Abstract
We report the 20-year rate of ipsilateral breast event (IBE) for patients with ductal carcinoma in situ (DCIS) treated with lumpectomy without radiation on a non-randomized prospective clinical trial. Patients were enrolled in cohort 1: low- or intermediate-grade DCIS, size ≤ 2.5 cm (n = 561); or cohort 2: high-grade DCIS, size ≤ 1 cm (n = 104). The Kaplan–Meier method was used to estimate time-to-event distributions. Cox proportional hazard methods were used to estimate hazard ratios (HRs) and tests for significance for event times. 561 patients were enrolled in cohort 1 and 104 in cohort 2. After central pathology review, 26% in cohort 1 were recategorized as high-grade and 26% in cohort 2 as low- or intermediate-grade. Mean DCIS size was similar at 7.5 mm in cohort 1 and 7.8 mm in cohort 2. Surgical margin was ≥3 mm in 96% of patients, and about 30% received tamoxifen. Median follow-up was 19.2 years. There were 104 IBEs, of which 54 (52%) were invasive. The IBE and invasive IBE rates increased in both cohorts up to 15 years, then plateaued. The 20-year IBE rates were 17.8% for cohort 1 and 28.7% for cohort 2 (p = 0.005), respectively. Invasive IBE occurred in 9.8% and 15.1% (p = 0.09), respectively. On multivariable analysis, IBE risk increased with size and was higher in cohort 2, but grade and margin width were not significantly associated with IBE. For patients with DCIS treated with excision without radiation, the rate of IBE increased with size and assigned cohort mostly in the first 15 years.
Similar content being viewed by others
Introduction
Nearly 15 years after the 2009 National Institutes of Health (NIH) State of Science Conference recommended concerted efforts to decrease indolent ductal carcinoma in situ (DCIS) diagnoses unnecessary surgeries, and excessive adjuvant treatment1, the optimal management for patients with DCIS remains controversial2, with most patients undergoing lumpectomy followed by radiotherapy (RT) and/or endocrine therapy (ET). The long-term rate of ipsilateral breast events (IBE) after wide local excision (WLE) varies substantially with clinical, pathologic, and genomic factors3,4,5,6,7,8,9, and patient selection for omission of adjuvant therapy continues to be elusive. The Radiation Therapy Oncology Group (RTOG) trial 9804 is the largest modern randomized study evaluating the impact of RT omission in patients with “good risk” DCIS. The study defined low-risk DCIS based on clinical and pathologic criteria, including mammographic detection, size ≤ 2.5 cm, margins ≥ 3 mm, and low or intermediate nuclear grade, and randomized patients to RT vs observation with or without endocrine therapy. In this study, IBE rate with and without RT increased modestly but continuously over time up to 15 years, and there was a significant reduction in recurrence rate with RT even in this highly selected group of patients with lower risk DCIS (7.1% vs. 15.1%)5. The ECOG-ACRIN Cancer Research Group E5194 is a non-randomized, prospective study of observation after WLE without RT that enrolled patients in two cohorts of patients with study-defined low-risk clinical and pathologic characteristics: cohort 1 included patients with institutionally categorized low- or intermediate-grade DCIS spanning ≤ 2.5 cm, and cohort 2 included patients with high-grade DCIS spanning ≤ 1 cm. Like RTOG 9804, endocrine therapy was given at the provider’s discretion. We have previously reported 12-year outcomes of E5195, which showed an increasing rate of IBE with time, as well as a marked separation of IBE rate between the two cohorts6. In cohort 1, the 12-year IBE rate of 14.4% was similar to that in RTOG 9804, but in cohort 2, the 12-year IBE rate was significantly higher at 24.6%. It is important to recognize that the DICS grade was re-assigned after central pathology review to align with updated pathology reporting guidelines10 after all enrollment had been completed, as reported in the 12-year data6. As a result, 26% of patients in cohort 1 had pathology up-graded to high grade, and 26% of patients in cohort 2 had pathology down-graded to low- or intermediate grade. While the differences in IBE rate between the two cohorts reported in E5194 have been widely understood to relate specifically to DCIS grade, on multivariable analysis, centrally determined DCIS grade was not associated with IBE in that analysis6. At the same time, while size criteria for the two cohorts were different, the size of DCIS in enrolled patients in both cohorts was similar, and DCIS size was strongly associated with IBE. These factors leave unanswered questions about the relationship between clinical and pathological factors and the long-term risk of IBE. Importantly, at the 12- and 15-year timepoints, there did not appear to be a reduction in IBE rate in either E5194 or RTOG 9804. The present report provides updated results of E5194 with 20-year outcomes.
Results
Patient, DCIS, and treatment characteristics
Patient, DCIS, and treatment characteristics and follow-up are summarized in Table 1. While protocol-specified size limitations for DCIS were different between cohorts, mean size was actually similar at 7.5 mm in cohort 1 and 7.8 mm in cohort 2. DCIS grade is reported as the CAP grade defined on the central pathology review, not the grade at the time of enrollment and cohort assignment. The previous publication of this study, including its appendix materials6, provides a detailed rationale and methodology for this process. In cohort 1, 50% of patient pathology specimens were classified as low grade and 50% as intermediate grade by the enrolling institution, and many were up-graded on central review: 15% remained low grade, 59% were intermediate, and 26% were high grade. In cohort 2, 100% were classified as high grades by the institution, and on re-classification, 2% were actually low grades, 24% were intermediate, and 74% remained high grades. Median follow-up from definitive surgery on the 239 patients still being followed was 19.2 years (interquartile range 17.3-20.5 years), with 205/239 (86%) followed for at least 15 years, and 87/239 (36%) followed for at least 20 years.
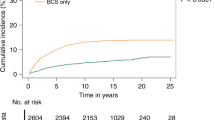
Breast cancer events
Overall, there were 104 IBEs (15.5%), 79 in cohort 1 and 25 in cohort 2, of which 54 (51%) were invasive (42 in cohort 1; 12 in cohort 2). The 20-year rates of IBE were 17.8% (95% CI 14.0%, 21.6%) for cohort 1 and 28.7% (95% CI 18.6%, 38.8%) for cohort 2 (p = 0.005; Fig. 1, Table 2). The 20-year invasive IBE rates were 9.8% (95% CI 6.9, 12.7) and 15.1% (95% CI 7.0, 23.3), respectively (p = 0.09; Fig. 1, Table 2). The rates of IBE and invasive IBE increased over time through 15 years of follow-up and then plateaued. Table 2 summarizes the 10, 15, and 20-year rates of breast events including DCIS, contralateral breast events, and survival. Development of metastatic disease has been reported for 5 patients (0.75%), 4 in cohort 1, and 1 in cohort 2; 2 of these 5 patients have died from breast cancer. In addition, 2 patients have been reported as dying from breast cancer without metastases being reported. In total, 4 patients are reported to have died from breast cancer.
Predictors of breast cancer events
Table 3 presents the IBE rate in the overall cohort by age, margin width, size, and CAP grade. Multi-factor Cox proportional hazards model analysis of IBE incidence tables is shown in Supplement 1. Cohort (1 vs. 2 hazard ratio [HR] = 1.77, 95% CI = 1.12, 2.78, p = 0.01) and increasing DCIS size (6–10 mm vs. ≤5 HR = 1.51, 95% CI 0.95, 2.40, >10 vs. ≤5 HR = 2.20, 95% CI 1.29, 3.75, p = 0.01) were significantly associated with IBE (Supplemental Table 1). Several multivariable models were prepared to evaluate the impact of CAP grade on IBE (Supplemental Table 2). When CAP grade was the only variable in the model, the estimated hazard ratio for CAP high grade vs. CAP low or intermediate grade was 1.56 (95% CI 1.01, 2.41), p = 0.04, and was 1.27 (95% CI 0.79, 2.05), p = 0.32 in the model with Cohort and tumor size. Finally, when CAP grade was analyzed in a model with size as the only other factor, the estimated hazard ratio was 1.5 (95% CI 0.97, 2.32), p = 0.07.
Two hundred patients, 175 (31%) in cohort 1 and 25 (24%) in cohort 2, received tamoxifen treatment during the study period. Tamoxifen use was also examined as a time-dependent covariate in proportional hazard models. The estimated hazard ratio for tamoxifen use vs. no tamoxifen use was 0.73 (95% CI 0.46, 1.14) p = 0.16, when tamoxifen use was the only variable in the model, and was 0.80 (95% CI 0.51, 1.27), p = 0.35 in the model with Cohort and tumor size (Table S3).
When added to the model with size and cohort, age (p = 0.34), menopause status (p = 0.24), margin width (p = 0.76), method of detection (p = 0.76), prior tamoxifen use (p = 0.23), and prior hormone replacement (p = 0.74) was not significant (Supplemental Tables 3–9). None of the factors considered for association with IBE risk showed significant association with invasive IBE risk. No differences were seen between the two cohorts for the 20-year rates of survival [64.7% (95% CI 60.1%, 69.3%) vs. 64.8% (95% CI 53.8%, 75.7%), p = 0.60].
Discussion
Prior reports of this study have demonstrated that for patients with DCIS who were selected on the basis of clinical/pathologic characteristics and treated with lumpectomy without radiation, the rates of developing an IBE and invasive IBE increased over time through 12 years of follow-up. The current report demonstrates that while IBE rates continue to increase over time, the rate is reduced after about 15 years, with minimal increases beyond that time in both cohorts of patients. Though the number of evaluable patients declined with longer follow-up, confidence intervals between 15 and 20 years remained relatively constant and at a statistically significant value. Multiple other studies also demonstrate an increase in rate over time up to 15 years3,5,11,12,13, yet few studies report a recurrence rate beyond this timeframe. The randomized SweDCIS study reported a 20-year IBE rate of 20.0% in patients receiving RT and 32.0% in those treated without RT, though the eligibility criteria for this study were much broader, requiring only that DCIS occupied a quadrant or less of the breast, without specific grade, margin, or size criteria. The hazard ratio for IBE decreased after 12 years in both arms and was close to zero for new in-situ events and remained low for invasive events; the authors speculated that RT delayed rather than prevented invasive IBE13. The finding in our analysis that the IBE rate decreases after about 15 years is thus consistent with other analyses and suggests that in a selected low-risk population of mostly postmenopausal patients, the rates of both DCIS-IBE and invasive IBE may level off over time. It is possible that this leveling-off relates to decreased incidence of new breast cancers and /or lower utilization of screening mammography in older patients, though follow-up in this dataset required an annual mammogram. Regardless of these potential explanations, the finding that the event rate levels off after 15 years is useful information for counseling patients.
Importantly, the current analysis continues to show a significant difference in IBE rate between the two cohorts. While the two cohorts were originally specified to include low/intermediate-grade DCIS up to 2.5 cm and smaller high-grade DCIS up to 1 cm, grade re-classification based on updated CAP standards resulted in significant changes, as previously described6,10. After central pathology review, 26% in cohort 1 were centrally recategorized as high-grade and 26% in cohort 2 as low- or intermediate-grade Thus, grade reclassification resulted in up-grading many patients’ pathology in cohort 1 and down-grading in cohort 26, highlighting the challenges of evaluating the impact of DCIS grade in longitudinal datasets. On the current univariable analysis evaluating CAP grade alone, CAP grade was significantly associated with 20-year IBE; however, significance was lost on multivariable analyses including size and cohort. Crude IBE rates were higher in patients with higher-grade pathology. Due to the changes in grade classification and the strong relationship between the cohort and the CAP pathology grade, it is difficult to draw strong conclusions regarding the specific impact of grade on IBE outcomes in this study, though grade is classically considered a risk factor for recurrence in most datasets5,14,15. On the other hand, though size eligibility requirements differed between the two cohorts, the mean DCIS size was similar in both cohorts, and size was the only factor other than the cohort that was significantly associated with increased IBE rates.
Thus, the underlying difference between the two cohorts is not entirely clear and highlights the fact that predictors of IBE are not fully understood. More recent efforts have focused on using molecular markers to determine the risk of recurrence after surgical excision, including the Oncotype DCIS Score (EXACT Sciences, Madison, WI)7,16 and the DCISionRT (PreludeDx, Laguna Hills, CA)8,9,17,18,19. The Oncotype DCIS Score was validated using banked tissue from E5194 and found significantly lower 10-year IBR rates in the low-risk group (IBR 10.6%) versus the intermediate-risk (IBR 26.7%) and high-risk (IBR 25.9%) groups7, but the results were not reported by the original cohort to which patients were assigned. The value of molecular markers compared with traditional clinical/pathologic features of DCIS therefore remains an area of great interest. The available data regarding these assays suggest that they may identify the risk of recurrence beyond routinely available clinicopathologic features, pointing to a need to prospectively evaluate these tests in randomized trials.
Both RTOG 9804 and E5194 allowed for the use of tamoxifen but did not specify criteria for its use. In E5194, tamoxifen was prescribed to about 30% of patients, and in RTOG 9804 58% of patients received RT versus 66% of patients not receiving RT. Tamoxifen did reduce the risk of IBE in RTOG 9804 but was not significantly associated with IBE in E5194. The relative impact of tamoxifen, or endocrine therapy in general, in reducing invasive IBE, non-invasive IBE, and contralateral breast events, and its relationship to other risk factors such as DCIS size and grade, is another area of great interest that should be evaluated in future studies. RTOG 9804 and E5914 both required margin widths of 3 mm or greater, though modern margin guidelines require only 2 mm20. Margin width beyond 3 mm was not significantly associated with IBE in either study, and the impact of smaller margins cannot be assessed here.
Methods
Patient methods
The ECOG-ACRIN E5194 study (NCT00002934) was a prospective, nonrandomized clinical trial that accrued from 1997-2002. The study protocol was approved by the National Cancer Institute Cancer Therapeutic Evaluation Program (NCI/CTEP) and then by the IRB of the respective institutional review boards of the participating centers at which the patients were enrolled. All patients gave written informed consent. Study teams complied with all relevant ethical regulations including the Declaration of Helsinki. Detailed information on trial design and conduct was previously reported6. Briefly, the study included two patient cohorts (not randomly assigned) with what was felt at the time of study design to represent low-risk clinical/pathologic characteristics: cohort 1: low- or intermediate-grade DCIS ≤ 2.5 cm (561 patients); and cohort 2: high-grade DCIS ≤ 1 cm (104 patients). As described in the introduction and previously reported, grade at the time of enrollment was determined by the enrolling site, based on standard criteria at that time21. Since the original trial design, guidelines for determining DCIS grade changed10. Central pathology review was therefore carried out on 500 of the enrolled patients (75% of all patients) after all enrollment had been completed and classifications were updated for subsequent analysis and reported as “College of American Pathologists (CAP) grade”6. Margin width was specified to be ≥3 mm in all dimensions, and 96% of pathology specimens met this criterion. All patients underwent WLE without RT. Tamoxifen was prescribed in 30% of all patients. Patients were followed with annual mammograms and breast examinations as specified in the study protocol.
Statistical methods
The primary endpoint of the study was the rate of IBE (defined as the occurrence of invasive cancer of any histology or DCIS in the treated breast). Time to first IBE was measured from primary surgery to diagnosis of invasive or non-invasive recurrence in the ipsilateral breast. Follow-up for IBEs was censored at the time of an ipsilateral mastectomy, at the time of initiation of chemotherapy for recurrent breast cancer, or at the time of the last disease evaluation. Statistical methods have been previously reported6 and are summarized here. The Kaplan–Meier method was used to estimate time-to-event distributions. Confidence intervals (CIs) were constructed using the normal approximation on the probability scale and are given at the 95% level. Cox proportional hazard methods were used to estimate hazard ratios (HRs) and tests for significance for event times. All p-values are two-sided. The multi-variable analysis of risk factors for IBE used the central pathology assignment, rather than the assigned grade at enrollment, and is referred to as the CAP grade. In conclusion: For selected lower-risk patients with DCIS treated with excision without radiation, the rate of IBE increased with size and assigned cohort through 15 years but not beyond. Further studies are needed to refine risk stratification for IBEs after a diagnosis of DCIS, including the contribution of genomic assays on clinical decision-making regarding the use of RT.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The study data used for this manuscript can be obtained by submitting a request to the ECOG-ACRIN Cancer Research Group. A request may be initiated by submitting an inquiry through the Contact Us link at https://ecog-acrin.org.
References
Allegra, C. J. et al. NIH state-of-the-science conference statement: diagnosis and management of ductal carcinoma in situ (DCIS). NIH Consens State Sci. Statements 26, 1–27 (2009).
Wright, J. L. et al. Overcoming barriers in ductal carcinoma in situ management: from overtreatment to optimal treatment. J. Clin. Oncol. 40, 225–230 (2022).
Fisher, B. et al. Lumpectomy and radiation therapy for the treatment of intraductal breast cancer: findings from national surgical adjuvant breast and bowel project B-17. J. Clin. Oncol. 16, 441–452 (1998).
Early Breast Cancer Trialists’ Collaborative Group, (EBCTCG). et al. Overview of the randomized trials of radiotherapy in ductal carcinoma in situ of the breast. J. Natl Cancer Inst. Monogr. 2010, 162–177 (2010).
McCormick, B. et al. Randomized phase III trial evaluating radiation following surgical excision for good-risk ductal carcinoma in situ: long-term report from NRG oncology/RTOG 9804. J. Clin. Oncol. 39, 3574–3582 (2021).
Solin, L. J. et al. Surgical excision without radiation for ductal carcinoma in situ of the breast: 12-year results from the ECOG-ACRIN E5194 study. J. Clin. Oncol. 33, 3938–3944 (2015).
Solin, L. J. et al. A multigene expression assay to predict local recurrence risk for ductal carcinoma in situ of the breast. J. Natl Cancer Inst. 105, 701–710 (2013).
Shah, C. et al. The clinical utility of DCISionRT® on radiation therapy decision making in patients with ductal carcinoma in situ following breast-conserving surgery. Ann. Surg. Oncol. 28, 5974–5984 (2021).
Wärnberg, F. et al. Prognostic risk assessment and prediction of radiotherapy benefit for women with ductal carcinoma in situ (DCIS) of the breast, in a randomized clinical trial (SweDCIS). Cancers (Basel) 13, 6103 (2021).
Lester, S. C. et al. Protocol for the examination of specimens from patients with ductal carcinoma in situ of the breast. Arch. Pathol. Lab. Med. 133, 15–25 (2009).
Cuzick, J. et al. Effect of tamoxifen and radiotherapy in women with locally excised ductal carcinoma in situ: long-term results from the UK/ANZ DCIS trial. Lancet Oncol. 12, 21–29 (2011).
Correa, C. et al. Overview of the randomized trials of radiotherapy in ductal carcinoma in situ of the breast. J. Natl Cancer Inst. Monogr. 2010, 162–177 (2010).
Donker, M. et al. Breast-conserving treatment with or without radiotherapy in ductal carcinoma in situ: 15-year recurrence rates and outcome after a recurrence, from the EORTC 10853 randomized phase III trial. J. Clin. Oncol. 31, 4054–4059 (2013).
Chua, B. H. et al. Radiation doses and fractionation schedules in non-low-risk ductal carcinoma in situ in the breast (BIG 3-07/TROG 07.01): a randomised, factorial, multicentre, open-label, phase 3 study. Lancet 400, 431–440 (2022).
Silverstein, M. J. et al. Prognostic classification of breast ductal carcinoma-in-situ. Lancet 345, 1154–1157 (1995).
Rakovitch, E. et al. A population-based validation study of the DCIS score predicting recurrence risk in individuals treated by breast-conserving surgery alone. Breast Cancer Res. Treat 152, 389–398 (2015).
Bremer, T. et al. A biological signature for breast ductal carcinoma in situ to predict radiotherapy benefit and assess recurrence risk. Clin. Cancer Res. 24, 5895–5901 (2018).
Vicini, F. A. et al. A novel biosignature identifies patients with DCIS with high risk of local recurrence after breast conserving surgery and radiation therapy. Int. J Radiat. Oncol. Biol. Phys. 115, 93–102 (2023).
Weinmann, S. et al. Validation of a ductal carcinoma in situ biomarker profile for risk of recurrence after breast-conserving surgery with and without radiotherapy. Clin. Cancer Res. 26, 4054–4063 (2020).
Morrow, M. et al. Society of surgical oncology–American Society for Radiation Oncology–American Society of Clinical Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in ductal carcinoma in situ. Pract. Radiat. Oncol. 6, 287–295 (2016).
Page, D. L. & Anderson, T. J. Diagnostic Histopathology of the Breast (Churchill Livingstone, 1987).
Acknowledgements
This study was coordinated by the ECOG-ACRIN Cancer Research Group (Peter J. O’Dwyer, M.D. and Mitchell D. Schnall, M.D., Ph.D., Group Co-Chairs) and supported by the National Cancer Institute of the National Institutes of Health under award numbers: U10CA180820, U10CA180794, UG1CA233196, UG1CA189858, UG1CA233328, UG1CA233290, UG1CA233247, and UG1CA233328. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We also acknowledge Drs. William C. Wood, George W. Sledge, Jr, Lorie L. Hughes, Lawrence J. Solin (in memoriam), and David L. Page (in memoriam) for their contributions to the original design, execution, and analyses of this study.
Author information
Authors and Affiliations
Contributions
Jean L.Wright: Interpretation of results, primary manuscript preparation, accountability for all aspects of work, approval of final manuscript. Robert Gray: Data management and data analyses, interpretation of results, manuscript preparation, accountability for all aspects of work, approval of final manuscript. Habib Rahbar: Interpretation of results, manuscript preparation, accountability for all aspects of work, approval of final manuscript. Christopher E. Comstock: Conceptualization and design of the study, manuscript preparation, accountability for all aspects of work, approval of final manuscript. Judy A. Tjoe: Interpretation of results, manuscript preparation, accountability for all aspects of work, approval of final manuscript. Sunil Badve: Conceptualization and design of the study Interpretation of results, accountability for all aspects of work, approval of final manuscript. Abram Recht: Interpretation of results, accountability for all aspects of work, approval of final manuscript. Joseph A. Sparano: Conceptualization and design of the study, interpretation of results, manuscript preparation, accountability for all aspects of work, approval of final manuscript. Nancy E. Davidson: Conceptualization and design of the study, interpretation of results, accountability for all aspects of work, approval of final manuscript. Antonio C. Wolff: Conceptualization and design of the study, interpretation of results, manuscript preparation, accountability for all aspects of work, approval of final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wright, J.L., Gray, R., Rahbar, H. et al. Lumpectomy without radiation for ductal carcinoma in situ of the breast: 20-year results from the ECOG-ACRIN E5194 study. npj Breast Cancer 10, 16 (2024). https://doi.org/10.1038/s41523-024-00622-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41523-024-00622-w