which 12 male and 7 female subjects were placed in a strict 6° head-down tilt (HDT) position for either 30 days at 0.5% ambient CO2 or 60 days with nominal environmental exposure to CO2. Bone mineral density (BMD) and bone mineral content (BMC) were determined using dual-energy X-ray absorptiometry (DXA). Blood and urine were collected before and after HDT for biochemical analysis. No change was detected in either BMD or BMC, as expected given the study duration. Bone resorption markers increased after bed rest as expected; however, elevated CO2 had no additive effect. Elevated CO2 did not affect concentrations of minerals in serum and urine. Serum parathyroid hormone and 1,25-dihydroxyvitamin D were both reduced after bed rest, likely secondary to calcium efflux from bone. In summary, exposure to 0.5% CO2 for 30 days did not exacerbate the typical bone resorption response observed after HDT bed rest. Furthermore, results from these strict HDT studies were similar to data from previous bed rest studies, confirming that strict 30–60 days of HDT can be used to evaluate changes in bone metabolism. This is valuable in the continuing effort to develop and refine efficacious countermeasure protocols to mitigate bone loss during spaceflight in low-Earth orbit and beyond.
Similar content being viewed by others
Introduction
Space is a hostile environment that brings many health risks for astronauts. The loss of bone mineral and muscle tissue are particularly well-documented outcomes of spaceflight1,2,3,4. Long-duration space missions on Skylab, Mir, and the International Space Station (ISS) have all resulted in some degree of bone loss1,5,6,7,8,9. Kidney calcification and renal stone formation are potential byproducts because calcium is released from bone when the body is unloaded in a microgravity environment1,5,6,8,10. To ensure the success of future human space exploration missions, it is important to understand the factors that might induce detrimental changes in the mass and the structure of bone so countermeasures can be developed to mitigate these changes.
One of the factors that could contribute to spaceflight-induced bone loss is exposure to elevated atmospheric carbon dioxide (CO2). Airflow is limited in spacecrafts and resources to scrub CO2 from the atmosphere are constrained, which is conducive to higher ambient CO2 levels11. In fact, on the ISS, CO2 levels are often about 0.5% (5000 ppm)11, over 10 times higher than ambient outdoor terrestrial levels12. Exposure to increased levels of CO2 can result in many health issues, including cognition deficits, headaches, and detrimental effects on bone health11,12.
Bed rest is a common analog used to assess human physiology responses to the microgravity environment of spaceflight. The bone hyperresorption induced by bed rest is well-documented to reflect hyperresorption induced by actual spaceflight, although at a lesser magnitude1,7,8,13,14. Subjects are placed in a 6° head-down tilt (HDT) position during bed rest, which reduces the typical mechanical forces on the bone, leading to bone resorption as the bone adapts to decreased weight and pressure15. Because bone exists in a dynamic equilibrium between formation and resorption, under reduced mechanical loading, the bone adjusts to the decreased need for strength by increasing resorption, which then outpaces formation, leading to bone loss16. Although bed rest is not a quantitative replica of spaceflight conditions, it produces the same qualitative effects such as bone loss1,17,18,19, decreased calcium absorption20 and increased urinary and fecal excretion of calcium13,14,20,21, leading to a negative calcium balance7,9,20. During many previous bed rest studies, subjects were allowed to prop their head up using a pillow; however to maintain the 6° angle on the head during strict HDT, no pillows were used. This was initiated to increase headward fluid pressure to more closely mimic the physiological effects of spaceflight.
A state of acidosis in the body induces several factors that affect bone metabolism, and these could exacerbate spaceflight or bed-rest induced bone loss. It is hypothesized that CO2 levels between 0.7–1.0%22 and diets with high potential renal acid load (PRAL) may trigger metabolic acidosis23,24. Bone acts as a buffer during metabolic acidosis by stimulating osteoclasts to release calcium carbonate to negate the acidosis25, resulting in hypercalciuria11,26 and a negative calcium balance27. CO2 levels greater than 0.7–1.0%27 prompt cyclic periods of respiratory and metabolic acidosis22,28 mirrored by fluctuations in the levels of circulating calcium and phosphorus as they are released from bone29. Contrary to metabolic acidosis, respiratory acidosis triggers renal absorption of bicarbonate to buffer the increased pCO222, and conflicting results have been reported regarding the effects on calcium regulation27. Some studies report an increase in urinary calcium28,30, whereas others report calcium retention11 or minimal to no change at all31 in response to respiratory acidosis. The precise level of CO2 known to trigger metabolic or respiratory acidosis in humans has never been clarified as it largely depends on individual metabolic responses to the exposure.
To our knowledge no studies have examined how CO2 levels affect bone loss during bed rest. Thus, we sought to determine how bone responds to 0.5% CO2 during strict HDT bed rest. Because the average ambient concentration of CO2 on the ISS is 0.5%12, the results of this study can help interpret the qualitative physiological changes in astronauts on the ISS. Guinea pig exposure to 0.5% CO2 for 8 weeks has resulted in kidney calcification and elevated plasma calcium levels, thus indicating 0.5% CO2 has a measurable physiological impact32. While it is unlikely metabolic or respiratory acidosis will be observed at such low levels of exposure, kidney calcification and calcium efflux from bone are both direct health risks to astronauts. Elevated CO2 exposure will continue to be a risk as space exploration missions extend beyond low-Earth orbit, so it is important to evaluate how CO2 impacts the body to determine an acceptable exposure level.
Results
Densitometry
The body mass of the elevated CO2 group and the control group was the same after strict bed rest as it was before bed rest (Table 1). As expected, 30–60 days of bed rest induced only minor changes in bone densitometry findings in both groups of subjects (Table 1).
Biochemistry
Bone resorption, as assessed from levels of excreted collagen crosslinks, increased after 30 and 60 days of strict HDT bed rest, but was not exacerbated by exposure to elevated levels of CO2 (Table 2). Collagen crosslinks N-telopeptide (NTX) excretion was greater in the control group before and after bed rest than the excretion levels in the CO2 group (expressed as ug/g, P < 0.05, or nmol/d, post-hoc P < 0.01). Deoxypyridinoline (DPD) excretion following bed rest was greater in the control groups compared to the CO2 group (P < 0.05); however, this interaction effect was only observed when the data were normalized to creatinine (Table 2). Levels of crosslink excretion in these 2 strict HDT studies were similar to values reported for earlier bed rest studies7,13,14,21,33,34,35,36 (Fig. 1).
Urinary calcium, n-telopeptide, parathyroid hormone (PTH), and bone-specific alkaline phosphatase (BSAP) before (Pre), and during bed rest (BR15, BR30, or BR60) comparing several bed rest studies of similar duration. Data are means ± SD. The control data from this study are the solid black line and filled circle (AGBRESA Control) and the subjects exposed to 0.5% CO2 during bed rest are the solid line with filled squares. Comparable bed rest studies are in gray with dashed lines9,13,14,16,18,21,33,34,35,47,65,66.
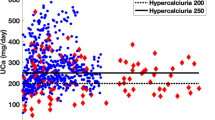
Bone-specific alkaline phosphatase (BSAP), a marker of bone formation, tended to increase after bed rest but did not reach statistical significance (post-hoc P = 0.09, Table 2). However, after bed rest, serum type 1 procollagen (P1NP) concentration, another indication of bone formation, increased 44 ± 35% above pre-bed rest levels in the control group (interaction P < 0.01), and increased 14 ± 15% above pre-bed rest levels in the elevated CO2 group (Table 2). Concentrations of serum osteocalcin in the control group were 19 ± 14% higher on the last day of bed rest than they were before bed rest, but were unchanged after bed rest in the elevated CO2 group (interaction P < 0.01) (Table 2). Concentrations of circulating parathyroid hormone (PTH) decreased after bed rest by 27 ± 26% and 19 ± 20% in the control and elevated CO2 groups, respectively (post-hoc P < 0.001). Similarly, concentrations of 1,25 (OH)2 vitamin D in both groups of subjects were less after bed rest than before bed rest (−29 ± 11% and −34 ± 18% in the control and in the elevated CO2 groups, respectively). In the control group, 25(OH) vitamin D levels were 13 ± 10% higher after bed rest than before bed rest, but no differences were detected in 25(OH) vitamin D levels in the elevated CO2 group. Bed rest-induced changes in serum vitamin K were also different in each group of subjects (interaction P < 0.001): the control group had a significant increase in serum vitamin K after bed rest (104 ± 85%) as compared to pre-bed rest values, whereas no changes were detected in the elevated CO2 group (Table 3). Although concentrations of magnesium in the serum were unaffected by bed rest or treatment, levels of magnesium in the urine were lower after bed rest than before, especially in the control group where urine magnesium was 40 ± 13% lower than values before bed rest (interaction P < 0.01) (Table 3). Before bed rest, the control subjects had higher levels of magnesium in their urine than the elevated CO2 subjects (interaction P < 0.01). Levels of serum calcium were higher (post-hoc P < 0.001) after bed rest than before bed rest but values were unaffected by CO2 exposure. Excretion of urinary calcium tended to increase in the control group and decrease in the elevated CO2 group after bed rest (interaction P = 0.058). For both groups of subjects, levels of serum phosphorus were higher (post-hoc P < 0.001) after bed rest than before bed rest, whereas urine phosphate was lower after bed rest but decreased to a greater extent in the control group (interaction P < 0.01). The serum concentrations of potassium and sodium were unaffected by bed rest and CO2 exposure, but sodium levels in urine were lower in both groups after bed rest (post-hoc P < 0.001), and potassium levels in the urine were lower in the control group after bed rest (interaction P < 0.05). Other chemistry results are shown in Table 2.
Blood pH increased slightly, but significantly, in the elevated CO2 group after bed rest (interaction P < 0.01), rising 0.3 ± 1.4%. The capillary whole blood bicarbonate concentration increased (interaction P < 0.01) after bed rest (11 ± 6%) in the elevated CO2 group, whereas no change was observed in the control group. The pCO2 increased after bed rest (post-hoc P < 0.01) in both groups of subjects (Table 4).
Diet
Dietary intake data are reported in Table 5. Vitamin K intake was similar for both groups of subjects before bed rest, and a small but significant decline was detected in the elevated CO2 group (interaction P < 0.001).
Discussion
Exposure to 0.5% CO2 for 30 days did not exacerbate markers predicting bone loss during strict HDT bed rest. However, this study did corroborate previous physiological effects of prolonged bed rest without strict HDT, including elevated markers of bone resorption8,9,13,15,16, increased urinary calcium excretion13,14,35, and decreased concentrations of serum PTH9,13,16,19,20,26,33 and 1,25 vitamin D1,16,20 that are often observed in bed rest studies of similar duration. In the present study, urinary calcium tended to increase after bed rest in the control group (P = 0.058), but did not reach statistical significance.
No measurable change was detected in the density or content of bone mineral in either the elevated CO2 group or the control group. This was expected, however, because it typically takes 90 days or more of bed rest for measurable changes to occur in bone mineral content (BMC) and bone mineral density (BMD) using DXA. The lack of change is consistent with data from other bed rest studies of similar durations9,14,21.
Whereas imaging techniques cannot quantify the small degree of bone loss that occurs in short-term studies such as the one reported here, collagen crosslinks provide biochemical evidence of bone resorption that ultimately lead to BMD or BMC changes, and the crosslinks respond within first days of bed rest37. An interaction effect was detected in the crosslink DPD when normalized to ug/g creatinine in that DPD increased more in the control group after bed rest. The interaction effect was likely due to subject variation because creatinine may yield abnormal results from a myriad of nonspecific factors which could interfere with the creatinine estimate up to 15%. These factors include simple day-to-day variations, emotional stress, or menstrual cycles, all of which may have impacted the subjects. A bed rest effect but no interaction effect was detected when DPD was expressed in nmol/d. NTX is often considered a more reliable marker of bone resorption, and the percent increases in NTX during the control (37.1 ± 31.0%) and the CO2 (55.0 ± 67.5%) studies were within the typical 50-65% range of NTX increase reported for previous bed rest studies13,14,16,35,38 (Fig. 1).
Collagen crosslinks provide specific insight into bone resorption, whereas urinary calcium is a non-specific marker affected by many variables. Bed rest and elevated CO2 exposure had no effect on calcium excretion; however, modest increases in calcium levels were detected in the serum of both groups of subjects. PTH and active vitamin D levels both decreased as well, likely secondary to the calcium release from bone13,19. The level of 25(OH) vitamin D, a marker of vitamin D stores in the body, was significantly higher after bed rest than before bed rest in the control group, whereas the level of 25(OH) vitamin D decreased modestly in the CO2 group. Although not attributable to the CO2 exposure, these findings reinforce the impact of bed rest and decreased mechanical loading on calcium regulation and bone metabolism.
Although subjects who do not exercise during bed rest typically have no change or a slight decrease in the levels of bone formation markers while their levels of bone resorption markers and osteoclast activity rises39, our data show mixed results15. PTH decreased in both groups, as typically observed during bed rest; however, P1NP increased and BSAP tended to increase in both groups (P = 0.09), which is more consistent with bed rest studies where subjects are exercising40 or when formation and resorption are still coupled. It is possible that the CO2 exposure and bed rest did not lead to the complete uncoupling of bone formation and resorption, such that the rapid increase of bone resorption triggered a modest increase in formation, somewhat repressed in the CO2 group. However, other bed rest studies do not report increases of bone formation markers after bed rest, so this result will need to be interpreted further in other studies.
D. Bemben et al.41 examined bone marker responses utilizing the CO2 dataset, but without the control data. D. Bemben et al. similarly found that bone turnover increased as indicated by the significant increase of P1NP and serum calcium. Our data indicates that while P1NP demonstrates an interactive effect when compared to control data, the serum calcium change becomes nonsignificant. Similarly, D. Bemben et al. found that PTH significantly decreased and bone alkaline phosphatase (bone ALP) increased significantly only in women. Similar to the results of D. Bemben et al., we observed a significant interactive effect with bone ALP. However unlike D. Bemben et al., we found the PTH becomes nonsignificant when compared to the control. D. Bemben found that the bone ALP was only significant in women, which may explain our interaction effect since the number of women in the CO2 group outnumbered those in the control. While osteocalcin and 25(OH) vitamin D were determined nonsignificant by D. Bemben et al., we observed an interaction effect in both when compared to control data. Although we did not observe significant changes in BMD, D. Bemben et al. found total hip aBMD significantly decreased and was significantly greater in females.
As CO2 levels rise above terrestrial levels (e.g., ~0.04%), the body eventually enters a state of metabolic acidosis diagnosed through arterial levels of pH and bicarbonate that provoke changes in bone metabolism. The anion gap may also be calculated, as a high anion gap may signify metabolic acidosis42. A statistically significant interaction effect with group and bed rest was found for both blood pH and bicarbonate that were measured in capillary blood pH, confirming previously published data of arterialized pH43. In comparison studies, both capillary pH and bicarbonate have been found to have a strong and significant positive correlation with arterial values44. Thus, the capillary measures are a good indication of arterial dissolved gas trends. Blood pH increased in the CO2 group and decreased in the control group. Blood bicarbonate increased in both groups. The calculated anion gap remained constant in the CO2 subjects but decreased in the control subjects, which provides evidence that exposure to 0.5% CO2 for 30 days did not increase metabolic acidosis. The small decrease in anion gap could perhaps be explained by a change in albumin status42.
If metabolic acidosis were present, we could expect hypercalciuria and changes in levels of serum sodium and potassium. In chronic metabolic acidosis, serum phosphate would also rise25. No hypercalciuria was observed beyond the effects of bed rest. Urine potassium decreased only in the control group, and urine phosphate decreased the most in the control group, reinforcing that the 30-day exposure to 0.5% CO2 did not trigger a metabolic acidosis response. Respiratory acidosis also likely did not occur because PTH typically increases during respiratory acidosis and our subjects had decreased levels of PTH after bed rest45.
The lack of day-to-day biochemistry sampling is a limitation of this study. Any acute biochemical changes would not be evident in the current study because measures were only taken on the last day of bed rest.
The small differences in dietary intake could potentially explain the different effects of bed rest and CO2 exposure on serum vitamin K and osteocalcin. Vitamin K is the coenzyme essential for producing osteocalcin, so it is possible the increase in osteocalcin in the control group was due to differences in vitamin K intake. This is supported in literature which demonstrates that vitamin K intake has a significant impact on bone turnover in spaceflight46. It is also possible that the differing durations of HDT between the groups had an effect on osteocalcin.
Our data show that exposure to 0.5% CO2 does not exacerbate markers predicting bone loss during 30 days of bed rest. A buffering or acidosis response from bone has been observed with higher levels of CO2 exposure, particularly above 1.0%11,28, and it is possible that CO2 levels of 0.5% are too low to induce this effect. The threshold level for CO2-induced effects on bone loss has still to be determined for both spaceflight and terrestrial conditions.
Studies of bone mineral and muscle tissue loss during bed rest have been conducted for almost 75 years, and the design and implementation of these studies has varied with location, collaborating studies, duration, degree (if any) of HDT, and many other factors. Previous studies have assessed bone loss during 17 weeks of horizontal bed rest17,47,48, because the investigators of these studies believed that disuse, and not the fluid shifts induced by HDT, is what induces bone loss during bed rest. In the 2000s, an international group of researchers established standard bed rest protocols that employ 6° HDT in an attempt to mimic the fluid shifts induced by spaceflight49. When trying to develop a bed rest model for astronaut ocular pathologies, investigators believed that standard 6° HDT bed rest was limiting the fluid pressures in the head because subjects were using a pillow to prop their head up and they leant on an elbow while eating. The studies reported here followed what has been coined “strict HDT,” which places subjects at a 6° angle without the use of a pillow under the head. The strict adherence preserves the angle of the head, actually changing the estimated arterial blood pressure on the head from 100 mmHg at 0° to 105 mmHg at 6°50. This pressure change may contribute to the resulting optic disc edema observed in some bed rest subjects51. The data reported here match those from earlier horizontal bed rest studies (Fig. 1), even with the elevated CO2 group only exposed to HDT for 30 days and the control group exposed for 60 days. This suggests that strict HDT bed rest for 30–60 days can also be used to study unloading-induced changes in bone metabolism. This is a point of significance due to reported difficulties in finding and utilizing good models for simulating microgravity52.
This research combined biochemical, densitometry, and dietary intake data to study bone metabolism during strict HDT and elevated CO2 exposure. No evidence was detected for loss of bone mass that would affect the integrity of the bone due to exposure to 0.50% CO2 atmosphere alone, although longer-duration studies might reveal otherwise. This strict HDT study design induced similar levels of bone biochemistry responses as earlier bed rest studies without HDT. Additionally, serum 1,25(OH)2 vitamin D and PTH were reduced after bed rest in both groups of subjects, suggesting that calcium efflux from bone was indeed having a physiological impact, but there was no effect specific to CO2 exposure alone that would lead to bone mineral loss. Future research on bone metabolism at other CO2 levels is needed to better establish a risk ceiling, especially as astronauts explore beyond low-Earth orbit in vehicles that will no doubt have CO2 levels higher than terrestrial exposures.
Methods
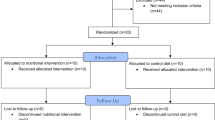
Data were obtained from the NASA Human Research Program Standard Measures Cross-Cutting Project from 2 bed rest studies: the vision impairment/intracranial pressure (VIIP) and Psychological:envihab Research Study (VaPER), a joint study between NASA and the German Aerospace Center (DLR); and the Artificial Gravity Bed Rest Study (AGBRESA), a joint study between NASA, European Space Agency (ESA), and the DLR. The studies were conducted at the DLR:envihab facility, which was designed to evaluate the physiological effects of bed rest, including bone loss. Although these overarching studies included many individual experiments, the data reported here were obtained from the NASA Standard Measures Project. Other results from these bed rest studies have been published53; however, none of the data reported herein have been previously published. NASA’s and DLR’s Institutional Review Board approved the experimental protocol and all subjects gave their written informed consent prior to participating in the study.
Bed rest studies
The VaPER study tested the physiological effects of a 30-day exposure to strict 6° HDT, and 0.5% ambient CO2 levels. VaPER consisted of a one-campaign, one-armed bed rest study without a cross-over design and lacking an ambulatory and a nominal environmental CO2 exposed control group. 11 subjects (6 male and 5 female) completed the study. Subjects underwent a 14-day baseline data collection phase (BDC) before bed rest, 30 days of sustained 6° HDT for all activities, followed by re-ambulation and recovery for 14 days. Dietary intake was standardized and controlled in accordance with the International Bed Rest Standards54. The study was performed from October 12 to December 4, 2017.
Inclusion criteria included subjects who were physically and mentally healthy, aged between 24–55 y with a BMI of 19–30 kg/m2. Subjects were required to be non-smokers for at least 6 months, and successfully complete a modified Air Force Class 3 physical. Exclusion criterial included any drug, medication, or alcohol abuse, vegetarian, have migraines, claustrophobia, eye disorders, gastro-esophageal reflux, chronic back complaints, bone fractures in either tibia or radii, muscle or joint disorder, diabetes, or history of chronic bowel disease.
The AGBRESA bed rest study tested the physiological effects of a 60-day exposure to strict 6° HDT. Although some subjects were exposed to continuous or intermittent artificial gravity treatment via centrifugation, this report only includes the 8 control subjects (2 women, 6 men) who received no artificial gravity exposure. AGBRESA consisted of 2 bed-rest campaigns, the first carried out between March 25 (first day of BDC 15 days before bed rest) and June 26, 2019 (last R + 13 data collection). The second campaign was performed between September 2, 2019 (first day of BDC 15 days before bed rest) and December 4, 2020 (last data collection 13 days after bed rest), and between September 25 (first day of BDC 14 days before bed rest) and December 23, 2019 (last data collection 13 days after bed rest). Altogether, the subjects each underwent a 15-day BDC phase, a 60-day intervention period, and a 14-day recovery phase. Dietary intakes were standardized based on the same requirements as the VaPER study. As with the VaPER study, all activities were performed in HDT during the bed rest phase, and subjects were instructed not to move their legs besides the physiotherapy and stretching they received to ease excess stiffness or pressure in targeted muscle groups.
Biological samples
Fasting blood samples and finger stick samples were collected 3 days before bed rest and again on the last day of bed rest. 24-h urine samples were collected 3 days prior to bed rest and again on the day of re-ambulation. DEXA scans were performed 14 days before bed rest and again 11 days after re-ambulation.
Urine and serum calcium were analyzed using an ion-selective electrode (MVZ Lab Quade, Cologne). 25-hydroxyvitamin D was analyzed with ADVIA Centaur Immunoassay (Siemens Healthcare Diagnostic, USA). 1,25-dihydroxyvitamin D was analyzed with chemiluminescent immunoassay (DiaSorin Inc, USA). Parathyroid hormone (PTH) and bone-specific alkaline phosphatase (BSAP) were analyzed with an immune radiometric assay (Immunotech, Czech Republic). Osteocalcin was analyzed with an enzyme-linked immunosorbent assay (ELISA) kit (Techomedical, USA). Type 1 procollagen (P1NP) was analyzed with radioimmunoassay (RIA) (Orion Diagnostica, Finland). Alkaline phosphatase, sodium, magnesium, urea nitrogen, potassium, phosphorus, and chloride were analyzed using a clinical analyzer (Atellica CH Analyzer, Siemens Healthcare Diagnostics Inc, Tarrytown, NY).
Collagen crosslinks N-telopeptide (NTX) and C-telopeptide (CTX) were analyzed in urine samples by ELISA technique (Techomedical, USA and Nordic Bioscience, Denmark, respectively). Deoxypyridinoline (DPD) and pyridinoline (PYD) were analyzed with high performance liquid chromatography (MVZ Lab Quade, Cologne). Crosslink data are presented as both excretion per day and excretion normalized to creatinine. Although 24-h excretion data provides a more reliable reflection than spot samples55, in this study, the normalized data help account for the range of body sizes given the mix of men and women in the 2 studies, and the higher proportion of men in the control group.
Three days before bed rest and on the last day of bed rest prior to reambulation, 2 arterialized capillary blood samples obtained from the index or middle finger were collected into heparinized glass capillary tubes and immediately analyzed for PO2, PCO2 and pH (ABL 800 FLEX; Radiometer, Brønshøj, Denmark).
All biochemistry analyses were performed in a Clinical Laboratory Improvement Amendment (CLIA) certified laboratory.
Bone densitometry
Bone densitometry was performed using a whole-body densitometer (GE Lunar Prodigy, enCORE software version 16) as previously described53. Briefly, single scans were performed for the following sites: whole body, lumbar spine, and hip. Due to other constraints of the studies, the left hip was scanned for VaPER and right hip was scanned for the AGBRESA study.
Dietary intake
Nutrient intake of both the AGBRESA and VaPER studies were controlled in accordance with the NASA and ESA standardization plan56. Total energy requirements for the VaPER study were calculated based on the World Health Organization formula57. AGBRESA energy requirements were calculated based on resting metabolic rate measurements. Because energy requirements are lower during bed rest, energy provision was adjusted throughout the studies to maintain the subjects’ body weights within 3% of the weight on the third day of bed rest, at which point fluid redistribution and loss were completed. All subjects consumed standardized meals: a 7-day meal plan before and after bed rest, and a standard 14-day meal plan that was implemented previously for :envihab long-term bed rest studies43. Subjects were expected to eat all of their food at each meal and were given an isocaloric diet based on NASA spaceflight nutritional requirements with a balanced intake of macro- and micronutrients and a ratio of 50 to 55% carbohydrate, <35% fat, and 12–15% protein. Subjects consumed a daily standardized level of water based on their weight (50 mL of fluid intake per 1 kg body weight), and they could add lemon juice to the water but were not allowed cocoa, chocolate, tea, alcoholic beverages, herbal drinks, or caffeinated beverages. The results of the vitamin D test during subject screening determined whether a subject received a 2000 IU vitamin D supplement before the HDT phase. Because the efficiency of vitamin D supplementation depends on baseline 25-hydroxyvitamin D and fat and body mass58, vitamin D supplementation was initiated 8 weeks prior to the start of bed rest, taking into account body weight and baseline status. The total loading dose used (IU) = 40 × (75 - 25-hydroxyvitamin D (nmol/L) × body weight (kg))59,60,61,62. Recommended daily doses in this phase ranged from 500–2500 IU vitamin D3/d. All subjects received a daily 1000 IU vitamin D supplement during the HDT phase. Dietary data were recorded with the PRODI Nutrition software (Kluthe, Prodi expert, Stuttgart, Germany).
The Potential Renal Acid Load (PRAL) of the diet was calculated using a formula from Pedone63 and Remer64: (0.49 × total protein intake) + (0.037 × phosphorus intake) – (0.021 × potassium intake) – (0.026 × magnesium intake) – (0.013 × calcium intake). The absolute PRAL was calculated from the total nutrients consumed, whereas the weight-adjusted PRAL was calculated from the nutrients consumed divided by kg of body mass. Anion gap (AG) was calculated using the equation: AG = [Na+] – ([Cl−] + [HCO3−]).
Statistical analysis
Two-factor repeated measures ANOVA tests were used to determine the group and interactive effect of the treatment (elevated CO2 or control) and study phase (before or after bed rest) on the biochemical markers and the bone densitometry in the areas of interest. Post hoc Bonferroni t-tests were conducted to determine the difference between groups when the ANOVA yielded significant interactions of P < 0.05 (Sigma Plot 12.0, Systat Software Inc., Palo Alto, CA). The biochemical markers were log or 1/x transformed to attain normal distributions. Because serum alkaline phosphatase, serum sodium, serum vitamin K, serum vitamin D, and BSAP could not be normalized, statistics were performed on raw data. The elevated CO2 group contained an outlier with values of blood pH greater than 3 standard deviations from the mean. Removing the outlier did not change the statistical significance so the outlier datum was kept. Diet data were not analyzed statistically due to both studies strictly controlling dietary protocols to the same specifications. However, vitamin K status was analyzed and compared between the elevated CO2 and control groups because there was a difference in serum vitamin K status between groups.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data from this paper are available upon request through the NASA Life Science Data Archive.
References
Smith, S. M. et al. Fifty years of human space travel: implications for bone and calcium research. Annu. Rev. Nutr. 34, 377–400 (2014).
Smith, S. M. & Zwart, S. R. Nutritional biochemistry of spaceflight. Adv. Clin. Chem. 46, 87–130 (2008).
LeBlanc, A. et al. Bone mineral and lean tissue loss after long duration space flight. J. Musculoskelet. Neuronal Interact. 1, 157–160 (2000).
Smith, S. M., Zwart, S. R., Douglas, G. L. & Heer, M. Human adaptation to spaceflight: The role of food and nutrition. 2nd edition (NP-2021-03-003-JSC). (National Aeronautics and Space Administration Lyndon B. Johnson Space Center, 2021).
Smith, S. M. et al. Bone markers, calcium metabolism, and calcium kinetics during extended-duration space flight on the Mir space station. J. Bone Miner. Res. 20, 208–218 (2005).
Smith, S. M. et al. Bone metabolism and renal stone risk during International Space Station missions. Bone 81, 712–720 (2015).
Smith, S. M. et al. Collagen cross-link excretion during space flight and bed rest. J. Clin. Endocrinol. Metab. 83, 3584–3591 (1998).
Zwart, S. R. & Smith, S. M. The impact of space flight on the human skeletal system and potential nutritional countermeasures. Int. SportMed. J. 6, 199–214 (2005).
Smith, S. M. et al. Effects of artificial gravity during bed rest on bone metabolism in humans. J. Appl. Physiol. (1985) 107, 47–53 (2009).
Smith, S. M. et al. Men and women in space: bone loss and kidney stone risk after long-duration spaceflight. J. Bone Miner. Res. 29, 1639–1645 (2014).
Drummer, C. et al. Effects of elevated carbon dioxide environment on calcium metabolism in humans. Aviat. Space Environ. Med. 69, 291–298 (1998).
Law, J. et al. Relationship between carbon dioxide levels and reported headaches on the international space station. J. Occup. Environ. Med. 56, 477–483 (2014).
Morgan, J. L. L. et al. Bone metabolism and nutritional status during 30-day head-down-tilt bed rest. J. Appl Physiol. (1985) 113, 1519–1529 (2012).
Zwart, S. R. et al. Lower body negative pressure treadmill exercise as a countermeasure for bed rest-induced bone loss in female identical twins. Bone 40, 529–537 (2007).
Spector, E. R., Smith, S. M. & Sibonga, J. D. Skeletal effects of long-duration head-down bed rest. Aviat. Space Environ. Med. 80, A23–28 (2009).
Smith, S. M. et al. Evaluation of treadmill exercise in a lower body negative pressure chamber as a countermeasure for weightlessness-induced bone loss: a bed rest study with identical twins. J. Bone Miner. Res. 18, 2223–2230 (2003).
LeBlanc, A. D., Schneider, V. S., Evans, H. J., Engelbretson, D. A. & Krebs, J. M. Bone mineral loss and recovery after 17 weeks of bed rest. J. Bone Miner. Res. 5, 843–850 (1990).
Morgan, J. L. L. et al. Rapidly assessing changes in bone mineral balance using natural stable calcium isotopes. Proc. Natl Acad. Sci. USA 109, 9989–9994 (2012).
Buehlmeier, J. et al. Markers of bone metabolism during 14 days of bed rest in young and older men. J. Musculoskelet. Neuronal Interact. 17, 399–408 (2017).
LeBlanc, A. et al. Calcium absorption, endogenous excretion, and endocrine changes during and after long-term bed rest. Bone 16, 301S–304S (1995).
Morgan, J. L. L. et al. Sex-specific responses of bone metabolism and renal stone risk during bed rest. Physiol. Rep. 2, 1–12 (2014).
Schaefer, K. E., Pasquale, S., Messier, A. A. & Shea, M. Phasic changes in bone CO2 fractions, calcium, and phosphorus during chronic hypercapnia. J. Appl Physiol. Respir. Environ. Exerc Physiol. 48, 802–811 (1980).
Bushinsky, D. A. Metabolic alkalosis decreases bone calcium efflux by suppressing osteoclasts and stimulating osteoblasts. Am. J. Physiol. 271, F216–222 (1996).
Jacobson, T. A. et al. Direct human health risks of increased atmospheric carbon dioxide. Nat. Sustainability 2, 691–701 (2019).
Bushinsky, D. A. et al. Acute acidosis-induced alteration in bone bicarbonate and phosphate. Am. J. Physiol. Ren. Physiol. 283, F1091–1097 (2002).
Smith, S. M., Heer, M. & Zwart, S. R. In Nutrition and bone health, 2nd ed. (eds. M. Holick & J. Nieves) Ch. 41, 687–705 (Springer, 2015).
Bushinsky, D. A. & Sessler, N. E. Critical role of bicarbonate in calcium release from bone. Am. J. Physiol. 263, F510–515 (1992).
Messier, A. A. et al. Calcium, magnesium, and phosphorus metabolism, and parathyroid-calcitonin function during prolonged exposure to elevated CO2 concentrations on submarines. Undersea Biomed. Res. 6, S57–70 (1979).
Alexander, R. T., Cordat, E., Chambrey, R., Dimke, H. & Eladari, D. Acidosis and urinary calcium excretion: insights from genetic disorders. J. Am. Soc. Nephrol. 27, 3511–3520 (2016).
Canzanello, V. J. et al. Effect of chronic respiratory acidosis on urinary calcium excretion in the dog. Kidney Int. 38, 409–416 (1990).
Frick, K. K. & Bushinsky, D. A. Effect of metabolic and respiratory acidosis on intracellular calcium in osteoblasts. Am. J. Physiol. Ren. Physiol. 299, F418–425 (2010).
Schaefer, K. E., Douglas, W. H., Messier, A. A., Shea, M. L. & Gohman, P. A. Effect of prolonged exposure to 0.5% CO2 on kidney calcification and ultrastructure of lungs. Undersea Biomed. Res. 6, S155–161 (1979).
Austermann, K. et al. Antioxidant supplementation does not affect bone turnover markers during 60 days of 6 degrees head-down tilt bed rest: results from an exploratory randomized controlled trial. J. Nutr. 151, 1527–1538 (2021).
Heer, M. et al. Effects of high-protein intake on bone turnover in long-term bed rest in women. Appl Physiol. Nutr. Metab. 42, 537–546 (2017).
Smith, S. M. et al. WISE-2005: supine treadmill exercise within lower body negative pressure and flywheel resistive exercise as a countermeasure to bed rest-induced bone loss in women during 60-day simulated microgravity. Bone 42, 572–581 (2008).
Zwart, S. R., Hargens, A. R. & Smith, S. M. The ratio of animal protein intake to potassium intake is a predictor of bone resorption in space flight analogues and in ambulatory subjects. Am. J. Clin. Nutr. 80, 1058–1065 (2004).
Baecker, N. et al. Bone resorption is induced on the second day of bed rest: results of a controlled crossover trial. J. Appl Physiol. (1985) 95, 977–982 (2003).
Zwart, S. R. et al. Amino acid supplementation alters bone metabolism during simulated weightlessness. J. Appl Physiol. (1985) 99, 134–140 (2005).
Heer, M., Baecker, N., Mika, C., Boese, A. & Gerzer, R. Immobilization induces a very rapid increase in osteoclast activity. Acta Astronaut 57, 31–36 (2005).
Cavanagh, P. R. et al. Replacement of daily load attenuates but does not prevent changes to the musculoskeletal system during bed rest. Bone Rep. 5, 299–307 (2016).
Bemben, D. A., Baker, B. S., Buchanan, S. R. & Ade, C. J. Circulating MiR-21 expression is upregulated after 30 days of head-down tilt bed rest. Osteoporos. Int. 32, 1369–1378 (2021).
Kraut, J. A. & Nagami, G. T. The serum anion gap in the evaluation of acid-base disorders: what are its limitations and can its effectiveness be improved. Clin. J. Am. Soc. Nephrol. 8, 2018–2024 (2013).
Laurie, S. S. et al. Unchanged cerebrovascular CO2 reactivity and hypercapnic ventilatory response during strict head-down tilt bed rest in a mild hypercapnic environment. J. Physiol. 598, 2491–2505 (2020).
Heidari, K. et al. Correlation between capillary and arterial blood gas parameters in an ED. Am. J. Emerg. Med. 31, 326–329 (2013).
Lopez, I., Aguilera-Tejero, E., Estepa, J. C., Rodriguez, M. & Felsenfeld, A. J. Role of acidosis-induced increases in calcium on PTH secretion in acute metabolic and respiratory acidosis in the dog. Am. J. Physiol. Endocrinol. Metab. 286, E780–785 (2004).
Heer, M. Nutritional interventions related to bone turnover in European space missions and simulation models. Nutrition 18, 853–856 (2002).
Shackelford, L. C. et al. Resistance exercise as a countermeasure to disuse-induced bone loss. J. Appl Physiol. (1985) 97, 119–129 (2004).
LeBlanc, A. D. et al. Regional changes in muscle mass following 17 weeks of bed rest. J. Appl Physiol. (1985) 73, 2172–2178 (1992).
Cromwell, R. L. et al. Overview of the NASA 70-day Bed Rest Study. Med. Sci. Sports Exerc., https://doi.org/10.1249/MSS.0000000000001617 (2018).
Hargens, A. R. & Vico, L. Long-duration bed rest as an analog to microgravity. J. Appl Physiol. (1985) 120, 891–903 (2016).
Zwart, S. R. et al. Association of genetics and B vitamin status with the magnitude of optic disc edema during 30-day strict head-down tilt bed rest. JAMA Ophthalmol. 137, 1195–1200 (2019).
Vico, L. et al. Effects of a 120 day period of bed-rest on bone mass and bone cell activities in man: attempts at countermeasure. Bone Min. 2, 383–394 (1987).
Clément, G. R. et al. International standard measures during the VaPER bed rest study. Acta Astronaut 190, 208–217 (2022).
Sundblad, P. et al. Guidelines for standardization of bed rest studies in the spaceflight cont`t. (International Academy of Astronautics (IAA) 2014).
Smith, S. M., Dillon, E. L., DeKerlegand, D. E. & Davis-Street, J. E. Variability of collagen crosslinks: impact of sample collection period. Calcif. Tissue Int. 74, 336–341 (2004).
Sundblad, P., Orlov, O., Angerer, O., Larina, I. & Cromwell, R. Standardization of bed rest studies in the spaceflight context. J. Appl Physiol. (1985) 121, 348–349 (2016).
World Health Organization. Energy and protein requirements. Report of a joint FAO/WHO/UNU expert consultation. Vol. 724 1–206 (World Health Organization, 1985).
Lee, P., Greenfield, J. R., Seibel, M. J., Eisman, J. A. & Center, J. R. Adequacy of vitamin D replacement in severe deficiency is dependent on body mass index. Am. J. Med. 122, 1056–1060 (2009).
van Groningen, L. et al. Cholecalciferol loading dose guideline for vitamin D-deficient adults. Eur. J. Endocrinol. 162, 805–811 (2010).
Aloia, J. F. et al. Vitamin D intake to attain a desired serum 25-hydroxyvitamin D concentration. Am. J. Clin. Nutr. 87, 1952–1958 (2008).
Heaney, R. P., Davies, K. M., Chen, T. C., Holick, M. F. & Barger-Lux, M. J. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am. J. Clin. Nutr. 77, 204–210 (2003).
Barger-Lux, M. J., Heaney, R. P., Dowell, S., Chen, T. C. & Holick, M. F. Vitamin D and its major metabolites: serum levels after graded oral dosing in healthy men. Osteoporos. Int. 8, 222–230 (1998).
Pedone, C. et al. Quality of diet and potential renal acid load as risk factors for reduced bone density in elderly women. Bone 46, 1063–1067 (2010).
Remer, T., Dimitriou, T. & Manz, F. Dietary potential renal acid load and renal net acid excretion in healthy, free-living children and adolescents. Am. J. Clin. Nutr. 77, 1255–1260 (2003).
Spatz, J. M. et al. Serum sclerostin increases in healthy adult men during bed rest. J. Clin. Endocrinol. Metab. 97, E1736–1740 (2012).
Ploutz-Snyder, L. L. et al. Exercise training mitigates multisystem deconditioning during bed rest. Med. Sci. Sports Exerc. 50, 1920–1928 (2018).
Acknowledgements
We would like to thank Kerry George for her excellent editorial review of the manuscript. The data reported here were from the NASA Human Research Program Standard Measures Cross-Cutting Project. Funding was provided by the NASA Human Research Program’s Human Health Countermeasures Element. ERM was funded through a summer fellowship with the NASA Space Life Sciences Summer Institute.
Author information
Authors and Affiliations
Contributions
S.R.Z., S.M.S., J.S., P.F.M., M.H., G.R.C., and E.M. designed, proposed, and implemented the study. E.R.M., J.S., S.M.S., and S.R.Z. reviewed and interpreted data. E.R.M. performed statistical analyses and wrote the first draft of the manuscript. P.F.M., J.S., M.H., G.R.C., E.M., S.M.S. and S.R.Z. contributed to development of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McGrath, E.R., Frings-Meuthen, P., Sibonga, J. et al. Bone metabolism during strict head-down tilt bed rest and exposure to elevated levels of ambient CO2. npj Microgravity 8, 57 (2022). https://doi.org/10.1038/s41526-022-00245-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41526-022-00245-0