Abstract
Systemic inflammation is believed to contribute to the distant recurrence of breast cancer. We evaluated serum samples obtained at diagnosis from 249 case:control pairs with stage II-III Her2-negative breast cancer with or without subsequent distant recurrence. Conditional logistic regression analysis, with models fit via maximum likelihood, were used to estimate hazard ratios (HRs) and test for associations of cytokines with distant recurrence risk. The only biomarker associated with a significantly increased distant recurrence risk when adjusted for multiple testing was the proinflammatory cytokine IL-6 (HR 1.37, 95% confidence intervals [CI] 1.15, 1.65, p = 0.0006). This prospective-retrospective study provides evidence indicating that higher levels of the cytokine IL-6 at diagnosis are associated with a significantly higher distant recurrence risk.
Similar content being viewed by others
Introduction
Inflammation is a normal physiologic response to injury, including cancer1, and plays a key role in contributing to cancer progression2,3. Inflammation is mediated by cytokines, which are glycoproteins secreted by inflammatory cells that induce several intracellular kinases; chemokines are a subset cytokines that induce chemotaxis of other cells4. Although cytokines mediate inflammation, and inflammation facilitates cancer progression, no studies have evaluated the association between specific cytokines and recurrence of breast cancer.
Prior studies have indicated that elevated C-reactive protein (CRP) and serum amyloid A (SAA) are associated with an increased risk of breast cancer recurrence5. CRP and SAA are nonspecific, acute-phase hepatic proteins secreted in response to cytokines, providing indirect evidence that cytokines may be contributing to breast cancer recurrence. In order to determine which specific cytokines might be mediating this effect, we evaluated the association between distant recurrence of breast cancer and serum levels of 36 human cytokines and chemokines involved in chemotaxis, angiogenesis, and immune system regulation, including effector CD4 + Th1/Th2 and Th17 T cells. We evaluated the association between cytokine levels and distant recurrence in 249 case:control pairs (498 patients) after primary surgery and before systemic adjuvant chemotherapy, and in 17 case:control pairs (34 patients) about 5 years after diagnosis who were without clinical evidence of recurrence.
Results
Study population
Of the 4994 patients enrolled on the parent E5103 trial, a total of 532 patients (10.7%) representing 266 case:control pairs were included in this analysis, including 498 patients representing 249 case:control pairs evaluating only a baseline specimen (which we refer to as parent cohort), plus 34 additional patients representing 17 case:control pairs without recurrence within the first 5 years enrolled in the late relapse EL112 substudy (which we refer to as the late relapse cohort) (Fig. 1, CONSORT Diagram). The distribution of covariates in the study populations are shown in Table 1. For the parent cohort, 88% were younger than 65 years, 46% were pre/peri-menopausal, 64% had hormone-receptor positive disease, 85% had at least one positive axillary node (including 53% with at least four positive axillary nodes), and 66% had tumors with poor histologic grade. Characteristics of the late relapse cohort were largely similar, except less likely to have ER- and PgR-negative disease (6% vs. 36%) and more likely to have low-grade tumors (18% vs. 3%).
Cytokine and chemokine levels at diagnosis and association with distant recurrence
Results for the cytokine and chemokine levels for the 498 patients in the parent cohort are shown in Supplementary Table 1, and for 34 patients in the late relapse cohort after 5 years in Supplementary Table 2. There were at least 200 informative case:control pairs (of a maximum of 249) for 23 of 36 cytokines for the parent cohort (Supplementary Table 3), and at least 11 informative case:control pairs (of a maximum of 17) for 25 of 36 cytokines for the late relapse cohort (Supplementary Table 4).
The only biomarker associated with a significantly increased distant recurrence risk when adjusted for multiple testing was the proinflammatory cytokine IL-6 (HR 1.37, 95% confidence intervals [CI] 1.15, 1.65, p = 0.0006; 232 case:control pairs). Others associated with a two-sided p value <0.05 (but exceeding 0.0014) included the T helper cell inflammatory cytokine IL-17A (HR 1.36, 95% CI 1.10, 1.67, p = 0.0052; 210 case:control pairs), included the chemokine MDC (macrophage-derived chemokine/CCL22) (HR 1.58, 95% CI 1.07, 2.33, p = 0.02; 249 case:control pairs), and the cytokine VEGF-A (HR 1.13, 95% CI 1.01, 1.27, p = 0.04; 240 case:control pairs) (Supplementary Table 3). There was no statistically significant interaction between elevated VEGF-A levels at diagnosis and benefit from adjuvant bevacizumab (p-value for interaction term = 0.34).
Absolute cytokine/chemokine levels at diagnosis in parent cohort
The median and mean value (and range) in all patients in the parent cohort for the four biomarkers associated with distant recurrence was 0.95 and 7.53 pg/ml (0.04–2761.24 pg/ml) for IL-6, 3.32 and 4.04 pg/ml (0.12–43.11 pg/ml) for IL-17A, 1019.14 and 1081.84 pg/ml (392.86–4063.81 pg/ml) for MDC/CCL22, and 77.88 and 109.38 (0.66–1196.67 pg/mL) for VEGF-A (Supplementary Table 1). There was no significant difference in IL-6 level by histologic grade (Wilcoxon rank sum test comparing grade 1 versus grade 3, p = 0.62).
Cytokines/chemokine levels at diagnosis and time to distant recurrence
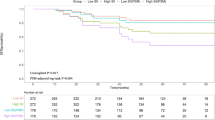
Kaplan–Meier plots for time to distant recurrence are shown in Fig. 2A–D, including IL-6 (Fig. 2A), IL-17A (Fig. 2B), MDC/CCL22 (Fig. 2C), and VEGF-A (Fig. 2D), each showing an association with distant recurrence when evaluated by tertiles.
Box plots showing comparison of log2values in cases versus controls using Wilcoxon signed rank test revealed p values of 0.0002 for IL-6, 0.005 for IL-17A, 0.02 for MDC/CCL22, and 0.06 for VEGF-A (Fig. 3).
Box plots and actual values of log2value (A) for IL-6, IL-17A, MDC/CCL22, and VEGF-A in cases with distant recurrence compared with controls without distant recurrence. Dot plots and actual values of raw values (B) for IL-6, IL-17A, MDC/CCL22, and VEGF-A in cases with distant recurrence compared with controls without distant recurrence.
Dot plots showing comparison of raw values in cases versus controls using Wilcoxon signed rank test revealed p values of 4.7e-05 for IL-6, 0.004 for IL-17A, 0.01 for MDC/CCL22, and 0.02 for VEGF-A.
Association between body mass index at diagnosis and cytokines/chemokines
Of the 498 patients in the parent cohort, 41% (205/498) were obese (BMI ≥ 30 kg/m2), 33% were overweight (BMI 25–29.9 kg/m2), and 26% had a normal BMI at trial entry. High baseline BMI (≥30 kg/m2) was associated with significantly higher IL-6 (p < 0.01) and MDC/CCL22 levels (p = 0.03), but not with IL-17A (p = 0.18) or VEGF-A (p = 0.64) (Supplementary Table 5). There was no significant difference in BMI at trial entry between controls and cases (mean 29.2 versus and 30.4 kg/m2, p = 0.12).
Cytokine and chemokine levels at 5 years and association with distant recurrence
At ~5 years after diagnosis in 34 patients (17 case:control pairs) in the late relapse cohort, exploratory analysis did not identify any biomarker significantly associated with recurrence (Supplementary Table 4), including IL-6 (HR 1.81, 95% CI 0.75, 4.37, p = 0.19, 17 case-control pairs), IL-17A (HR 1.06, 95% CI 0.61, 1.84, p = 0.83, 14 case:control pairs), MDC/CCL22 (HR 1.12, 95% CI 0.19, 6.53, p = 0.89, 17 case:control pairs), and VEGF-A (HR 0.78, 95% CI 0.39, 1,53, p = 0.46, 17 case:control pairs). There was no significant difference in IL-6 level by histologic grade (Wilcoxon rank sum test comparing grade 1 versus grade 3, p = 0.60).
Discussion
We performed a case:control study including a total of 532 patients (including 266 case:control pairs) with high-risk stage II–III HER2-negative breast cancer to determine whether one or more serum cytokine levels at diagnosis, or 5 years after diagnosis when cancer-free, was associated with distant breast cancer recurrence despite surgery and adjuvant chemotherapy (plus endocrine therapy if ER-positive disease). We employed a discovery-based panel of 36 human cytokines and chemokines selected based on evidence for their role in chemotaxis, angiogenesis, and immune system regulation. Four cytokines measured at diagnosis were associated with distant recurrence, including the cytokine IL-6, IL-17A, and VEGF-A, and the chemokine MDC/CCL22. This prospective:retrospective study performed in accordance with REMARK biomarker guidelines6 demonstrates an association between serum cytokine levels and distant breast cancer recurrence, providing a foundation for additional validation of these findings in other cohorts. Similar associations were not observed when blood samples were evaluated 5 years after diagnosis in those who were recurrence-free and had later recurrence, although the sample size was limited, and less than planned.
Of the four cytokines associated with distant recurrence, IL-6 had the most robust association, and the only one whose association was statistically significant after adjustment for multiple testing (HR 1.37, p = 0.0006). The IL-6/JAK/STAT3 pathway has a key role in the growth and development of many human cancers. Elevated levels of IL-6 are observed in chronic inflammatory conditions, such as rheumatoid arthritis and inflammatory bowel disease, and in a variety of cancers7, including breast cancer8. IL-6 stimulates hyperactivation of JAK/STAT3 signaling, which promotes tumor proliferation, angiogenesis, invasiveness, and immunosuppression9. There are currently two approved agents targeting IL-6, including antibodies targeting IL-6 (siltuximab) or the IL-6 receptor (tocilizumab). Siltuximab is chimeric mouse–human antibody approved for the treatment of multicentric Castleman disease10. Tocilizumab is a humanized monoclonal antibody approved for the treatment of systemic juvenile idiopathic arthritis and cytokine-release syndrome occurring in adults or children after CAR-T cells11,12. A number of trials are ongoing evaluating the combination of IL-6 antibodies plus cytotoxic therapy in a variety of cancer types9. Evaluation of such combinations in the neoadjuvant setting, with pathologic response as the endpoint as in the I-SPY trial13, may be a reasonable strategy to determine whether high IL-6 levels identify a population that may benefit targeting the IL-6 axis, and whether larger scale trials are warranted.
Three other cytokines demonstrated an association with distant recurrence, including IL-17A, macrophage-derived chemokine/CCL22, VEGF-A, though not statistically significant after adjustment for multiple testing. IL-17A is a pro-inflammatory cytokine that plays critical role in host defenses on barrier surfaces, and plays a role in autoimmune conditions14. The primary function of Th17 cells that secrete IL-17A includes control of the gut microbiota and clearance of extracellular bacteria and fungi14. Several monoclonal antibodies that inhibit the function of IL-17A have been approved for psoriasis and psoriatic arthritis (secukinumab, ixekizumab, brodulmab)15. Evidence indicates that IL-17A may also have a role in promoting metastasis by eliciting expansion and polarization of neutrophils that suppress cytotoxic CD8 T lymphocytes in mouse mammary tumors, thereby promoting metastasis, which may be abrogated by neutralization of IL-17A16. IL-17A can also enhance tumor growth in vivo through the induction of IL-617. Chemokines such as MDC/CCL22 provide directional cues during migration of leukocytes to damaged or infected tissues, including cancer18. Finally, VEGF-A is a cytokine that facilitates growth of new blood vessels. The anti-VEGF antibody has been extensively evaluated for the treatment of metastatic breast cancer, where it modestly prolongs progression-free survival when added to chemotherapy, but did not improve overall survival19. In metastatic breast cancer, pretreatment plasma VEGF-A level was not predictive of benefit from bevacizumab20. In addition, adjuvant bevacizumab was not effective in reducing distant recurrence risk when added to adjuvant chemotherapy21. This experience with VEFG-A as a biomarker for predicting benefit from bevacizumab highlights the limitations of this approach with the other potentially promising biomarkers identified in our study.
Obesity has been associated with increased recurrence risk in localized estrogen-receptor positive breast cancer22,23. Although higher BMI was associated with significantly higher IL-6 (p < 0.01) and MDC/CCL22 levels (p = 0.03), there was no significant difference in mean BMI in cases with recurrence compared with controls without recurrence. Further evaluation of IL-6 and MDC/CCL22 as prognostic biomarkers should include evaluation of BMI as a confounding factor.
In conclusion, higher serum levels of several cytokines at diagnosis was associated with an increased distant recurrence risk in localized breast cancer, providing a foundation for further assessment and prospective validation of IL-6, IL-17A, and MDC/CCL22 as prognostic biomarkers, and IL-6 as a candidate predictive marker for therapeutic strategies targeting the IL-6/JAK/STAT3 pathway. Strengths of the analysis include the prospective-retrospective study design conducted in accordance with REMARK guidelines and use of a multiplex cytokine panel including selected biomarkers, whereas limitations include lack of validation in an independent cohort, and inadequate sample size for the late relapse cohort.
Methods
Eligibility criteria
The study population included patients enrolled in a previously completed E5103 adjuvant clinical trial (NCT00433511), which accrued 4994 patients with node-positive or high-risk node-negative, human epidermal growth factor receptor 2 (Her2)-negative operable breast cancer between November 2007 and February 2011. The protocol stipulated adjuvant therapy including sequential doxorubicin/cyclophosphamide-paclitaxel chemotherapy alone or in combination with bevacizumab, plus endocrine therapy for patients with hormone receptor-positive disease. Five-year invasive disease-free survival rates ranged from 76–80%, and were not significantly impacted by bevacizumab use21. Trial participants were eligible to participate in a late recurrence substudy (EL112) if they were without clinical evidence of recurrence based on history and physical exam between 4.5 and 7.5 years after registration in the original E5103 trial and consented to participate in the substudy.
Study design and statistical analysis plan
This prospective-retrospective study was designed and results reported in accordance with the REMARK guidelines6. The primary endpoint was time to distant recurrence, defined as date from registration to first invasive distant recurrence; patients without documentation of invasive distant recurrence were censored at date last known disease-free. Clinical recurrences were determined by the local treating physician based on clinical, radiographic, and pathologic information, and confirmed by a research coordinator in the ECOG-ACRIN data management center and study principal investigator (KDM). Propensity score matching was used to identify ~250 case: control pairs with and without distant recurrence. The covariates used to create propensity score matching included age (<40(referent), 40–64, ≥65 years), menopausal status (pre/peri vs. post), estrogen/progesterone receptor expression (both negative vs. one or both positive), tumor size (≤2 cm(referent), 2–5 cm, >5 cm), axillary nodal status (negative(referent), 1–3 positive, ≥4 positive), and histologic grade (I (referent), II, III).
Conditional logistic regression analysis, with models fit via maximum likelihood, were used to estimate hazard ratios (HR) and test for associations. With ~250 matched pairs, it was estimated that there was 80% power to detect a HR of 1.66 using methods previously described24. As an additional exploratory aim, we evaluated an additional 17 case-control pairs (of 24 planned to provide 80% power to detect a HR of 6.45) including patients without recurrence within the first 4.5–7.5 years after diagnosis who provided a blood specimen a part of the EL112 substudy. Due to skewed nature of cytokines, HRs are reported on Log2 (log base 2); therefore, a two-fold elevation in the original value of a marker was associated with the stated HR for distant recurrence. The Kaplan–Meier method was used to estimate time to recurrence distributions by tertiles. Wilcoxon test as appropriate or Kruskal Wallis test (>2 category variable) was used to test for associations between markers and baseline demographic and disease characteristic categorical variables. Note that the results for markers are reported among the informative pairs (where marker values were available for the case and the control within the matched pair). Given multiple comparisons across many cytokines with relatively few informative case:control pairs, HR estimates with p-value < 0.002 would be considered for statistical significance (Bonferroni adjustment: 0.05/23 for 23 of 36 cytokines with ≥200 informative pairs). If considering all 36 markers, a p-value of <0.0014 would be required for statistical significance. Because of the association between obesity and inflammation, the association between body mass index with cytokine values was also evaluated. All statistical analyses were performed using SAS9.4 and R 3.6.1. For the graph in Fig. 3B, a total of 10 pairs (20 patients) were excluded due to outlying values outside of the ranges used in the graph, including 5 pairs for IL6, 3 pairs for IL17A, and pairs from VEGF-A; these values are included in the table appearing in Fig. 3B, and also included in the statistical comparison.
Cytokine/chemokine assay
Serum samples were collected at the time of trial registration after potentially curative primary surgery, and before systemic adjuvant therapy. Archived frozen serum samples stored in the ECOG-ACRIN Central Biorepository and Pathology Facility (CBPF) at the MD Anderson Cancer Center were analyzed using the MSD V-Plex Human Cytokine 36-Plex Kit (https://www.mesoscale.com/products/v-plex-plus-human-cytokine-36-plex-kit-k15089g) for detection of a panel of 36 human cytokines and chemokines, including the following: Eotaxin, Eotaxin-3, GM-CSF, IFN-γ, IL-10, IL-12/IL-23p40, IL-12p70, IL-13, IL-15, IL-16, IL-17A, IL-1α, IL-1β, IL-2, IL-21, IL-22, IL-23, IL-27, IL-31, IL-4, IL-5, IL-6, IL-7, IL-8, IL-8 (HA), IP-10, MCP-1, MCP-4, MDC, MIP-1α, MIP-1β, MIP-3α, TARC, TNF-α, TNF-β, VEGF-A. Samples were analyzed in accordance with the manufacturer’s instructions by the Translational Molecular Pathology and Immunoprofiling Lab Oncology Research and Immuno-monitoring Core at MD Anderson Cancer Center.
Study oversight
The first author (J.A.S.) wrote the manuscript, the second and third authors (A.O., N.G.) performed the statistical analysis, and the final version incorporated changes recommended by the coauthors. Data were collected by the ECOG–ACRIN Cancer Research Group Coordinating Center. All the authors vouch for the accuracy and completeness of the data and analyses presented and for the adherence of the study to the protocol. No commercial support was involved in the planning or execution of this secondary analysis of the E5103 trial. The parent E5103 study and EL112 late relapse substudy were reviewed and approved by the Cancer Therapy Evaluation Program, National Cancer Institute, and by the local institutional review board at each participating center.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The datasets generated during and/or analyzed during the current study are available in the NCTN/NCORP Data Archive (https://nctn-data-archive.nci.nih.gov).
References
Furman, D. et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 25, 1822–1832 (2019).
Coussens, L. M. & Werb, Z. Inflammation and cancer. Nature 420, 860–867 (2002).
DeNardo, D. G. & Coussens, L. M. Inflammation and breast cancer. Balancing immune response: crosstalk between adaptive and innate immune cells during breast cancer progression. Breast Cancer Res. 9, 212 (2007).
Esquivel-Velazquez, M. et al. The role of cytokines in breast cancer development and progression. J. Interferon Cytokine Res. 35, 1–16 (2015).
Pierce, B. L. et al. Elevated biomarkers of inflammation are associated with reduced survival among breast cancer patients. J. Clin. Oncol. 27, 3437–3444 (2009).
McShane, L. M. et al. Reporting recommendations for tumor marker prognostic studies (REMARK). J. Natl Cancer Inst. 97, 1180–1184 (2005).
Vainer, N., Dehlendorff, C. & Johansen, J. S. Systematic literature review of IL-6 as a biomarker or treatment target in patients with gastric, bile duct, pancreatic and colorectal cancer. Oncotarget 9, 29820–29841 (2018).
Knupfer, H. & Preiss, R. Significance of interleukin-6 (IL-6) in breast cancer (review). Breast Cancer Res. Treat. 102, 129–135 (2007).
Johnson, D. E., O’Keefe, R. A. & Grandis, J. R. Targeting the IL-6/JAK/STAT3 signalling axis in cancer. Nat. Rev. Clin. Oncol. 15, 234–248 (2018).
van Rhee, F. et al. Siltuximab for multicentric Castleman’s disease: a randomised, double-blind, placebo-controlled trial. Lancet Oncol. 15, 966–974 (2014).
Smolen, J. S. et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomised trial. Lancet 371, 987–997 (2008).
Le, R. Q. et al. FDA approval summary: tocilizumab for treatment of chimeric antigen receptor T cell-induced severe or life-threatening cytokine release syndrome. Oncologist 23, 943–947 (2018).
Esserman, L. The I-SPY approach to drug development. Clin. Adv. Hematol. Oncol. 14, 782–784 (2016).
Chen, K. & Kolls, J. K. Interluekin-17A (IL17A). Gene 614, 8–14 (2017).
Amatya, N., Garg, A. V. & Gaffen, S. L. IL-17 Signaling: The Yin and the Yang. Trends Immunol. 38, 310–322 (2017).
Coffelt, S. B. et al. IL-17-producing gammadelta T cells and neutrophils conspire to promote breast cancer metastasis. Nature 522, 345–348 (2015).
Wang, L. et al. IL-17 can promote tumor growth through an IL-6-Stat3 signaling pathway. J. Exp. Med. 206, 1457–1464 (2009).
Balkwill, F. R. The chemokine system and cancer. J. Pathol. 226, 148–157 (2012).
Hey, S. P. et al. A Systematic review and meta-analysis of bevacizumab in first-line metastatic breast cancer: lessons for research and regulatory enterprises. J. Natl Cancer Inst. 112, 335–342 (2020).
Miles, D. et al. Bevacizumab plus paclitaxel versus placebo plus paclitaxel as first-line therapy for HER2-negative metastatic breast cancer (MERiDiAN): a double-blind placebo-controlled randomised phase III trial with prospective biomarker evaluation. Eur. J. Cancer 70, 146–155 (2017).
Miller, K. D. et al. Double-blind phase III trial of adjuvant chemotherapy with and without bevacizumab in patients with lymph node-positive and high-risk lymph node-negative breast cancer (E5103). J. Clin. Oncol. 36, 2621–2629 (2018).
Sparano, J. A. et al. Obesity at diagnosis is associated with inferior outcomes in hormone receptor-positive operable breast cancer. Cancer 118, 5937–5946 (2012).
Pan, H. & Gray, R. G., Group, o. b. o. t. E. B. C. T. C. Effect of obesity in premenopausal ER+ early breast cancer: EBCTCG data on 80,000 patients in 70 trials. J. Clin. Oncol. 32, 503–503 (2014).
Dupont, W. D. Power calculations for matched case-control studies. Biometrics 44, 1157–1168 (1988).
Acknowledgements
This study was coordinated by the ECOG-ACRIN Cancer Research Group (Peter J. O’Dwyer, MD and Mitchell D. Schnall, MD, PhD, Group Co-Chairs) and supported by the National Cancer Institute of the National Institutes of Health under the following award numbers: U10CA180820, U10CA180794, U10CA180821, UG1CA189859, UG1CA232760, UG1CA233290, and UG1CA233196. Also supported by the Breast Cancer Research Foundation and Susan G. Komen Foundation (J.A.S., MD). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. government.
Author information
Authors and Affiliations
Contributions
Conception and design or acquisition, analysis, or interpretation of the data: J.A.S., A.O’.N, N.G., J.A.S., D.W.N., C.T.D., A.C.W., G.W.S., and K.D.M. Drafting of work or revising it critically: J.A.S., A.O’.N., N.G., J.A.S., D.W.N., C.T.D., A.C.W., G.W.S., and K.D.M. Final approval of the completed work: J.A.S., A.O’.N., N.G., J.S., D.W.N., C.T.D., A.C.W., G.W.S., and K.D.M. Accountability for all aspects of the work: J.A.S., A.O.’N., N.G., J.A.S., D.W.N., C.T.D., A.C.W., G.W.S., and K.D.M.
Corresponding author
Ethics declarations
Competing interests
J.A.S. is an Associate Editor for npj Beast Cancer. The authors otherwise report no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sparano, J.A., O’Neill, A., Graham, N. et al. Inflammatory cytokines and distant recurrence in HER2-negative early breast cancer. npj Breast Cancer 8, 16 (2022). https://doi.org/10.1038/s41523-021-00376-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41523-021-00376-9