Abstract
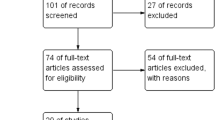
Though early research suggested that thyroid hormones were not involved with the testes, male spermatogenesis, or erectile function, investigations on this topic over the past few decades have increased and shed new light. A literature review of studies conducted between 1963 and 2022 regarding male sexual dysfunction (SD) and thyroid disorders was performed to define the diagnostic consideration, pathophysiology, and management of SD secondary to thyroid dysregulation. This article provides evidence and interpretation of prior clinical and preclinical studies and contextualizes these studies for clinical practice. Clinical manifestations of SDs included erectile and ejaculatory dysfunction, impaired spermatogenesis, and disruption of the hypothalamic-pituitary-gonadal axis. Our aim of this communication was to perform a literature review detailing the impact of thyroid disorders on male SD. We hope to provide a framework for practicing urologists, endocrinologists, or general practitioners when evaluating patients with concurrent thyroid and male SD. It is important to recognize that thyroid disorders can be an important part of the pathophysiology of male SD in patients. Future research studies are needed to further elucidate the mechanisms involved.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The data in this paper can be found by searching the listed references on PubMed.
References
Gabrielson AT, Sartor RA, Hellstrom WJG. The impact of thyroid disease on sexual dysfunction in men and women. Sex Med Rev. 2019;7:57–70. https://doi.org/10.1016/j.sxmr.2018.05.002.
Jannini EA, Ulisse S, Armiento MD. Thyroid hormone and male gonadal function. Endocr Rev. 1995;16:443–59. https://doi.org/10.1210/edrv-16-4-443.
Corona G, Wu FCW, Forti G, Lee DM, O’Conner DB, O’Neil TW, et al. Thyroid hormones and male sexual function. Int J Androl. 2012;35:668–79. https://doi.org/10.1111/j.1365-2605.2012.01266.x.
Marques P, Skorupskaite K, Rozario KS, Anderson RA, George JT. Physiology of GnRH and gonadotropin secretion. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext. South Dartmouth (MA): MDText.com, Inc.; 2000. https://www.ncbi.nlm.nih.gov/books/NBK279070/.
Sadiq NM, Tadi P. Physiology, pituitary hormones. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK557556/.
Vagenakis AG. Pituitary-thyroid interaction: effects of thyroid hormone, non thyroidal illness and various agents on TSH secretion. Acta Med Austriaca. 1988;15:52–6.
Caraty A, Martin GB, Montgomery G. A new method for studying pituitary responsiveness in vivo using pulses of LH-RH analogue in ewes passively immunized against native LH-RH. Reprod Nutr Dev. 1984;24:439–48. https://doi.org/10.1051/rnd:19840409.
Huhtaniemi IT. LH and FSH receptor mutations and their effects on puberty. Horm Res. 2002;57:35–38. https://doi.org/10.1159/000058098.
Griswold MD. The central role of Sertoli cells in spermatogenesis. Semin Cell Dev Biol. 1998;9:411–6. https://doi.org/10.1006/scdb.1998.0203.
Rastrelli G, Corona G, Maggi M. Testosterone and sexual function in men. Maturitas. 2018;112:46–52. https://doi.org/10.1016/j.maturitas.2018.04.004.
Sengupta P, Dutta S, Karkada IR, Chinni SV. Endocrinopathies and male infertility. Life. 2021;12:10. https://doi.org/10.3390/life12010010.
Abalovich M, Levalle O, Hermes R, Scaglia H, Aranda C, Zylbersztein C, et al. Hypothalamic-pituitary-testicular axis and seminal parameters in hyperthyroid males. Thyroid. 1999;9:857–63. https://doi.org/10.1089/thy.1999.9.857.
Donnelly P, White C. Testicular dysfunction in men with primary hypothyroidism; reversal of hypogonadotrophic hypogonadism with replacement thyroxine. Clin Endocrinol. 2000;52:197–201. https://doi.org/10.1046/j.1365-2265.2000.00918.x.
Oppenheimer JH, Schwartz HL, Surks MI. Tissue differences in the concentration of triiodothyronine nuclear binding sites in the rat: liver, kidney, pituitary, heart, brain, spleen, and testis. J Endocrinol. 1974;95:897–903. https://doi.org/10.1210/endo-95-3-897.
Barker SB, Klitgaard HM. Metabolism of tissues excised from thyroxine-injected rats. Am J Physiol. 1952;170:81–6. https://doi.org/10.1152/ajplegacy.1952.170.1.81.
Holsberger DR, Cooke PS. Understanding the role of thyroid hormone in Sertoli cell development: a mechanistic hypothesis. Cell Tissue Res. 2005;322:133–40. https://doi.org/10.1007/s00441-005-1082-z.
Sakai Y, Yamashina S, Furudate S. Developmental delay and unstable state of the testes in the rdw rat with congenital hypothyroidism. Dev Growth Differ. 2004;46:327–34. https://doi.org/10.1111/j.1440-169x.2004.00748.x.
Jannini EA, Dolci S, Ulisse S, Nikodem VM. Developmental regulation of the thyroid hormone receptor alpha 1 mRNA expression in the rat testis. Mol Endocrinol. 1994;8:89–96. https://doi.org/10.1210/mend.8.1.8152433.
Hernandez A. Thyroid hormone role and economy in the developing testis. Vitam Horm. 2018;106:473–500. https://doi.org/10.1016/bs.vh.2017.06.005.
Maran RR, Sivakumar R, Arunakaran J, Ravisankar B, Ravichandran K, Sidharthan V, et al. Duration-dependent effect of transient neonatal hypothyroidism on sertoli and germ cell number, and plasma and testicular interstitial fluid androgen binding protein concentration. Endocr Res. 1999;25:323–40. https://doi.org/10.1080/07435809909066151.
Mendis-Handagama SM, Ariyaratne HB. Effects of hypothyroidism on anti-mullerian hormone expression in the prepubertal rat testis. Histol Histopathol. 2008;23:151–6. https://doi.org/10.14670/HH-23.151.
Sun Y, Yang W, Luo H, Wang X, Chen Z, Zhang J, et al. Thyroid hormone inhibits the proliferation of piglet Sertoli cell via PI3K signaling pathway. Theriogenology. 2015;83:86–94. https://doi.org/10.1016/j.theriogenology.2014.08.003.
Holsberger DR, Buchold GM, Leal MC, Kiesewetter SE, O’Brien DA, Hess RA, et al. Cell-cycle inhibitors p27Kip1 and p21cip1 regulate murine sertoli cell proliferation. Biol Reprod. 2005;72. https://doi.org/10.1095/biolreprod.105.040386.
Fumel B, Guerquin MJ, Livera G, Staub C, Magistrini M, Gauthier C, et al. Thyroid hormone limits postnatal Sertoli cell proliferation in vivo by activation of its alpha1 isoform receptor (TRalpha1) present in these cells and by regulation of Cdk4/JunD/c-myc mRna levels in mice. Biol Reprod. 2012;87:16–9. https://doi.org/10.1095/biolreprod.111.098418.
Cardone A, Angelini F, Esposito T, Comitato R, Varriale B. The expression of androgen receptor messenger RNA is regulated by tri-iodothyronine in lizard testis. J Steroid Biochem Mol Biol. 2000;72:133–41. https://doi.org/10.1016/S0960-0760(00)00021-2.
Catalano S, Pezzi V, Chimento A, Giordano C, Carpino A, Young M, et al. Triiodothyronine decreases the activity of the proximal promoter (PII) of the aromatase gene in the mouse Sertoli cell line, TM4. Mol Endocrinol. 2003;17:923–34. https://doi.org/10.1210/me.2002-0102.
Rao JN, Liang JY, Chakraborti P, Feng P. Effect of thyroid hormone on the development and gene expression of hormone receptors in rat testes in vivo. J Endocrinol Invest. 2003;26:435–43. https://doi.org/10.1007/BF03345199.
Kobayashi K, Kubota H, Hojo R, Miyagawa M. Dose-dependent effects of perinatal hypothyroidism on postnatal testicular development in rat offspring. J Toxicol Sci. 2014;39:867–74. https://doi.org/10.2131/jts.39.867.
Lagu SK, Bhavsar NG, Sharma RK, Ramachandran AV. Neonatal hypothyroidism-induced changes in rat testis size, dependence on temperature. Neuro Endocrinol Lett. 2005;26:780–8.
Souhila DS, Zohra HS, Kamel A, Hadj-Bekkouche F. Effects of thyroxine treatment during lactation on the testicular function of rats across different ages. Folia Histochem Cytobiol. 2013;51:107–14. https://doi.org/10.5603/FHC.2013.0017.
Marchlewska K, Kula K, Walczak-Jedrzejowska R, Oszukowska E, Orkisz S, Slowikowska-Hilczer J. Triiodothyronine modulates initiation of spermatogenesis in rats depending on treatment timing and blood level of the hormone. Mol Cell Endocrinol. 2011;341:25–34. https://doi.org/10.1016/j.mce.2011.04.022.
Faraone-Mennella MR, Ferone A, Marino L, Cardone A, Comitato R, Venditti P, et al. Poly(ADP-ribosyl)ation of proteins and germ cell development in hyperthyroid rat testes. Mol Cell Biochem. 2009;323:119–29. https://doi.org/10.1007/s11010-008-9970-7.
Sarkar D, Singh SK. Neonatal hypothyroidism affects testicular glucose homeostasis through increased oxidative stress in prepubertal mice: effects on GLUT3, GLUT8 and Cx43. J Androl. 2017;5:749–62. https://doi.org/10.1111/andr.12363.
Fernández V, Videla LA. Hepatic glutathione biosynthetic capacity in hyperthyroid rats. Toxicol Lett. 1996;89:85–9. https://doi.org/10.1016/s0378-4274(96)03791-5.
Nikoobakht MR, Aloosh M, Nikoobakht N, Mehrsay AR, Biniaz F, Karjalian MA. The role of hypothyroidism in male infertility and erectile dysfunction. Urol J. 2012;9:405–9.
Rehman R, Zafar A, Fatima SS, Mohib A, Sheikh A. Altered sperm parameters and subclinical hypothyroidism; a cross sectional study in Karachi, Pakistan. Int J Clin Pr. 2020;74:e13555. https://doi.org/10.1111/ijcp.13555.
Zhao S, Tang L, Fu J, Yang Z, Su C, Rao M. Subclinical hypothyroidism and sperm DNA fragmentation: a cross-sectional study of 5401 men seeking infertility care. J Clin Endocrinol Metab. 2022;107:e4027–36. https://doi.org/10.1210/clinem/dgac458.
Rao M, Yang Z, Su C, Zhao Z, Wan R, Liu J, et al. Paternal subclinical hypothyroidism affects the clinical outcomes of in vitro fertilization/intracytoplasmic sperm injection. Thyroid. 2021;31:12–22. https://doi.org/10.1089/thy.2020.0154.
Rao M, Wang L, Yan G, Chen M, Tang L, Zhao S. Normal-range paternal serum-free thyroxine concentrations and outcomes of assisted reproductive technologies. Thyroid. 2022;32:705–13. https://doi.org/10.1089/thy.2022.0049.
La Vignera S, Vita R. Thyroid dysfunction and semen quality. Int J Immunopathol Pharm. 2018;32:2058738418775241. https://doi.org/10.1177/2058738418775241.
Krassas GE, Pontikides N, Deligianni V, Miras K. A prospective controlled study of the impact of hyperthyroidism on reproductive function in males. J Clin Endocrinol Metab. 2002;87:3667–71. https://doi.org/10.1210/jcem.87.8.8714.
Veronelli A, Masu A, Ranieri R, Rognoni C, Laneri M, Pontiroli AE. Prevalence of erectile dysfunction in thyroid disorders: comparison with control subjects and with obese and diabetic patients. Int J Impot Res. 2006;18:111–4. https://doi.org/10.1038/sj.ijir.3901364.
Krassas GE, Tziomalos K, Papadopoulou F, Pontikides N, Perros P. Erectile dysfunction in patients with hyper- and hypothyroidism: how common and should we treat? J Clin Endocrinol Metab. 2008;93:1815–9. https://doi.org/10.1210/jc.2007-2259.
Carani C, Isidori AM, Granata A, Carosa E, Maggi M, Lenzi A, et al. Multicenter study on the prevalence of sexual symptoms in male hypo- and hyperthyroid patients. J Clin Endocrinol Metab. 2005;90:6472–9. https://doi.org/10.1210/jc.2005-1135.
Salvio G, Martino M, Giancola G, Arnaldi G, Balercia G. Hypothalamic–pituitary diseases and erectile dysfunction. J Clin Med. 2021;10:2551. https://doi.org/10.3390/jcm10122551.
Esposito K, Giugliano D. Obesity, the metabolic syndrome, and sexual dysfunction in men. Clin Pharm Ther. 2011;90:169–73. https://doi.org/10.1038/clpt.2011.91.
Seppet EK, Kaasik A, Minajeva A, Paju K, Ohisalo JJ, Vetter R, et al. Mechanisms of thyroid hormone control over sensitivity and maximal contractile responsiveness to β-adrenergic agonists in atria. Mol Cell Biochem. 1998;184:419–26. https://doi.org/10.1007/978-1-4615-5653-4_29.
Carosa E, Di Sante S, Rossi S, Castri A, D’Adamo F, Gravina GL, et al. Ontogenetic profile of the expression of thyroid hormone receptors in rat and human corpora cavernosa of the penis. J Sex Med Med. 2010;7:1381–90. https://doi.org/10.1111/j.1743-6109.2009.01701.x.
Özdemirci S, Yildiz F, Utkan T, Ulak G, Cetinaslan B, Erden F, et al. Impaired neurogenic and endothelium-dependent relaxant responses of corpus cavernosum smooth muscle from hyperthyroid rabbits. Eur J Pharm. 2001;428:105–11. https://doi.org/10.1016/S0014-2999(01)01268-7.
Corona G, Jannini EA, Vignozzi L, Rastrelli G, Maggi M. The hormonal control of ejaculation. Nat Rev Urol. 2012;9:508–19. https://doi.org/10.1038/nrurol.2012.147.
Cihan A, Demir O, Demir T, Aslan G, Comlekci A, Esen A. The relationship between premature ejaculation and hyperthyroidism. J Urol. 2009;181:1273–80. https://doi.org/10.1016/j.juro.2008.10.150.
Culha MG, Tuken M, Gonultas S, Cakir OO, Serefoglu EC. Frequency of etiological factors among patients with acquired premature ejaculation: prospective, observational, single-center study. Int J Impot Res. 2020;32:352–7. https://doi.org/10.1038/s41443-019-0188-x.
Canat L, Erbin A, Canat M, Dinek M, Caskurlu T. Assessment of hormonal activity in patients with premature ejaculation. Int Braz J Urol. 2017;43:311–6. https://doi.org/10.1590/S1677-5538.IBJU.2016.0064.
Waldinger MD, Quinn P, Dilleen M, Mundayat R, Schweitzer DH, Boolell M. A multinational population survey of intravaginal ejaculation latency time. J Sex Med. 2005;2:492–7. https://doi.org/10.1111/j.1743-6109.2005.00070.x.
Cihan A, Murat N, Demir O, Aslan G, Demir T, Gidener S, et al. An experimental approach to the interrelationship between hyperthyroidism and ejaculation latency time in male rats. J Urol. 2009;181:907–12. https://doi.org/10.1016/j.juro.2008.10.061.
Kravets I. Hyperthyroidism: diagnosis and treatment. Am Fam Physician. 2016;93:363–70.
Biondi B, Cooper DS. Thyroid hormone therapy for hypothyroidism. Endocrine. 2019;66:18–26. https://doi.org/10.1007/s12020-019-02023-7.
Cannarella R, Calogero AE, Aversa A, Condorelli RA, La Vignera S. Is there a role for levo‐thyroxine for the treatment of arterial erectile dysfunction? The clinical relevance of the mean platelet volume. J Clin Med. 2020;9:742. https://doi.org/10.3390/jcm9030742.
Reid JR, Wheeler SF. Hyperthyroidism: diagnosis and treatment. Am Fam Physician. 2005;72:623–30.
Acknowledgements
The authors wish to thank Scott Bailey, PhD, Department of Urology, Tulane University School of Medicine, for editing and preparing this manuscript.
Author information
Authors and Affiliations
Contributions
Conceived and/or designed the work that led to the submission, acquired data, and/or played an important role in interpreting the results: RM, DS, and WJGH. Drafted or revised the manuscript: RM, DS, and WJGH. Approved the final version: WJGH. Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: WJGH.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morenas, R., Singh, D. & Hellstrom, W.J.G. Thyroid disorders and male sexual dysfunction. Int J Impot Res (2023). https://doi.org/10.1038/s41443-023-00768-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-023-00768-4