Abstract
Older women are under-represented in breast cancer (BC) clinical trials, and treatment guidelines are primarily based on BC studies in younger women. Studies uniformly report an increased incidence of local relapse with omission of breast radiation therapy. Review of the available literature suggests very low rates of distant relapse in women ≥70 years of age. The incremental benefit of endocrine therapy in decreasing rate of distant relapse and improving disease-free survival in older patients with low-risk BC remains unclear. Integration of molecular genomic assays in diagnosis and treatment of estrogen receptor positive BC presents an opportunity for optimizing risk-tailored adjuvant therapies in ways that may permit treatment de-escalation among older women with early-stage BC. The prevailing knowledge gap and lack of risk-specific adjuvant therapy guidelines suggests a compelling need for prospective trials to inform selection of optimal adjuvant therapy, including omission of adjuvant endocrine therapy in older women with low risk BC.
Similar content being viewed by others
Introduction
Annually, 268,600 women are diagnosed with breast cancer (BC) in North America, and of these, 30% are ≥70 years of age1. The majority present with early-stage disease and are eligible for breast conservation surgery (BCS)2,3. SEER data on the US Incidence of breast cancer subtypes by age note that majority BC among women between the age of 65–74 and ≥75 years had favorable subtype (receptor positive/HER 2 negative), 77.8% and 80.1%, respectively4. Further, triple negative and HER2 positive subtypes were less likely to be diagnosed in women over the age of 65 years.
The EBCTCG meta-analysis5 on breast radiation therapy (RT) included 10,801 women with BC derived from 17 randomized trials. The analysis demonstrates that RT reduced the rates of first loco-regional relapse (LR) and/or distant relapse (DR) by 54% (HR 0.46, 95% confidence interval (CI) 0.41–0.51, p < 0.0001). The 10-year risk of any first recurrence decreased from 31.0% to 15.6% (95% CI 13.2–17.6, 2p < 0.00001). RT reduced BC death by about a sixth (RR 0.83, 95% CI 0.73–0.95), and the 15-year risk of BC death decreased from 20.5% to 17.2% (95% CI 0.8–5.8, 2p = 0.005). Specifically, among the 1340 women ≥70 years the benefit of RT was similar (HR 0.47, 95% CI 0.33–0.66), the 10-year risk of any first recurrence LR or DR reduced from 17.7% vs. 8.8% (2p = 0.00002), including the subset of women with estrogen receptor-positive (ER+) T1 intermediate grade tumors. Contemporary RT standard of 1-week to 3-week duration is associated with reduced treatment burden and toxicity6,7,8,9,10,11,12,13,14. The implications that patients experience increased inconvenience and RT-related treatment burden are notably in reference to an outdated 5–7 weeks fractionated RT schedule.
Similarly, the benefit of endocrine therapy (ET) in reducing recurrence risk in ER + BC is established through numerous clinical trials15,16,17,18,19,20. The meta-analysis reported on 88,023 women with BC, including 66,408 with N0 disease (75.4%). Comparing 5 years of tamoxifen versus none, the updated analysis noted 39% reduction in recurrence risk (HR 0.61, 2p < 0.0001) with tamoxifen. This translated into a reduction in the annual event rate in years 0–15 from 4.7% to 3.0%19. These data and results from several clinical trials showing the benefit of ET14,15,16,17,18,19 drives our current guidelines for recommending ET × 5 years for ER + BC patients21.
Of note, many past clinical trials, and as such the meta-analysis included very few women ≥70 years16,22. Only 3972 (4.5%) women were ≥70 years in the meta-analysis. In this group, the annual event rate reduced from 5.7% vs. 3.3% (HR 0.49, SE 0.12) with tamoxifen. The rates of non-BC mortality far exceed BC-specific mortality in older women; thereby confounding the absolute clinical benefit of ET on all-cause mortality in this population.
Adjuvant endocrine therapy (ET) with omission of radiation (RT) in older women
Prior to the availability of molecular genomic assays (MGA), Phase III trials including, CALGB 9343, PRIME II, Canadian, and ABCSG 8A evaluated the omission of RT in post-menopausal women23,24,25,26,27,28 (Table 1). In all four studies, the randomization was between RT + ET versus ET alone.
Between 1994 and 1999, the CALGB 9343 trial22 randomized 636 women, ≥70 years old, with stage T1, node-negative (N0) ER + BC. RT was delivered over a 6.5-week duration (33 fractions). The 10-year LR rate with RT + ET and ET alone was 2% and 10%, respectively (p < 0.001). The overall risk of Distant Relapse (DR) was low. Specifically, 27 patients developed a DR, 10 in the RT + ET arm, and 17 in the ET arm. At a median follow-up of 12.6 years, only 21 BC deaths were reported (1% in each group), and majority of the 334/636 women had died from non-BC causes.
Between 2003 and 2009, the PRIME II trial randomized 1326 eligible women ≥65 years old with ER + BC, T-size ≤3.0 cm, and pN023,24. RT was delivered over 5-week duration (25 fractions). At a median follow-up of 10 years, Local relapse (LR) rates with RT + ET and ET alone was 0.9% and 9.8%, respectively (p < 0.0008). DR was observed in only 5 patients in RT + ET and 4 patients in ET only group. Majority of the deaths (87%) were from non-BC causes.
Between 1992 and 2000, the Canadian Trial25 randomized 769 women age ≥50 years, with ER + BC, T-size ≤5 cm, N0. The 5-year LR was 0.6% in ET + RT arm and 7.7 % in ET alone arm (p < 0.001). The disease-free survival was 91% and 84% in the ET + RT and ET alone group, respectively (p = 0.004). No differences in rate of DR (p = 0.69), and BC deaths reported was the same (n = 10) in each group.
Between 1996 and 2004, the ABCSG trial 8A randomized 869 postmenopausal patients ER + low-risk BC26,27. RT was delivered over 6 weeks (25 fractions + boost). At a median follow up of 9.8 years, the rate of LR in the RT + ET and ET alone groups was 2.5% and 7.6%, respectively (p < 0.0004), and DFS was 94.5% and 88.4%, respectively (p = 0.015). Overall, 28 patients developed DR, 16 patients in the RT + ET group, and 12 patients in the ET alone group.
While expecting modestly higher rates of LR with omission of RT, the risk of DR and BC mortality is very low in favorable risk BC. Data from these trials culminated in guideline recommendations to offer older (≥70 years) women with stage I ER + BC the option to omit breast RT when prescribing ET.
Consequences of local recurrence
Management of subsequent ipsilateral breast tumor recurrence (IBTR) requires additional surgery and adjuvant treatment. With initial omission of RT, further BCS + RT is an endorsed option for treatment of IBTR. However, available data on management of IBRT from the CALGB and PRIME II trials22,23 shows that almost 50% of older women undergo mastectomy. In the aging population, IBTR is not without risk given the psychological distress from repeat cancer events, and the complex healthcare needs as women are older and possibly frail29.
Studies using MGA-defined risk groups in ER + BC
MGA has improved prognostication and risk stratification of BC compared to clinic-pathological features only, and with some assays we gain predictive information to safely omit chemotherapy30,31,32,33. The utilization of MGA in older BC patients may further help refine risk-tailored algorithms for adjuvant ET.
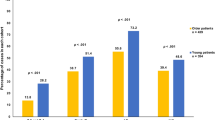
Table 2 summarizes rates of LR, DR and BC-specific mortality in women ≥70 years categorized by 21-gene Oncotype DX Recurrence Score (RS)™. The Clalit Health Services registry34 reported a higher proportion (55%) of women ≥70 years had low RS < 18 compared to younger women (45%), p = 0.004. The 5-year Kaplan–Meier estimates of DR among the 181 women ≥70 years with RS < 18 was 0.6%, and BC-specific mortality rate was 0.4%. Similarly, SEER study identified 5988 women ≥70 years of age with available RS. Among the 3424 women with pN0 and low RS (<18), and the 5-year rate of BC-specific mortality was only 1.3%35,36.
The TAILOR Rx study37,38 included 1619 women (only 113 were ≥70 years) with low RS (0–10) treated with ET alone. At 5 years, the rate of freedom from recurrence at distant site in this favorable low-risk cohort was 99.3% (95% CI, 98.7–99.6).
The EORTC 10041/BIG 3-04 MINDACT phase 3 trial39 enrolled 6693 women <70 years. In an exploratory analysis of clinical–low and genomic–ultralow-risk BC, the distant metastases-free interval (DMFI) was 97.6%, and there was no difference in DMFI between patients receiving no adjuvant treatment (NAT) and ET alone, 97.8% and 97.4%, respectively.
The RASTER40 prospective community-based observational study defined risk groups using the 70-gene signature (MammaPrint)™ risk and Adjuvant! Online (AOL). In 140 clinically/genomic identified low-risk patients who did not receive any systemic therapy, the reported 10-year rates of the distant relapse-free interval (DRFI) was 93.9% (95% CI 90.0–98.1), and BC-specific survival was 96.7% (95% CI 93.5–99.9).
It is noteworthy that the study design of all ongoing trials41,42,43,44,45 using MGA to define low-risk BC, across the board prescribe ET. Hence, despite contemporary MGA trials outcomes with omission of ET in low-risk BC will remain unaddressed.
From the summarized data, MGA regardless of stage or grade is able to identify older BC patients with extremely low rates of DR. In patients with low-risk of DR, the absolute benefits of reduction in relapse anticipated with ET similarly may be small as well. As such, the health risks and side effects may outweigh the benefits. If this relationship is indeed borne out, with prospective trials designed to test this question in women ≥70 years of age, ET may constitute overtreatment.
Adjuvant comprehensive local therapy alone with omission of endocrine therapy
There are very few randomized studies on early stage BC that includes a treatment arm with omission of ET46,47,48 (Table 3). Of note, all these studies predate the practice of integrating MGA.
Between 1982 and 1987, the NSABP B14 study21 randomized 2644 women <70 years with ER + N0 BC to receive tamoxifen + RT, and placebo + RT. The mean age of the study subjects that reported better DFS and no difference in OS (p = 0.13) with tamoxifen was 55 years. There is caution when translating an observed benefit in largely younger women to older ≥70 year women.
Between 1992 and 2000, the British Association of Surgical Oncology (BASO) II trial 45 enrolled 1135 women <70 years with ER + BC, stage T1N0, grade 1 or good prognostic subtype. In a 2 × 2 factorial design treatment arms, included surgery alone, ET alone, RT alone, and RT + ET. The highest LR was with surgery alone at 2.2% per annum, and there was no difference in LR and BC-specific survival in women treated with S + RT alone and S + ET alone.
From 1991 to 1998, the German Breast Study Group Trial V (GBSG-V)46 study with similar design as the BASO trial enrolled 361 patients between the ages of 45 and 75 years with stage T1N0 BC. At a median follow-up of 9.9 years, the reported LR rates in the surgery alone, ET alone, RT alone, or RT + ET arms were 34%, 10%, 13%, and 7%, respectively. No difference in the event-free survival was noted between S + RT alone and S + ET alone groups.
Between 1989 and 1998, the NSABP B-21 trial47 enrolled 1009 women with ER + BC, T-size <1 cm, N0 BC. Following BCS, the randomization included RT alone, tamoxifen alone, or RT + tamoxifen. A statistically significant difference in LR (p = 0.008) is noted between the 3 arms. With median follow-up of 86.9 months, no difference in rates of DR (p = 0.28) or OS (p = 0.93) was reported. In this largely low-risk study population, the rate of DR in RT only (3.2%), ET only (3.3%), and RT + ET (1.5%) groups was similar. The data showed a small number of BC deaths across treatment arms (n = 9 Tam; n = 8 RT; n = 5 ET + RT).
The Ontario population-based study49 included 5076 women age ≥65 years with T-size ≤2 cm, N0, ER + BC. The 5-year rate of DR for RT + ET was 0.43%, ET alone 0.71%, RT alone 0.71%, and 1.7% in patients receiving NAT. The 5-year OS by treatment was 95.7% RT + ET, 81.6% ET alone, 92.8% RT alone, and 71.5% NAT (p < 0.0001).
From the available randomized and population-based data, the omission of ET in early-stage low-risk BC does not signal any detrimental shifts in disease outcomes including change in rates of DR with omission of ET.
Contralateral breast cancer (CBC) risk in older women
Available data shows that age at initial diagnosis is the most important predictor of subsequent risk for CBC, and this risk exponentially decreases with increasing age of primary BC diagnosis50,51,52. Therefore, one might surmise that CBC risk is low in women ≥70 years age at diagnosis. If benefits of ET in reducing risk of CBC were demonstrably limited, older women might well desire to forgo ET and its associated negative impact on quality of life (QoL).
Endocrine therapy and quality of life
Most commonly, older postmenopausal patients are prescribed AI. However, there is an increased incidence of AI-associated bothersome skeletal events and musculoskeletal symptoms, and the rates of non-adherence to AI approaching 25–30% is not trivial53,54. Older women have a high prevalence of underlying health issues and comorbidities, which make them more susceptible to tolerating ET poorly55,56,57,58,59,60,61 (Table 4).
Prospective PRIME trial QoL studies62 illustrate different toxicity profiles ET and RT. RT-related breast symptoms markedly improve by 15 months after completion of RT, while ET-associated side effects persist over the 5-year duration of ET therapy. The prospective CANTO trial studied 4262 BC patients (63% were post-menopausal). The study results note that in postmenopausal women, ET had a differentially worse and persistent effect on QoL at 2 years from diagnosis63.
The ET-associated cognitive decline with a negative impact on verbal learning/memory, visual learning/memory, frontal executive function, and processing speed is particularly of concern in an aging population64,65,66,67.
In summary, ET is associated with negative impact on QoL and high rates of poor tolerance of ET. The balance between benefit and risks of ET in women with low-risk BC is not well defined. There is compelling rationale for pursuing clinical trials in older women that will provide unequivocal evidence on the absolute therapeutic benefit of ET in low-risk BC, and help drive risk-tailored recommendations for adjuvant ET.
Role of comprehensive geriatric assessment (CGA)
In clinical trials and routine clinical practice, the importance of including CGA is being strongly promoted68,69,70,71,72. In the aging population, CGA is a helpful measure for stratifying individual risk, and may guide selection of therapeutic options according to biological age, functional status, intrinsic capacity, frailty, possible resilience, comorbidities, polypharmacy, and patient preferences. Alongside validated QoL assessments, prospective clinical trials should include CGA in study of older cancer patients. With such informed assessments, CGA may emerge as the one of the important determinants for establishing optimal adjuvant therapy in breast cancer.
Future directions and ongoing studies
To define risk-tailored treatment based on absolute clinical benefit by type of adjuvant therapy for early stage BC in older women requires modern prospective trials. The current NCCN guidelines and practice will not change without level 1 evidence demonstrating low, comparable event rates with improved QoL among older women with ER+ early BC treated with BCS + RT alone.
Two ongoing studies seeking to optimize the approach to adjuvant RT and ET in older women with early-stage BC are open and accruing patients in Italy and Canada. There are currently no trials in this patient population in the US (Table 5).
Exclusive Endocrine Therapy Or Partial Breast Irradiation for Women Aged ≥70 Years With Luminal A-like Early Stage Breast Cancer (EUROPA Trial—NCT04134598) study at the University of Florence opened to accrual since 2021 and plans to enroll 926 patients. Eligible patients have clinical low-risk hormone-sensitive BC, and randomization is between partial breast radiation (PBI) or ET alone. In comparing PBI to ET, the primary study endpoints include health-related QoL using the EORTC QLQ-C30, and non-inferior local recurrence rates. An interim analysis is planned when 152 enrolled patients reach the 2-year follow-up. Stopping rules include a >2% IBTR rate per year or a >7% DM rate at any time. Although this study will generate important evidence, history suggests that practice in the US is unlikely to change in the absence of a trial conducted in North America, given differences in co-morbidities, medical practice patterns, and patients’ values and preferences.
Evaluating Harms and Benefits of Endocrine Therapy in Patients ≥70 Years of Age with Lower Risk Breast Cancer (REaCT trial—NCT04921137), study sponsored by Ottawa Hospital Research Institute opened to enrollment in 2021. The study aims to evaluate the feasibility of ET omission in women ≥70 years treated with standard local therapy. The randomization is between no ET vs ET for 5 years. The study will enroll 100 patients with low-risk BC categorized by histopathologic features only. The primary outcomes include assessment of adverse events/toxicity and health-related QoL.
Conclusions
Women ≥70 years constitute a distinct group of BC patients with rising incidence of early stage BC amenable to BCS. The widely accepted standard of 1–3 week short-duration RT schedule is associated with less clinical and financial toxicity. Comprehensive local therapy (BCS + RT) is well tolerated, and beneficial in reducing risk of the most common site of BC relapse observed in older (≥70 years) women. Breast RT remains a relevant adjuvant option in our aging BC population.
Better understanding of the clinical–pathologic factors and MGAs have improved our ability to classify low-risk ER+, HER2-negative BC across all age groups. Older patients with favorable-risk BC treated with ET have very low rates of DR. As such, with the omission of ET, the up to 50% anticipated increased risk of DR in this population might remain low and clinically acceptable. To date, there is very little research aimed at defining age-specific recommendations for adjuvant ET in women ≥70 years.
To inform future practice guidelines for clinicians and patients, we advocate pursuing prospective trials to establish optimal age-adjusted, risk-tailored adjuvant therapy in older BC patient population, including systematic geriatric assessment, and the role of comprehensive local therapy alone with omission of ET as an alternative.
References
American Cancer Society. Cancer facts & figures 2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf (2021).
Henry, C., Ferlay, J., Boniol, M. & Autier, P. Changes in breast cancer incidence and mortality in middle-aged and elderly women in 28 countries with Caucasian majority populations. Ann. Oncol. 19, 1009–1018 (2008).
DeSantis, C. E. et al. Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J. Clin. 66, 31–42 (2016).
Howlader, N. et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER 2 status. J. Natl Cancer Inst. 106, dju055 (2014).
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378, 1701–1706 (2011).
Smith, B. D. et al. Radiation therapy for the whole breast: executive summary of an American Society for Radiation Oncology (ASTRO) evidence-based guideline. Pract. Radiat. Oncol. 8, 145–152 (2018).
Whelan, T. J. et al. Long-term results of hypofractionated radiation therapy for breast cancer. N. Engl. J. Med. 362, 513–520 (2010).
Coles, C. E. et al. IMPORT Trialists: partial-breast radiotherapy after breast conservation surgery for patients with early breast cancer (UK IMPORT LOW trial): 5-year results from a multicentre, randomised, controlled, phase 3, non-inferiority trial. Lancet 390, 1048–1060 (2017).
Vicini, F. A. et al. Long-term primary results of accelerated partial breast irradiation after breast-conserving surgery for early-stage breast cancer: a randomised, phase 3, equivalence trial. Lancet 394, 2155–2164 (2019).
Haviland, J. S. et al. The UK Standardisation of Breast Radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trials. Lancet Oncol. 14, 1086–1094 (2013).
Murray Brunt, A. et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5-year efficacy and late normal tissue effects results from a multicentre, non-inferiority, randomised, phase 3 trial. Lancet 395, 1613–1626 (2020).
Offeresen, B. V. et al. Hypofractionated versus standard fractionated radiotherapy in patients with early breast cancer or ductal carcinoma in situ in a randomized phase III trial: the DBCG HYPO trial. J. Clin. Oncol. 38, 3615–3625 (2020).
Correa, C. et al. Accelerated partial breast irradiation: executive summary for the update of an ASTRO Evidence-Based Consensus Statement. Pract. Radiat. Oncol. 7, 73–79 (2017).
Brunt, A. M. et al. Ten-year results of FAST: a randomized controlled trial of 5-fraction whole-breast radiotherapy for early breast cancer. J. Clin. Oncol. 38, 3261–3272 (2020).
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet 386, 1341–1352 (2015).
Early Breast Cancer Trialists’ Collaborative Group. Effects of adjuvant tamoxifen and of cytotoxic therapy on mortality in early breast cancer: an overview of 61 randomised trials among 28,896 women. N. Engl. J. Med. 319, 1681–1692 (1988).
Early Breast Cancer Trialists’ Collaborative Group. Tamoxifen for early breast cancer: an overview of the randomised trials. Lancet 351, 1451–1467 (1998).
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet 378, 771–784 (2011).
Burstein, H. J. et al. Adjuvant endocrine therapy for woman with hormone receptor positive breast cancer: ASCO clinical practice guideline focused update. J. Clin. Oncol. 37, 423–438 (2018).
Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365, 1687–1717 (2005).
Gradishar, W. J. et al. Breast cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J. Natl Compr. Cancer Netw. 20, 691–722 (2022).
Fisher, B. et al. A randomized clinical trial evaluating tamoxifen in the treatment of patients with node-negative breast cancer who have estrogen-receptor-positive tumors. N. Engl. J. Med. 320, 479–484 (1989).
Hughes, K. S. et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. J. Clin. Oncol. 31, 2382–2387 (2013).
Kunkler, I. H. et al. Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): a randomised controlled trial. Lancet Oncol. 1, 266–273 (2015).
Kunkler, I. et al. Breast-conserving surgery with or without irradiation in early breast cancer. N. Eng. J. Med. 388, 585–594 (2023).
Fyles, A. W. et al. Tamoxifen with or without breast irradiation in women 50 years of age or older with early breast cancer. N. Engl. J. Med. 351, 963–970 (2004).
Pötter, R. et al. Lumpectomy plus tamoxifen or anastrozole with or without whole breast irradiation in women with favorable early breast cancer. Int. J. Radiat. Oncol. Biol. Phys. 68, 334–340 (2007).
Fastner, G. et al. Endocrine therapy with or without whole breast irradiation in low-risk breast cancer patients after breast-conserving surgery: 10-year results of the Austrian Breast and Colorectal Cancer Study Group 8A trial. Eur. J. Cancer 127, 12–20 (2020).
Leach, C. R. et al. The complex health profile of long-term cancer survivors: prevalence and predictors of comorbid conditions. J. Cancer Surviv. 9, 239–251 (2015).
Paik, S. et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N. Engl. J. Med. 351, 2817–2826 (2004).
Sparano, J. A. et al. Clinical and genomic risk to guide the use of adjuvant therapy for breast cancer. N. Engl. J. Med. 380, 2395–2405 (2019).
Esserman, L. J. et al. Use of molecular tools to identify patients with indolent breast cancers with ultralow risk over 2 decades. JAMA Oncol. 3, 1503–1510 (2017).
Sparano, J. A. et al. Development and validation of a tool integrating the 21-gene recurrence score and clinical- pathological features to individualize prognosis and prediction of chemotherapy benefit in early breast cancer. J. Clin. Oncol. 39, 557–564 (2021).
Stemmer, S. et al. Clinical outcomes in patients with node-negative breast cancer treated based on the recurrence score results: evidence from a large prospectively designed registry. npj Breast Cancer 3, 33 (2017).
Shak, S. et al. Outcome disparities by age and 21-gene recurrence score result in hormone receptor positive breast cancer. Ann. Oncol. https://doi.org/10.1093/annonc/mdw364.03 (2016).
Petkov, V. et al. Breast-cancer-specific mortality in patients treated based on the 21-gene assay: a SEER population-based study. npj Breast Cancer 2, 16017 (2016).
Sparano, J. A. et al. Prospective validation of a 21-gene expression assay in breast cancer. N. Engl. J. Med. 373, 2005–2014 (2015).
Sparano, J. A. et al. Adjuvant Chemotherapy Guided by a 21-Gene Expression Assay in Breast Cancer. N. Eng. J. Med. 379, 111–121 (2018).
Lopes Cardozo, J. M. N. et al. Outcome of patients with an ultralow-risk 70-gene signature in the MINDACT Trial. J. Clin. Oncol. 40, 1335–1345 (2022).
Vliek, S. B. et al. Ten-year follow-up of the observational RASTER study, prospective evaluation of the 70-gene signature in ER-positive, HER 2-negative, node-negative early breast cancer. Eur. J. Cancer 175, 169–179 (2022).
Whelan, T. J. et al. LUMINA: a prospective trial omitting radiotherapy (RT) following breast conserving surgery (BCS) in T1N0 luminal A breast cancer (BC). J. Clin. Oncol. 40, LBA501 (2022).
The IDEA Study (Individualized Decisions for Endocrine Therapy Alone). NCT02400190.
The PRECISION Trial (Profiling Early Breast Cancer for Radiotherapy Omission): A Phase II Study of Breast-Conserving Surgery Without Adjuvant Radiotherapy for Favorable-Risk Breast Cancer. NCT02653755.
Kirwan, C. C., Coles, C. E., Bliss, J. & The PRIMETIME Protocol Working Group. It’s PRIMETIME. Postoperative avoidance of radiotherapy: biomarker selection of women at very low risk of local recurrence. Clin. Oncol. 28, 594–596 (2016).
EXamining PErsonalised Radiation Therapy for low-risk early breast cancer. EXPERT (BIG 16-02/ANZ 1601). NCT02889874.
Blamey, R. W. et al. Radiotherapy or tamoxifen after conserving surgery for breast cancers of excellent prognosis: British Association of Surgical Oncology (BASO) II trial. Eur. J. Cancer 49, 2294–2302 (2013).
Winzer, K. J. et al. Radiation therapy and tamoxifen after breast conserving surgery: updated results of a 22 randomised clinical trial in patients with low risk of recurrence. Eur. J. Cancer 46, 95–101 (2010).
Fisher, B. et al. Tamoxifen, radiation therapy, or both for prevention of ipsilateral breast tumor recurrence after lumpectomy in women with invasive breast cancers of one centimeter or less. J. Clin. Oncol. 20, 4141–4149 (2002).
Goldberg, M. et al. Patterns of adjuvant care and outcomes of elderly women with stage I breast cancer after breast-conserving surgery: a population-based analysis. Breast Cancer Res. Treat. 176, 657–667 (2019).
Yoon, T. I. et al. Age-related risk factors associated with primary contralateral breast cancer among younger women versus older women. Breast Cancer Res. Treat. 173, 657–665 (2019).
Chen, Y., Thompson, W., Semenciw, R. & Mao, Y. Epidemiology of contralateral breast cancer. Cancer Epidemiol. Biomark. Prev. 8, 855–8611 (1999).
Giannakeas, V., Lim, D. W. & Narod, S. A. The risk of contralateral breast cancer: a SEER-based analysis. Br. J. Cancer 125, 601–610 (2021).
Beckwée, D., Leysen, L., Meuwis, K. & Adriaenssens, N. Prevalence of aromatase inhibitor-induced arthralgia in breast 391 cancer: a systematic review and meta-analysis. Support Care Cancer https://doi.org/10.1007/s00520-017-3613-z (2017).
Amir, E., Seruga, B., Niraula, S., Carlsson, L. & Ocaña, A. Toxicity of adjuvant endocrine therapy in postmenopausal 389 breast cancer patients: a systematic review and meta-analysis. J. Natl Cancer Inst. https://doi.org/10.1093/jnci/djr242 (2011).
Yussof, I., Mohd Tahir, N. A., Hatah, E. & Mohamed Shah, N. Factors influencing five-year adherence to adjuvant 393 endocrine therapy in breast cancer patients: a systematic review. Breast 62, 22–35 (2022).
He, W. et al. Predictors of discontinuation of adjuvant hormone therapy in patients with breast cancer. J. Clin. Oncol. 33, 2262–2269 (2015).
Salgado, B. A. & Zivian, M. T. and CINAHL for studies that measured rates and/or correlates of adherence and/or persistence to adjuvant hormonal therapy. Breast Cancer Res. Treat. 45, 431–439 (2007).
Hershman, D. L. et al. Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8,769 early-stage breast cancer patients. J. Clin. Oncol. 28, 4120–4128 (2010).
Sheppard, V. B. et al. Frailty and adherence to adjuvant hormonal therapy in older women with breast cancer: CALGB protocol 369901. J. Clin. Oncol. 32, 2318–2327 (2014).
Murphy, C. C., Bartholomew, L. K., Carpentier, M. Y., Bluethmann, S. M. & Vernon, S. W. Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic review. Breast Cancer Res. Treat. 134, 459–478 (2012).
Crivellari, D. et al. Hormone therapy in elderly breast cancer 396 patients with comorbidities. Crit. Rev. Oncol. Hematol. 73, 92–98 (2010).
Williams, L. J., Kunkler, I. H., King, C. C., Jack, W. & van der Pol, M. A randomised controlled trial of post-operative radiotherapy following breast-conserving surgery in a minimum-risk population: quality of life at 5 years in the PRIME trial. Health Technol. Assess. 15, 1–57 (2011).
Ferreira, A. R. et al. Differential impact of endocrine therapy and chemotherapy on quality of life of breast cancer survivors: a prospective patient-reported outcomes analysis. Ann. Oncol. 30, 1784–1795 (2019).
Mandelblatt, J. S. et al. Cancer-related cognitive outcomes among older breast cancer survivors in the Thinking and Living with Cancer Study. J. Clin. Oncol. 36, 3211–3222 (2018).
Wagner, L. I., Sweet, J. J., Butt, Z., Lai, J. S. & Cella, D. Measuring patient self-reported cognitive function: development of the functional assessment of cancer therapy–cognitive function instrument. J. Support Oncol. 7, 32–39 (2009).
Wagner, L. et al. Patient-reported cognitive impairment among women with early breast cancer randomly assigned to endocrine therapy alone versus chemoendocrine therapy: results from TAILORx. J. Clin. Oncol. 38, 1875–1886 (2020).
Underwood, E. A. et al. Cognitive sequelae of endocrine therapy in women treated for breast cancer: a meta-analysis. Breast Cancer Res. Treat. 168, 299–310 (2018).
Loh, K. P. et al. What every oncologist should know about geriatric assessment for older patients with cancer: Young International Society of Geriatric Oncology Position Paper. J. Oncol. Pract. 14, 85–94 (2018).
Wildiers, H. et al. International Society of Geriatric Oncology consensus on geriatric assessments in older patients with cancer. J. Clin. Oncol. 32, 2595–2603 (2014).
Dotan, E. et al. NCCN Guidelines® Insights: Older Adult Oncology, Version 1. J. Natl Compr. Cancer Netw. 19, 1006–1019 (2021).
Abbasi, J. Older patients (still) left out of cancer clinical trials. JAMA 322, 1751–1753 (2019).
Williams, N. et al. Feasibility of comprehensive geriatric assessment in an academic breast oncology clinic. Cancer Res. 80, P4-16-01 (2020).
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the writing of this review and in providing in-depth understanding and critique of the literature on this topic.
Corresponding author
Ethics declarations
Competing interests
S.S.: Honoraria for consulting/advisory boards in the past 2 years: AstraZeneca, Daiichi-Sankyo, Natera, Biotheranostics, Molecular Templates, Sanofi; non-promotional speaking: Genentech/Roche; research funding to institution: Genentech/Roche, Kailos Genetics; third party in kind writing: AstraZeneca and Genentech/Roche; travel in kind: Genentech/Roche, Daiichi Sankyo, Sanofi; SEAGEN Board of Directors with stock, stipend, and travel; Napo Pharmaceuticals Scientific Advisory Board: stipend and travel; American Society of Clinical Oncology Conquer Cancer Foundation Board of Directors, unpaid; National Surgical Breast and Bowel Project Foundation Board of Directors, unpaid; R.J.: Effort on this work was supported by a Senior Scholar Grant from the Susan G. Komen Foundation. Unrelated to the current work, R.J. has stock options as compensation for her advisory board role in Equity Quotient, a company that evaluates culture in health care companies; she has received personal fees from the Greenwall Foundation, Doris Duke Charitable Foundation, and the National Institutes of Health and grants or contracts for unrelated work from the National Institutes of Health, the Doris Duke Charitable Foundation, and the American Cancer Society. She has served as an expert witness for Dressman Benzinger LaVelle and Kleinbard, LLC. T.W.: Exact sciences—non-direct financial support for biomarker testing for ongoing studies unrelated to this work. J.A.S.: Associate Editor of npj Breast Cancer. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chadha, M., White, J., Swain, S.M. et al. Optimal adjuvant therapy in older (≥70 years of age) women with low-risk early-stage breast cancer. npj Breast Cancer 9, 99 (2023). https://doi.org/10.1038/s41523-023-00591-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41523-023-00591-6