Abstract
These analyses explore the impact of homologous recombination repair gene mutations, including BRCA1/2 mutations and homologous recombination deficiency (HRD), on the efficacy of the poly(ADP-ribose) polymerase (PARP) inhibitor talazoparib in the open-label, two-cohort, Phase 2 ABRAZO trial in germline BRCA1/2-mutation carriers. In the evaluable intent-to-treat population (N = 60), 58 (97%) patients harbor ≥1 BRCA1/2 mutation(s) in tumor sequencing, with 95% (53/56) concordance between germline and tumor mutations, and 85% (40/47) of evaluable patients have BRCA locus loss of heterozygosity indicating HRD. The most prevalent non-BRCA tumor mutations are TP53 in patients with BRCA1 mutations and PIK3CA in patients with BRCA2 mutations. BRCA1- or BRCA2-mutated tumors show comparable clinical benefit within cohorts. While low patient numbers preclude correlations between HRD and efficacy, germline BRCA1/2 mutation detection from tumor-only sequencing shows high sensitivity and non-BRCA genetic/genomic events do not appear to influence talazoparib sensitivity in the ABRAZO trial.
ClinicalTrials.gov identifier: NCT02034916.
Similar content being viewed by others
Introduction
The tumor suppressors breast cancer susceptibility genes BRCA1 and BRCA2 are critical to the repair of double-strand breaks in DNA via homologous recombination repair (HRR). During tumorigenesis, loss of the BRCA wildtype alleles leads to the use of other repair pathways, notably those involving poly(ADP-ribose) polymerase (PARP) 1 and 21,2. PARP inhibition in BRCA-mutated cells that have deficient HRR results in cell death due to synthetic lethality1,3. Investigations have also introduced the concept of “BRCAness” where constitutional methylation of the BRCA1 promoter4 or deficiencies in other HRR proteins, aside from BRCA1/2, render cells sensitive to PARP inhibitors (PARPi)3,5,6,7.
This initial model explaining PARPi efficacy based on synthetic lethality alone was modified when preclinical data showed that some PARPi trapped PARP1 on DNA in addition to PARP1 catalytic inhibition8,9. It is hypothesized that trapped PARP may impede replication fork machinery directly10 or prevent replication fork progression, resulting in damaged DNA that cannot be repaired by cells with defective HRR mechanisms1. Studies have shown that the degree of trapping varies between different PARPi, with talazoparib displaying the greatest potency1,9,11.
Clinical trials have demonstrated the efficacy of talazoparib in breast cancers with germline BRCA1/2 mutations (gBRCA1/2mut)12,13. ABRAZO (NCT02034916) was a two-cohort, Phase 2 study of talazoparib in gBRCA1/2mut carriers with a response to prior platinum with no progression on or ≤8 weeks of the last platinum dose (Cohort 1), or ≥3 platinum-free cytotoxic regimens (Cohort 2) for advanced breast cancer. Here, talazoparib demonstrated a confirmed objective response rate (ORR) of 20.8% (95% confidence interval [CI] 10.47–34.99) and 37.1% (95% CI 21.47–55.08) in Cohorts 1 and 2, respectively12,14. Investigator-assessed median progression-free survival (PFS) was 4.0 months (95% CI 2.8–5.4) in Cohort 1 and 5.6 months (95% CI 5.5–7.8) in Cohort 2. An exploratory subgroup analysis suggested that a longer platinum-free interval following the last dose of platinum therapy was associated with greater clinical activity12.
Mutations in genes involved in HRR are associated with better outcomes after PARPi therapy in prostate cancer15, but it is unclear which tumor genetic or genomic factors might influence PARPi response in patients with human epidermal growth factor receptor 2-negative (HER2−), gBRCA1/2mut locally advanced or metastatic breast cancer (MBC). Despite studies suggesting that the inactivation or deletion of a single BRCA1/2 allele, resulting in haploinsufficiency, can be enough to promote tumorigenesis16,17, patients with gBRCA1/2mut tumors frequently exhibit tumoral loss of non-mutated (wildtype) allele at the BRCA1 or BRCA2 locus, known as locus-specific loss of heterozygosity (LOH)16,17,18. Indeed, the presence of LOH has been shown to be associated with high sensitivity to PARPi16,18.
The goal of these analyses was to assess tumor tissue from patients enrolled in ABRAZO, with a focus on BRCA1/2mut, including germline-tumor concordance and zygosity; other genes implicated in homologous recombination DNA damage repair (DDR); other commonly mutated non-DDR genes; homologous recombination deficiency (HRD), assessed using genome-wide LOH (gLOH); and to explore potential correlations of the above with efficacy outcomes. Here, 97% of patients have ≥1 BRCA1/2 mutation with 95% concordance between germline and tumor mutations. The most prevalent non-BRCA tumor mutations are TP53 and PIK3CA. BRCA LOH is evident in 85% of tBRCAmut patients evaluable for BRCA zygosity and 81.6% of patients have gLOH ≥16% across both cohorts. Overall, BRCA1- or BRCA2-mutated tumors show comparable clinical benefit within cohorts while non-BRCA genetic/genomic events do not appear to influence talazoparib sensitivity.
Results
Patients
A total of 84 patients enrolled between May 2014 and February 2016 comprised the intent-to-treat (ITT) population of the ABRAZO trial12. The median follow-up time was 13.7 months for each cohort12. Baseline characteristics are shown in Table 1. Tumor tissue was evaluable for sequencing from 60/84 patients (71%) with a similar number of evaluable patients in both cohorts (Table 1, Fig. 1, Supplementary Fig. 1)19.
1Known/likely pathogenic variants per FoundationOne® CDx test are shown (genes altered in >1 patient are plotted). Those patients with multiple alterations in a gene are indicated by (■) and if one of the alterations is LOH, the square is colored as LOH. For rearrangements, if a partner gene was present, both genes were labeled. CN copy number, LOH loss of heterozygosity, NA not available, RE rearrangement, SV short variant.
Prevalence and types of BRCA1/2 mutations found in tumors
Of 60 evaluable patients, 58 (97%) exhibited ≥1 BRCA1 or BRCA2 pathogenic tumor mutation (tBRCA1/2mut); no patients had both BRCA1 and BRCA2 mutations (Table 2, Fig. 1). The two patients without a tBRCA1/2mut had BRCA2 variants of unknown pathogenic significance distinct from their gBRCA2mut (Table 2, Supplementary Table 1 [patients 30 and 36]). The landscape of tumor genetic alterations in ABRAZO based on testing with FoundationOne® CDx is shown in Fig. 1. The distribution of BRCA mutations was not uniform, with BRCA1 mutations more commonly observed in Cohort 1 than Cohort 2. Conversely, BRCA2 mutations were more prevalent in Cohort 2 than Cohort 1 (Table 2, Fig. 1). Across both cohorts, the most common tumor BRCA1/2 variant types detected were single nucleotide variants (BRCA1: 15/60, 25.0%; BRCA2: 11/60, 18.3%), deletions (BRCA1: 11/60, 18.3%; BRCA2: 12/60, 20.0%), and insertions (BRCA1: 4/60, 6.7%; BRCA2: 6/60, 10.0%), with a tumor BRCA1 copy number alteration (CNA) only evident in 1/60 patients (Supplementary Table 1 [patient 16]).
Concordance between gBRCA1/2 and tBRCA1/2 mutational status was evaluated in 56 patients in the ITT population who were analyzed using the BRACAnalysis CDx® assay and had tumor tissue evaluable using FoundationOne® CDx. Here, 53 patients (95%) exhibited concordance in mutations, i.e., same mutation detected in germline also found in tumor, and 54 patients (96%) exhibited concordance in mutational status, i.e., same BRCA gene mutated in germline also mutated in tumor (Fig. 2).
1The proportion of patients with a known gBRCA1mut based on the BRACAnalysis CDx® assay (Myriad Genetics) who have a BRCA1 mutation detected in tumor using FoundationOne® CDx is shown, and similarly for BRCA2. All patients showing concordant BRCA1 or BRCA2 mutational status exhibited the same mutation in tumor as originally detected in germline, as evidenced by mapping to a common Variation ID in ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/) or other comparative means. An additional patient was included as concordant (mapped to REARR) as their pathogenic tBRCA1 CNA was deemed to align with a gBRCA1 deletion of exons 13–15. Of the three non-concordant patients, one patient exhibited a gBRCA2 SNV that was not detected in the tumor, which exhibited a different BRCA2 SNV of unknown pathogenicity; the second patient exhibited a gBRCA2 duplication of exons 15–18, which was not detected in the tumor, and a tBRCA2 SNV of unknown pathogenicity (this patient was mapped to REARR category); and the third patient exhibited a gBRCA1 rearrangement (del exon 16), which was not detected in the tumor, and a tBRCA1 splice site mutation (this patient was mapped to REARR category). BRCA1/2 breast cancer susceptibility gene 1 or 2, DEL deletion, gBRCA1/2mut germline BRCA1/2 mutation, INS insertion, REARR rearrangement, SNV single nucleotide variant, tBRCA tumor BRCA.
BRCA LOH, with retention of a mutant BRCA allele, was predicted in 40/47 (85%) tBRCA1/2mut patients evaluable for BRCA zygosity (Table 2, Fig. 1). Of these 40 patients, 37 exhibited tumor retention of a known gBRCAmut. Of the remaining three of 40 patients, one (patient 60) exhibited BRCA LOH with tumor retention of a presumed somatic (i.e., not detected in germline testing) BRCA1 mutation, with a different known gBRCAmut predicted to be in a heterozygous state in the tumor; gBRCAmut details were not available for the other two patients (patients 21 and 37) (Supplementary Table 1).
Prevalence of non-BRCA1/2 tumor mutations
TP53 and PIK3CA were the most prevalent non-BRCA tumor mutations. In both cohorts, TP53 mutations were more prevalent with BRCA1mut than BRCA2mut; this trend was particularly evident in Cohort 1 (comprising patients with a prior platinum response; Table 3). In both cohorts, PIK3CA mutations were more prevalent in BRCA2mut tumors versus tumors harboring BRCA1mut (Table 3), with differences in mutation incidence reflecting tumor subtype differences: 5/6 patients with PIK3CA mutations had tBRCA2mut hormone-receptor positive (HR+) disease, while the remaining patient had tBRCA1mut triple-negative breast cancer (TNBC) (data not shown).
When analysis was confined to CNAs in the ABRAZO population, RAD21 and MYC were the most frequently altered non-BRCA genes in BRCA-mutated tumors (only amplification events detected; see Fig. 1). Furthermore, CNAs of RAD21 and MYC were more commonly observed in tumors from Cohort 2 than in Cohort 1 (Table 3).
Genomic LOH
In the evaluable ITT population, the median (range) gLOH score was 21.3% (9.1–41.8) and 23.4% (0.0–38.9) for Cohorts 1 and 2, respectively. Across both cohorts, 81.6% (31/38) of patients had gLOH ≥16% (exploratory threshold for high gLOH)20, with similar results observed in Cohort 1 (85.0% [17/20 patients]) and Cohort 2 (77.8% [14/18 patients]) separately. Of the seven evaluable patients with gLOH <16% (patients 8, 34, 49, 51, 55, 66, and 71), five had BRCA LOH, one did not exhibit BRCA LOH, and one was not evaluable for BRCA LOH (Supplementary Table 1).
Of 34 patients from combined Cohorts 1 and 2 who were evaluable for both gLOH and BRCA LOH status, only three lacked BRCA LOH (Supplementary Table 1 [patients 51, 60, 67]), precluding assessment of the relationship between gLOH and BRCA LOH in this study.
Clinical benefit and tumor mutational profile
In Cohort 1, the clinical benefit rate at 24 weeks (CBR24) was 24% (4/17; 95% CI 7–52) and 25% (3/12; 95% CI 5–57) for tBRCA1mut and tBRCA2mut, respectively. In Cohort 2, the CBR24 was 67% (8/12; 95% CI 35–90) and 63% (10/16; 95% CI 35–85) for tBRCA1mut and tBRCA2mut, respectively. A range of clinical outcomes were reported in tBRCAmut patients lacking BRCA LOH (n = 2 in Cohort 1; n = 5 in Cohort 2); although only two patients achieved a partial response, three had stable disease, and PFS ranged from 1.35–30.29 months (Supplementary Table 1). The low number of tBRCAmut patients without BRCA LOH (n = 7) precluded efficacy comparisons between tBRCAmut patients exhibiting or not exhibiting BRCA LOH.
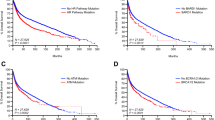
A significant association was observed between the number of DDR alterations (two vs one) and best response to talazoparib in Cohort 2, with single mutations being associated with higher responsiveness (Fig. 3; odds ratio [OR] 0.08, 95% CI 0.01–0.83, p = 0.03). However, analysis of Cohort 1 did not show such an association (Fig. 3; OR 0.85, 95% CI 0.08–9.44, p = 1). In addition, there was no significant association between the number of DDR alterations (two vs one) and CBR24 in Cohort 1 or 2 (OR 1.7, 95% CI 0.24–12.17, p = 0.62, and OR 0.36, 95% CI 0.06–2.00, p = 0.37, respectively). The presence of non-BRCA DDR mutations did not appear to enhance talazoparib sensitivity in this BRCA-mutant setting (Fig. 3).
1Based on evaluable ITT population with measurable disease. Number of DDR alterations is sum of known and likely pathogenic variants in the following genes, excluding copy number alterations: BRCA1, BRCA2, CHEK2, ARID1A, ATR, BARD1, BRD4, BRIP1, FANCC, STAG2. BRCA1/2 breast cancer susceptibility gene 1 or 2, CR complete response, DDR DNA damage response, DDRalt DNA damage response alteration, ITT intent-to-treat, NE non-evaluable, PD progressive disease, PR partial response, SD stable disease.
In the analysis exploring the impact of common non-DDR alterations on PFS, no associations were evident between the alteration status of TP53 or RAD21, and PFS in Cohort 1 or 2 (Table 4).
Discussion
In these analyses of tumor tissue from patients enrolled in the open-label, Phase 2 ABRAZO study, 97% of evaluable tumors exhibited ≥1 BRCA1/2mut and there was 95% concordance between known gBRCA1/2mut and tBRCA1/2mut; this is perhaps unsurprising given the importance of gBRCAmut in breast cancer pathology, and the fact that patients were selected based on gBRCAmut status.
BRCA LOH was evident in 85% of tBRCAmut patients evaluable for BRCA zygosity. This high prevalence of LOH for BRCA1/2mut is consistent with previous studies in breast cancer where loss of the wildtype chromosome was seen in 88–89% of BRCA1/2mut patients18,21. Sequencing of another set of gBRCA1/2mut breast tumors also showed high incidence of locus-specific LOH for BRCA1 (90%); however, lower LOH incidence (54%) was observed for BRCA2. In that dataset, LOH for BRCA1 was more commonly copy neutral and loss of the wildtype allele more frequent in gBRCA2mut tumors16. In a larger patient cohort containing pan-cancer germline pathogenic BRCA1/2 carriers, 86% of zygosity changes targeted loss of the remaining wildtype allele22. This is consistent with a positive selective pressure for bi-allelic inactivation of BRCA1/222. Of note, there are mechanisms of silencing the wildtype BRCA allele other than BRCA LOH, such as BRCA1 promoter methylation; hence, absence of BRCA LOH does not necessarily correspond to partial retention of wildtype BRCA function16,21,23. Studies have also suggested that a haploinsufficiency phenotype in gBRCA2mut cells results in reduced functional BRCA2 protein levels, which could contribute toward chromosomal instability and subsequent promotion of tumorogenesis24,25.
BRCA1/2 alterations are most frequently bi-allelic in tumor types that have demonstrated clinical sensitivity to PARPi monotherapy, including ovarian, breast, prostate, and pancreatic cancer18,22. Bi-allelic BRCA1/2 inactivating mutations are also associated with Signature 3, a pattern of genome-wide mutations linked to HRD in breast cancer23. However, the low fraction of tumors without BRCA LOH in this study precluded the assessment of impact of zygosity on outcome.
DDR gene alteration burden or alteration status of selected non-BRCA genes was not generally associated with clinical efficacy in this study, as assessed by best percent change of sum of longest diameters of target lesions from baseline over time, or PFS, respectively. Moreover, the presence of additional non-BRCA DDR mutations was not associated with enhanced talazoparib efficacy. Tumor HRD (as assessed by gLOH) was variable, but high, in ABRAZO. However, low patient numbers precluded correlations with efficacy.
Previously, gLOH has been used to determine deficiency in homologous recombination in tumor samples26 and higher scores have been associated with better therapeutic response26,27. gLOH scores were on average relatively high in ABRAZO and similar to those found in HER2– gBRCA1/2mut breast cancer (median 23.0%, based on N = 1730 tumors; 27.8% for gBRCA1mut and 21.0% for gBRCA2mut) from Foundation Medicine’s FoundationCore® database. Moreover, these scores are much greater than those seen for the overall breast cancer population (median 12.2%, based on N = 20,614 tumors), reflecting HRR deficiency associated with gBRCA1/2mut. In addition, ABRAZO patients exhibited a relatively high observed fraction of gLOH-high tumors (≥16% gLOH score20), which was also similar to that reported in HER2– gBRCA1/2mut breast cancer (78.1%; 82.3% for gBRCA1mut and 74.9% for gBRCA2mut) and over two-fold higher than that observed in the overall breast cancer population (35.3%) in the Foundation Medicine database. The association of gBRCAmut status with elevated gLOH was also evident within both HER2– and TNBC disease subtypes in the Foundation Medicine database (Supplementary Fig. 2).
Breast tumors often display distinct mutational profiles and gene rearrangement signatures that are associated with BRCAmut21. TP53 and PIK3CA are among the most frequently mutated genes in HR+/HER2− breast cancer28. In the Foundation Medicine database, TP53 mutations were evident in 86.2% (225/261) and 30.1% (96/319) of gBRCA1mut and gBRCA2mut tumors, respectively (Q = 1.38E–44), after Benjamini-Hochberg correction for multiple comparisons. In another dataset of pan-disease BRCA1/2-mutated cancers, TP53 mutations were the most common genomic alterations overall (67%) and were most prevalent in gBRCA1mut carriers29. Furthermore, breast and ovarian tumors with gBRCA1/2mut are more likely to have TP53 mutations if they display BRCA LOH16. The strong correlation between BRCA mutations and TP53 mutations reflects a common association with TNBC30,31. Similarly, in the ABRAZO population, TP53 mutations were more prevalent in BRCA1mut than BRCA2mut tumors. Somatic loss of both BRCA1 and TP53 has been recapitulated in animal models and results in rapid formation of highly proliferative, poorly differentiated, estrogen receptor-negative mammary carcinomas32, suggesting a role for TP53 mutations in this setting. Furthermore, studies have shown that p53 interacts with BRCA1 and regulates the ability of BRCA1 to respond to DNA damage, suggesting that wildtype BRCA1 can be rendered dysfunctional in a mutated TP53 background33,34.
In the Foundation Medicine database, PIK3CA mutations were evident in 8.4% (22/261) and 13.2% (42/319) of gBRCA1mut and gBRCA2mut tumors, respectively (Q = 0.08). Similarly, in the ABRAZO population, a numerically higher prevalence of PIK3CA mutations was associated with BRCA2mut tumors, particularly BRCA2mut HR+ tumors. These findings reflect previous studies which demonstrate that PIK3CA mutations are frequently found in HR+/HER2− breast cancer35. In a group of patients with hereditary breast cancer, PIK3CA mutations were associated with BRCA2 but not BRCA1 mutations, and with luminal-type breast cancer36.
Here, several other non-BRCA gene mutations were detected in tumors including CHEK2, ARID1A, ATR, BARD1, BRD4, BRIP1, FANCC, and STAG2. Mutations in ARID1A, a subunit of the SWI/SNF chromatin remodeling complex, represent the most frequent alteration of the SWI/SNF complex in estrogen receptor-positive breast cancer, and ARID1A has been suggested to play a major role in breast luminal lineage fidelity and endocrine therapy sensitivity37.
The clinical benefit of talazoparib in the ABRAZO population was comparable between cohorts for patients with BRCA1mut or BRCA2mut tumors. Despite only representing ~15% of evaluable patients in the ABRAZO population, there was also potential for clinical benefit of talazoparib in tBRCA1/2mut patients lacking BRCA LOH. DDR deficiencies elicited by mutations, for example, in BRCA1/2, are associated with a high mutational burden or genomic instability with worse clinical outcomes across almost all cancer types38. Here, a significant association was observed between the number of DDR alterations and best response to talazoparib in Cohort 2. However, there was no significant association between the number of DDR gene alterations and CBR24. Of note, the presence of non-BRCA1/2 DDR mutations did not appear to enhance sensitivity to talazoparib in patients with BRCA1/2mut; this finding was expected given that patients were enrolled based on gBRCAmut status and the importance of gBRCAmut in tumor pathobiology in such patients, potentially suggesting that the observation in Cohort 2 was a chance finding. Furthermore, no associations were evident between the alteration status of TP53 and RAD21, and PFS in Cohorts 1 or 2.
Limitations of the ABRAZO study have previously been discussed and include the termination of enrollment prior to completion, resulting in a low number of evaluable patients in each cohort12. This was due to overlapping enrollment criteria with the Phase 3 EMBRACA trial (NCT01945775)39 following a protocol amendment to EMBRACA12. Early termination also precluded further stratification by BRCA1/2mut and breast cancer subtypes. Furthermore, DNA sequencing may fail to find functional non-genetic deficiencies in DDR genes (e.g., promoter methylation). Finally, the primary/metastatic origin of archival tissue was not determined for this study. To address some of these limitations, similar analyses have been performed for tumor tissue from the Phase 3 EMBRACA study40. Whole genome sequencing/next-generation sequencing (NGS) analyses of paired biopsies from ABRAZO and EMBRACA are also pending to address acquired resistance mechanisms.
In this genomic analysis of the ABRAZO trial, we demonstrate that tumor-only BRCA1/2 sequencing has high sensitivity for gBRCA1/2mut. We report the genomic profile of BRCA1/2-related breast cancer, and provide evidence that non-BRCA genetic/genomic events did not appear to impact the efficacy of talazoparib. These findings are consistent with those recently published for the Phase 3 EMBRACA (talazoparib) and OlympiAD (olaparib) studies40,41. As both germline and somatic mutations may be identified by tumor sequencing, further research is required to assess whether tumor-only sequencing can direct talazoparib therapy.
Methods
Study design and patients
ABRAZO was an open-label, two-cohort, Phase 2 study of talazoparib (1 mg, orally once daily) in patients with MBC with a deleterious or a suspected deleterious gBRCA1/2mut12. Briefly, the study comprised two cohorts: Cohort 1 included patients who had a complete response or partial response to a previous platinum-containing regimen for metastatic disease, and no disease progression within 8 weeks of the last dose of platinum therapy; Cohort 2 included patients who had received ≥3 previous cytotoxic chemotherapy regimens for metastatic disease and no previous platinum therapy for metastatic disease. Patients with HER2-positive disease were eligible for either cohort, provided they were considered refractory to HER2-targeted therapy12. The primary and secondary endpoints were ORR and CBR24, respectively. The protocol was approved by the appropriate Institutional Review Board or local ethics committee at each participating institution and written informed patient consent was obtained12. The following independent ethics committees or Institutional Review Boards provided study approval: Comité de Protection des Personnes Sud-Ouest et Outre Mer III, Bordeaux, France; Ethik-Kommission der Medi, Fakultät der Ludwig-Maximilians- Universität (LMU) München – Fachbereich Medizin, München, Germany; Comité Éticos de Investigación Clínica, Hospital Universitario Ramón y Cajal, Madrid, Spain; NRES Committee London - City and East, Bristol Research Ethics Committee Centre, Bristol, UK; Office of the Human Research Protection Program, Los Angeles, CA, USA; Johns Hopkins Medicine Institutional Review Board, Baltimore, MD, USA; The Committee on Human Research, University of California, San Francisco, CA, USA; Western Institutional Review Board, Puyallup, WA, USA; Penn State College of Medicine Institutional Review Board, Hershey, PA, USA; University of Texas MD Anderson Cancer Center Institutional Review Board, Houston, TX, USA; University of Miami Institutional Review Board, Miami, FL, USA; University of Tennessee Graduate School of Medicine Institutional Review Board, Knoxville, TN, USA; Spectrum Health Institutional Review Board, Grand Rapids, MI, USA; Administrative Panels on Human Subjects in Medical Research, Stanford University, Palo Alto, CA, USA; and the Memorial Sloan Kettering Cancer Center Institutional Review Board, New York, NY, USA. The ethics committees were properly constituted and compliant with all requirements and local regulations. The study was conducted in accordance with the protocol, good clinical practice standards, the Declaration of Helsinki, and the International Conference on Harmonization.
Next-generation sequencing and mutational analysis
In the majority of patients, gBRCA1/2mut were determined using the BRACAnalysis CDx® assay (Myriad Genetics Inc., Salt Lake City, UT, USA). Enrollment of five patients was supported by local BRCA1/2 testing12. Archival or de novo tumor tissue (formalin-fixed, paraffin-embedded tissue; primary/metastatic sites) was sequenced using the FoundationOne® CDx NGS panel (Foundation Medicine, Inc., Cambridge, MA, USA), including mutations in BRCA1/2 and non-BRCA genes involved in DDR. For the purposes of this analysis, tumor mutations were defined as known or likely pathogenic variants per the FoundationOne® CDx test with CNAs excluded.
The influence of tumor BRCA1/2 mutational zygosity on PFS was explored by comparing patients with and without BRCA1/2 LOH. gLOH and somatic-germline-zygosity (SGZ) assessments were performed by Foundation Medicine Inc. using the Foundation Core Build 2019Q142,43.
DNA was extracted and adaptor ligated hybridization capture for all coding exons of 310 genes plus 34 introns frequently rearranged in cancer was performed. Libraries were sequenced to a median unique coverage depth of >500X. Analysis for genomic alterations, including short variant alterations (base substitutions, insertions, and deletions), copy number alterations (amplifications and homozygous deletions), as well as gene rearrangements was performed as previously described44.
To assess tumor and germline concordance, mutations were mapped to a common Variation ID in ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/) or other comparative means. In addition, non-BRCA DDR genes (CHEK2, ARID1A, ATR, BARD1, BRD4, BRIP1, FANCC, STAG2) were selected for inclusion in correlative analyses on the basis of involvement in homologous recombination-mediated DNA repair and/or demonstrated potential for mutations to sensitize to PARP inhibitors in nonclinical models45,46,47,48, coupled with presence of known or likely pathogenic variants (excluding CNAs) of these genes in this dataset.
Foundation Medicine clinical database
The Foundation Medicine clinical database comprises patient cases that underwent genomic profiling as a routine part of clinical care using a targeted comprehensive genomic profiling assay in a Clinical Laboratory Improvement Amendments (CLIA)-certified, College of American Pathologists (CAP)-accredited, New York State-approved laboratory (FoundationOne® CDx, Cambridge, MA, USA). Database version Foundation Core Build 2019Q1 was used in this study.
Endpoint definitions in ABRAZO
ORR was defined as the proportion of patients in the tumor-evaluable population who had a confirmed objective response (best overall response of complete or partial response) assessed by the independent radiology facility using Response Evaluation Criteria In Solid Tumors (RECIST) version 1.1 at the time of data cutoff. CBR24 was defined as complete response, partial response, or stable disease ≥24 weeks per RECIST version 1.1 by investigator assessment.
Statistical analysis
The influence of tumor BRCA1/2 mutational zygosity on PFS was analyzed by comparison of patients with and without BRCA1/2 LOH using the Cox proportional hazards model and a log-rank two-sided test to compare between altered/unaltered groups. Logistic regression was used to determine the odds ratio, 95% CI, and p value for the effect of two versus one DDR mutations on PFS.
The Mann–Whitney U test was used for comparison of gLOH values between germline BRCA wildtype and germline BRCA-mutated tumors in patients with HER2– and TNBC and Fisher’s exact test was used to determine the odds ratio and p value for comparison of the percentage of samples with gLOH ≥16% between the two groups. No corrections were made for multiple comparisons due to the low patient numbers and exploratory nature of this research, and as this study is primarily intended for hypothesis-generation.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
This study presents a secondary analysis of data from the ABRAZO trial12 and Pfizer does not have access to the primary sequencing files. Upon request, and subject to review, Pfizer will provide the clinical data that support the findings of this study. Subject to certain criteria, conditions and exceptions, Pfizer may also provide access to the related individual anonymized participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
References
Lord, C. J. & Ashworth, A. PARP inhibitors: synthetic lethality in the clinic. Science 355, 1152–1158 (2017).
Javle, M. & Curtin, N. J. The potential for poly (ADP-ribose) polymerase inhibitors in cancer therapy. Ther. Adv. Med Oncol. 3, 257–267 (2011).
McCabe, N. et al. Deficiency in the repair of DNA damage by homologous recombination and sensitivity to poly(ADP-ribose) polymerase inhibition. Cancer Res. 66, 8109–8115 (2006).
Wong, E. M. et al. Constitutional methylation of the BRCA1 promoter is specifically associated with BRCA1 mutation-associated pathology in early-onset breast cancer. Cancer Prev. Res. (Phila.) 4, 23–33 (2011).
Turner, N., Tutt, A. & Ashworth, A. Hallmarks of ‘BRCAness’ in sporadic cancers. Nat. Rev. Cancer. 4, 814–819 (2004).
Sharma, P. et al. Results of a phase II randomized trial of cisplatin +/− veliparib in metastatic triple-negative breast cancer (TNBC) and/or germline BRCA-associated breast cancer (SWOG S1416). J. Clin. Oncol. 38, 1001–1001 (2020).
van der Wijngaart, H. et al. Olaparib monotherapy in pretreated patients with BRCA1/2 alterations: results of a DRUP trial cohort. J. Clin. Oncol. 38, 3633 (2020).
Ashworth, A. & Lord, C. J. Synthetic lethal therapies for cancer: what’s next after PARP inhibitors? Nat. Rev. Clin. Oncol. 15, 564–576 (2018).
Murai, J. et al. Stereospecific PARP trapping by BMN 673 and comparison with olaparib and rucaparib. Mol. Cancer Ther. 13, 433–443 (2014).
Xie, S. et al. Timeless interacts with PARP-1 to promote homologous recombination repair. Mol. Cell. 60, 163–176 (2015).
Zandarashvili, L. et al. Structural basis for allosteric PARP-1 retention on DNA breaks. Science 368, eaax6367 (2020).
Turner, N. C. et al. A phase II study of talazoparib after platinum or cytotoxic nonplatinum regimens in patients with advanced breast cancer and germline BRCA1/2 mutations (ABRAZO). Clin. Cancer Res. 25, 2717–2724 (2019).
de Bono, J. et al. Phase I, dose-escalation, two-part trial of the PARP inhibitor talazoparib in patients with advanced germline BRCA1/2 mutations and selected sporadic cancers. Cancer Discov. 7, 620–629 (2017).
ClinicalTrials.gov. A. Phase 2, 2-Stage, 2-Cohort Study of Talazoparib (BMN 673), in Locally Advanced and/or Metastatic Breast Cancer Patients With BRCA Mutation (ABRAZO Study) (ABRAZO), https://clinicaltrials.gov/ct2/show/NCT02034916 (2019).
Swift, S. L. et al. Effect of DNA damage response mutations on prostate cancer prognosis: a systematic review. Future Oncol. 15, 3283–3303 (2019).
Maxwell, K. N. et al. BRCA locus-specific loss of heterozygosity in germline BRCA1 and BRCA2 carriers. Nat. Commun. 8, 319 (2017).
Nones, K. et al. Whole-genome sequencing reveals clinically relevant insights into the aetiology of familial breast cancers. Ann. Oncol. 30, 1071–1079 (2019).
Sokol, E. S. et al. Pan-cancer analysis of BRCA1 and BRCA2 genomic alterations and their association with genomic instability as measured by genome-wide loss of heterozygosity. JCO Precis Oncol. 4, 442–465 (2020).
Turner, N. C. et al. Next-generation DNA sequencing (NGS) results for tumours from phase II ABRAZO study of talazoparib after platinum or cytotoxic non-platinum regimens in patients (pts) with advanced breast cancer (ABC) and germline BRCA1/2 (gBRCA) mutations. Ann. Oncol. 30, v108–v109 (2019).
Coleman, R. L. et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 390, 1949–1961 (2017).
Nik-Zainal, S. et al. Landscape of somatic mutations in 560 breast cancer whole-genome sequences. Nature 534, 47–54 (2016).
Jonsson, P. et al. Tumour lineage shapes BRCA-mediated phenotypes. Nature 571, 576–579 (2019).
Polak, P. et al. A mutational signature reveals alterations underlying deficient homologous recombination repair in breast cancer. Nat. Genet. 49, 1476–1486 (2017).
Arnold, K. et al. Lower level of BRCA2 protein in heterozygous mutation carriers is correlated with an increase in DNA double strand breaks and an impaired DSB repair. Cancer Lett. 243, 90–100 (2006).
Savelyeva, L. et al. Constitutional genomic instability with inversions, duplications, and amplifications in 9p23-24 in BRCA2 mutation carriers. Cancer Res. 61, 5179–5185 (2001).
Abkevich, V. et al. Patterns of genomic loss of heterozygosity predict homologous recombination repair defects in epithelial ovarian cancer. Br. J. Cancer 107, 1776–1782 (2012).
Telli, M. L. et al. ABRAZO: exposure-efficacy and -safety analyses of breast cancer patients with germline BRCA1/2 mutations receiving talazoparib in a phase 2 open-label trial. Cancer Res. 78, P1-14-03 (2017).
Meric-Bernstam, F. et al. Survival outcomes by TP53 mutation status in metastatic breast cancer. JCO Precis Oncol. 2018, PO.17.00245 (2018).
Khiabanian, H. et al. Inference of germline mutational status and evaluation of loss of heterozygosity in high-depth, tumor-only sequencing data. JCO Precis Oncol. 2018, https://doi.org/10.1200/PO.17.00148 (2018).
Holstege, H. et al. High incidence of protein-truncating TP53 mutations in BRCA1-related breast cancer. Cancer Res. 69, 3625–3633 (2009).
Na, B. et al. Therapeutic targeting of BRCA1 and TP53 mutant breast cancer through mutant p53 reactivation. NPJ Breast Cancer 5, 14 (2019).
Liu, X. et al. Somatic loss of BRCA1 and p53 in mice induces mammary tumors with features of human BRCA1-mutated basal-like breast cancer. Proc. Natl Acad. Sci. USA. 104, 12111–12116 (2007).
Jiang, J. et al. p53-dependent BRCA1 nuclear export controls cellular susceptibility to DNA damage. Cancer Res. 71, 5546–5547 (2011).
Feng, Z., Kachnic, L., Zhang, J., Powell, S. N. & Xia, F. DNA damage induces p53-dependent BRCA1 nuclear export. J. Biol. Chem. 279, 28574–28584 (2004).
Mollon, L. et al. Abstract 1207: a systematic literature review of the prevalence of PIK3CA mutations and mutation hotspots in HR+/HER2- metastatic breast cancer. Cancer Res. 78, 1207 (2018).
Michelucci, A. et al. PIK3CA in breast carcinoma: a mutational analysis of sporadic and hereditary cases. Diagn. Mol. Pathol. 18, 200–205 (2009).
Xu, G. et al. ARID1A determines luminal identity and therapeutic response in estrogen-receptor-positive breast cancer. Nat. Genet. 52, 198–207 (2020).
Knijnenburg, T. A. et al. Genomic and molecular landscape of DNA damage repair deficiency across the cancer genome atlas. Cell Rep. 23, 239–254.e236 (2018).
Litton, J. K. et al. Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N. Engl. J. Med. 379, 753–763 (2018).
Blum, J. L. et al. Determinants of response to talazoparib in patients with HER2-negative, germline BRCA1/2-mutated breast cancer. Clin. Cancer Res. 28, 1383–1390 (2022).
Hodgson, D. et al. Analysis of mutation status and homologous recombination deficiency in tumors of patients with germline BRCA1 or BRCA2 mutations and metastatic breast cancer: OlympiAD. Ann. Oncol. 32, 1582–1589 (2021).
Swisher, E. M. et al. Rucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 Part 1): an international, multicentre, open-label, phase 2 trial. Lancet Oncol. 18, 75–87 (2017).
Sun, J. X. et al. A computational approach to distinguish somatic vs. germline origin of genomic alterations from deep sequencing of cancer specimens without a matched normal. PLoS Comput Biol. 14, e1005965 (2018).
Frampton, G. M. et al. Development and validation of a clinical cancer genomic profiling test based on massively parallel DNA sequencing. Nat. Biotechnol. 31, 1023–1031 (2013).
Heeke, A. L. et al. Prevalence of homologous recombination-related gene mutations across multiple cancer types. JCO Precis Oncol. 2018, PO.17.00286 (2018).
Chung, J. H. et al. Prospective comprehensive genomic profiling of primary and metastatic prostate tumors. JCO Precis Oncol. 3, PO.18.00283 (2019).
Mondal, G., Stevers, M., Goode, B., Ashworth, A. & Solomon, D. A. A requirement for STAG2 in replication fork progression creates a targetable synthetic lethality in cohesin-mutant cancers. Nat. Commun. 10, 1686 (2019).
Sun, C. et al. BRD4 inhibition is synthetic lethal with PARP inhibitors through the induction of homologous recombination deficiency. Cancer Cell. 33, 401–416.e408 (2018).
Acknowledgements
In Manchester, this trial was undertaken in/supported by the NIHR Manchester Clinical Research Facility at The Christie Hospital NHS Foundation Trust. The ABRAZO study was sponsored by Medivation, which was acquired by Pfizer in September 2016 (grant number not applicable). The authors wish to thank Masaki Mihaila and the Pfizer clinical programming team for the ABRAZO correlative analyses. Medical writing support was provided by Dominic James, PhD, and Hannah Logan, PhD, of CMC AFFINITY, a division of IPG Health Medical Communications, and was funded by Pfizer.
Author information
Authors and Affiliations
Contributions
Conceptualization: MLT, AMW. Methodology: ADL, AM, HSR, JC, MR. Validation: ADL, AM, E-MG, JC, UC, MR. Formal analysis: NCT, ADL, YC. Investigation: AM, E-MG, JE, MLT, PAF, SAH, MR. Resources: ADL, HSR, JC, JE, PAF, SAH, AMW. Data curation: E-MG, JC, UC. Writing - original draft: ADL. Writing - review and editing: all authors. Visualization: JFH, LAA. Supervision: ADL. Project administration: PAF.
Corresponding author
Ethics declarations
Competing interests
NCT declares no competing non-financial interests but the following competing financial interests: advisory board honoraria from AstraZeneca, Exact Sciences, Gilead Sciences, GSK, Guardant, Inivata, Lilly, Novartis, Pfizer, Relay Therapeutics, Repare Therapeutics, Roche/Genentech, and Zentalis; and research funding from AstraZeneca, Guardant Health, Inivata, Invitae, Merck Sharp & Dohme, Natera, Personalis, Pfizer, and Roche/Genentech. ADL, JC, and UC declare no competing non-financial interests but the following competing financial interests: employees of Pfizer and own stocks in Pfizer. MLT declares no competing non-financial interests but the following competing financial interests: research funding (to her institution) from AbbVie, Arvinas, Bayer, Biothera, Calithera Biosciences, EMD Serono, Genentech, GSK, Hummingbird Biosciences, Medivation, Merck, Novartis, OncoSec, Pfizer, PharmaMar, Tesaro and Vertex; and consulting/advisory fees from AbbVie, Aduro Biotech, AstraZeneca, Blueprint Medicines, Daiichi Sankyo, Gilead Sciences, GSK, G1 Therapeutics, Guardant, Immunomedics, Merck, Natera, Novartis, OncoSec, Pfizer, RefleXion, Replicate, Roche/Genentech, and Sanofi. HSR declares no competing non-financial interests but the following competing financial interests: research support to the University of California San Francisco from Astellas Pharma, AstraZeneca, Daiichi Sankyo, Gilead Sciences, GSK, Lilly, Merck & Co., Novartis, OBI Pharma, Pfizer, Pionyr Immunotherapeutics, Roche/Genentech, Sermonix Pharmaceuticals, Taiho Oncology, and Veru; travel support to academic meetings from AstraZeneca, Gilead Sciences, and Merck; and consultancy/advisory support from Blueprint, NAPO, Puma, and Scorpion Therapeutics. AM declares no competing non-financial interests but the following competing financial interests: honoraria from Pfizer, and travel/accommodation support from AstraZeneca and Pierre Fabre. JE declares no competing non-financial interests but the following competing financial interests: consulting fees from AstraZeneca, Daiichi Sankyo, Lilly, Novartis, Pfizer, Roche, and Tesaro; contracted research from AstraZeneca, Daiichi Sankyo, Lilly, Novartis, Odonate, Pfizer, Roche, and Seattle Genetics; and travel support from AstraZeneca, Celgene, Daiichi Sankyo, Lilly, Novartis, Pfizer, and Tesaro. E-MG and LAM have nothing to disclose. JB declares no competing non-financial interests but the following competing financial interests: consultant/advisory board member for AstraZeneca and Pfizer; and submitted a European patent request (EP17382884.9). PAF declares no competing non-financial interests but the following competing financial interests: commercial research grants from Novartis to his institution; speakers bureau honoraria from Amgen, Celgene, Daiichi Sankyo, Novartis, Pfizer, Puma, Roche, and Teva; and consultant/advisory board member for Celgene, Daiichi Sankyo, Novartis, Pfizer, Puma, Roche, and Teva. SAH declares the following non-financial interests: unpaid TRIO-US Chief Medical Officer (until Jan 2023), unpaid consultant/steering committee member for Arvinas, AstraZeneca, Celcuity, Cyomx, Daiichi Sankyo, Dantari, Gilead Sciences, Greenwich Life Sciences, Immunomedics, Lilly, MacroGenics, Novartis, Orum, Pieris Pharmaceuticals, Puma Biotechnology, Roche/Genentech, Sanofi, Seattle Genetics/SeaGen, Zymeworks; and the following competing financial interests: contracted research support (which may include editorial assistance) from Ambrx, Amgen, Arvinas, AstraZeneca, Bayer, BioMarin, Cascadian Therapeutics, Celcuity, Cyomx, Daiichi Sankyo, Dantari, Dignitana, G1 Therapeutics, Gilead Sciences, Greenwich Life Sciences, GSK, Immunomedics, Lilly, MacroGenics, Merrimack, Novartis, OBI Pharma, Orinove, Orum, Pfizer, Phoenix Molecular Design, Pieris Pharmaceuticals, Puma Biotechnology, Radius Health, Roche/Genentech, Sanofi, Seattle Genetics/SeaGen, and Zymeworks. JFH was an employee of Foundation Medicine, Inc. and a stockholder of Roche Holding AG when the study was carried out. LAA declares no competing non-financial interests but the following competing financial interests: employee of Foundation Medicine, Inc. and owns stocks in Roche Holdings AG. YC declares no competing non-financial interests but the following competing financial interests: contractor at Pfizer (until 2021) at the time the work was performed. AMW declares no competing non-financial interests but the following competing financial interests (at the time of the study): consultancy fees from ACCORD, Amgen, AstraZeneca, Athenex, Daiichi Sankyo, Lilly, MSD, NAPP, Novartis, Pfizer, Pierre Fabre, Roche, and Takeda; reimbursement from Amgen, Daiichi Sankyo, and Roche; speaker fees from AstraZeneca, Lilly, Novartis, Pfizer, and Roche; and research funding from Lilly, Novartis, Pfizer, and Roche. He was NCRI Breast Research Group early breast cancer systemic anti-cancer therapy lead 2014–21, ACP strategy director 2018–21, and a member of NHSE Clinical reference group for systemic anti-cancer therapy 2013–21 and clinical advisor to NICE for same period (all unremunerated). He left the NHS in January 2021 and worked for AstraZeneca until March 2022, when he left to concentrate fulltime on Outreach Research & Innovation Group (a company he founded to improve access to clinical trials for cancer patients). He has given talks for Roche and Seagen separately through Andrew Wardley Limited. MER declares no competing non-financial interests but the following competing financial interests: research funding from AstraZeneca and Pfizer; past research funding from AbbVie, Medivation, and Tesaro (at the time the work was performed); travel, accommodation, and expenses from AstraZeneca and other transfer of value from AstraZeneca and Pfizer.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Turner, N.C., Laird, A.D., Telli, M.L. et al. Genomic analysis of advanced breast cancer tumors from talazoparib-treated gBRCA1/2mut carriers in the ABRAZO study. npj Breast Cancer 9, 81 (2023). https://doi.org/10.1038/s41523-023-00561-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41523-023-00561-y