Abstract
Peyronie’s disease continues to be poorly understood. We characterize the presenting features of Peyronie’s disease within a large cohort and elucidate the factors that correlate with surgical intervention. Univariate and multivariate analyses were performed on 1483 consecutive patients to assess pre-operative predictors of surgical intervention for Peyronie’s disease. Overall, 1263 patients met inclusion criteria. Mean age was 55.4 ± 11.1 years with a mean duration of disease at presentation of 33.2 ± 42.5 months. Mean primary curvature was 49.8 ± 20.8°. Primary ventral curvature was present in 11.4% and 36.5% of patient had a multiplanar curvature. During penile duplex ultrasound evaluation indentation/narrowing deformities were appreciated in 76.0%, hourglass deformity in 10.1%, and hinge effect in 33.0% of patients. Calcification was seen in 30.1% of patients. Operative intervention occurred in 35.3% of patients. Degree of primary curvature (1.03 OR, p < 0.001), hourglass deformity (1.82 OR, p = 0.01), decreased tunical elasticity (1.20 OR, p = 0.03), and prior intralesional collagenase clostridium histolyticum injections (2.94 OR, p < 0.001) predicted surgical correction on multivariate analysis. Compared to historical studies, we found a higher incidence of severe degree of curvature (27.5% >60°), indentation deformities, hinge-effect, multiplanar curvature and penile calcifications. Ultimately, predictors of surgical intervention included those with worse erectile function and more severe characteristics.
Similar content being viewed by others
Introduction
Peyronie’s disease (PD) is a progressive wound-healing disorder resulting in fibrous plaque formation within the tunica albuginea of the penis. While the exact pathophysiology is unknown, the etiology is perceived to be a result of trauma to the erect penis with tunical injury in genetically susceptible individuals and aberrant healing [1, 2]. As a result of PD, patients can experience changes including abnormal penile curvature, narrowing, shortening, pain, erectile dysfunction (ED), difficulties engaging in penetrative intercourse, and psychological distress [3].
While initial studies reported some spontaneous resolution of penile curvature, it is now known that in the absence of active treatment, most men experience stable or worsening curvature, worsening sexual function, penile length loss, and relationship dissatisfaction [3,4,5,6]. Treatment for PD is broad, varies based on symptom severity and stability, and consists of conservative and operative treatments with the goal to make the penis functionally straight, which is reported as being 20-30° or less [7]. Consensus among experts and guidelines is that history and physical examination are adequate for diagnosis, and intracavernosal injection and estimation of penile angulation is the gold standard to evaluate deformity prior to invasive intervention [8]. There is no single treatment modality that is considered standard of care, thus shared decision-making is important.
Presenting features of PD vary and includes an acute inflammatory phase, followed by a chronic phase where stability of the deformity occurs. The acute phase (active) lasts 6 to greater than 12 months and is characterized by penile pain, minor curvature, and a palpable scar or nodule [8, 9]. The chronic phase (stable) of PD is characterized by a palpable plaque with a deformity that is no longer progressive [1]. To date, there are no firmly agreed-upon criteria characterizing the transition to chronic PD given the broad patient presentations within the literature, but there is agreement that all patients must be in the stable phase (deformity unchanged for a minimum of 3–6 months) before surgical intervention [3, 8].
Referral patterns for PD vary depending on physician knowledge of the disease and comfort with management [5, 10]. Most commonly, PD patients will have a singular plaque and uniplanar curvature in the dorsal or lateral direction of the erect penis, although there are numerous presentations including those categorized as “atypical”. Previous studies have reported ~10–39% of patients with PD have atypical features (ventral plaques, hourglass deformities, unilateral indentations, severely shortened penile length, and multiplanar curvatures) [11, 12]. Most series do not provide details on how they classified these atypical features, although hourglass deformities are typically bilateral notching or indentation at the same level of the penile shaft (>10% of penile girth discrepancy and distal from the greatest curvature); and multiplanar curvatures (plaques causing multiple angulations at different levels of the penis) [13]. Treatment of atypical PD poses unique challenges, and some conventional treatment methods such as intralesional injections are off label for these patients. We aim to analyze within a tertiary referral center the presenting features of PD, treatment, and outcomes. Within this database, we attempt to perform objective deformity characterization of all patients.
Materials and Methods
We retrospectively identified all new patients presenting for PD from 2016-2021 for a minimum 1-year follow-up. Institutional Review Board approval was obtained. Patient charts were analyzed for demographics, comorbidities, physical exam findings, penile duplex, non-operative treatments, and when applicable surgical approach and outcomes. All patients included had evidence of PD at examination by a single urologist with expertize in PD management. Patients were tracked longitudinally, and subsequent interventions and outcomes were collected. Patients were excluded if they only had virtual visits, refused penile duplex evaluation, or had PD surgical correction prior to presentation.
Baseline demographics and comorbidities analyzed included age, duration of care, body mass index, presence of: hypertension, hyperlipidemia, diabetes mellitus, coronary artery disease, prostate cancer, hypogonadism, and tobacco history.
ED specific characteristics analyzed included rigidity with most effective treatment (0-10), prior and/or current use of: phosphodiesterase type 5 (PDE5) inhibitors, intracavernosal injections, and/or vacuum erection device.
PD specific characteristics analyzed included PD duration, duration of stability, history of trauma, penile shortening, ability to have penetrative intercourse, prior and/or current use of: oral PD therapies (Vitamin E, Carnitine, L-Arginine, Pentoxifylline, Potassium aminobenzoate, Colchicine, Tamoxifen, and/or PDE5 inhibitors), intralesional PD therapies (verapamil, and/or collagenase clostridium histolyticum (CCH)), mechanical therapies (penile traction and/or vacuum therapies).
A physical examination was performed on all patients. Clinical examination included stretched penile length (pubis to corona dorsally), presence and location of plaque(s), penile elasticity (tunical compliance as a surrogate for extent of scarring: normal, diminished, or poor), intracavernosal injection with subsequent penile duplex ultrasound (those with incomplete erection were redosed before ultrasound assessment to ensure optimal rigidity), erection rigidity (0-10), ability to maintain erection, direction and degree of primary curvature (measured using a goniometer), direction and degree of secondary/multiplanar curvature, degree of composite curvature (when applicable adding degree of curvature in 2 planes), calcification (measured by ultrasound, grade 1: <0.3 cm, grade 2: 0.3–1.5 cm, and grade 3 ≥ 1.5 cm or 2 or more plaques > 1.0 cm) [14], narrowing/hourglass, hinge/instability (buckling of the erect penis at a point of narrowing with application of axial pressure to the glans), indentation (unilateral or circumferential narrowing), penile girth (penile circumference at base, point of narrowing, sub-coronal), any prior PD treatments and rigidity of the erection during duplex ultrasound as compared to the patient’s “home” sexually induced erection (same, better, worse).
For patients ultimately undergoing surgery, intervention was likewise performed by a single surgeon based on previously published surgical algorithm [15, 16]. Operative interventions included tunica albuginea plication (TAP), plaque incision and grafting or partial plaque excision and grafting (PEG) with or without TAP, and inflatable penile prosthesis (IPP) implantation with or without incision and grafting or manual modeling [17,18,19,20]. Additional operative details for IPP included incision approach (penoscrotal, subcoronal, infrapubic, or combined), cylinder and reservoir sizes, reservoir location, and drain placement. For grafting procedure, type of graft was included (Tachosil (Baxter Healthcare, Deerfield, IL, USA), Tutoplast (Coloplast, Minneapolis, MN, USA), NuKnit (Ethicon Inc., Somerville, NJ, USA), Evarrest (Ethicon Inc., Somerville, NJ, USA)).
Statistical analysis was performed using IBM SPSS Statistics Version 26. A p-value of <0.05 was considered statistically significant. Univariate analyses were performed on baseline demographics, comorbidities, ED- and PD-specific characteristics, non-operative interventions, and their correlation with operative intervention, and timing of referral. All proportional data are presented as percentages and were analyzed using chi-square tests. All continuous data are presented as mean ± standard deviation and were compared using two-tailed, unpaired Student’s t-tests and analysis of variance. Predictive variables in univariate analysis were input into a binary logistic regression model in a stepwise fashion and were presented with odds ratios and 95% confidence interval.
Results
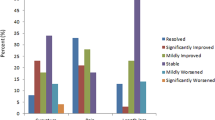
During the study period, 1483 patients were encountered, of which 1263 patients met inclusion criteria. Mean patient age was 55.4 ± 11.1 (range 18-83) years. The mean duration of PD symptoms was 33.2 ± 42.5 (range 0-440) months. The majority (74.9%) of patients were still capable of having penetrative sexual intercourse (Table 1). Mean curvature magnitude in primary direction was 49.8 ± 20.8 (range 5-120)°. Multiplanar curvature was present in 36.5% of patients. Curvature breakdown by direction included dorsal curvature (63.0%), lateral curvature (25.6%), ventral curvature (11.4%). Indentation/narrowing deformities were present in 76.0% of patients, 10.1% had hourglass deformities, and 33.0% had hinge effect. Calcification was identified in 30.1% of patients (Table 2).
Ultimately, 446 (35.3%) underwent operative intervention, 252 (56.5%) without ED, 156 (35.0%) underwent PEG, and 96 (21.5%) underwent TAP. In 194 (43.5%) patients with concomitant ED, 166 (85.6%) underwent IPP placement with or without manual modeling and PEG, while 14 (3.1%) underwent PEG alone, and 14 (3.1%) underwent TAP alone. Revision surgery or repeat operative intervention occurred in 6.9% of patients (Table 3).
On univariate analysis, patients who ultimately underwent surgery were older (56.6 ± 9.3 vs 54.8 ± 12.0 years, p = 0.003), had greater BMI (27.6 ± 3.8 vs 27.1 ± 4.6, p = 0.04), hypertension (29.8% vs 24.5%, p = 0.04), diabetes (16.1% vs 9.8%, p = 0.001), hypogonadism (12.3% vs 8.3%, p = 0.02), prior tobacco use (37.4% vs 30.6%, p = 0.01), history of prostatectomy (5.6% vs 2.8%, p = 0.01), intracavernosal injection use (9.0% vs 5.6%, p = 0.02), less likely to be on oral PD treatment (64.1% vs 81.6%, p < 0.001), previously undergone CCH injections (16.1% vs 6.5%, p < 0.001), less likely to use penile traction therapy (50.4% vs 63.8%, p < 0.001), less likely to have subjective shortening (60.8% vs 67.0%, p = 0.03), less likely to be able to have penetrative sexual intercourse (67.2% vs 79.1%, p < 0.001), diminished/poor elasticity versus normal (61.8% vs 38.2%, p < 0.001), greater mean primary curvature (58.9 ± 19.5° vs 44.5 ± 19.6°, p < 0.001), greater mean secondary curvature (30.1 ± 13.2° vs 25.8 ± 12.0°, p < 0.001), greater composite curvature (69.8 ± 28.7° vs 53.5 ± 27.8°, p < 0.001), greater likelihood of grade 3 calcifications (35.5% grade 3 vs 17.1% grade 1–2, p < 0.001), have an indentation deformity (78.0% vs 71.4%, p = 0.01), have an hourglass deformity (14.7% vs 7.8%, p < 0.001), and have hinge effect (43.9% vs 27.2%, p < 0.001) (Table 4).
On stepwise binary multivariate logistic regression analysis, predictors of surgical intervention increased 1.82-fold with hourglass deformity (95% Confidence Interval (CI) 1.13-2.93, p = 0.01), 2.94-fold with previous CCH injections (95% CI 1.90-4.60, p < 0.001), 1.56-fold with hypogonadism (95% CI 1.02-2.50, p = 0.04), 1.03-fold with greater degree of primary curvature (95% CI 1.02-1.05, p < 0.001), and 1.20-fold with poor elasticity (95% CI 1.02-1.42, p = 0.03). Protective factors against surgical intervention included use of PD oral therapies in three-arm protocol (oral pentoxifylline 400 mg TID with combination amino acid capsule containing- L-arginine, L-citrulline and L-carnitine and daily external penile traction therapy) (95% CI 0.30-0.62, p < 0.001), and maintenance of ability to have penetrative sexual intercourse (95% CI 0.52-0.99, p = 0.046) (Table 5).
Timing of presentation was delayed (>12 months after disease onset) in 52% of patients and was further analyzed on univariate analysis. Those who presented in a delayed fashion, were more likely to have coronary artery disease (7.1% vs 4.0%, p = 0.02), subjective shortening (69.7% vs 59.3%, p < 0.001), greater degree of primary curvature (51.2 ± 20.7° vs 47.9 ± 20.7°, p = 0.01), and greater degree of composite curvature (62.1 ± 28.2° vs 58.5 ± 28.2°, p = 0.03), while less likely to have had a prostatectomy (2.7% vs 5.0%, p = 0.03) (Table 6).
Discussion
Over the last 20 years, much has been learned about PD. It is known now that PD is not purely a penile plaque and curvature problem, but previously, this was the emphasis of most large data cohorts [5, 6, 21,22,23,24]. Our data provide a sizeable modernization to the literature on initial presentation of PD all being evaluated and managed by a single expert in PD. We now add further information on calcification, delays in presentation, hinge effect, indentation/hourglass, shortening, as well as other “atypical” features that are now recognized as increasingly common.
From a presentation standpoint, the earlier, largest single-institution cohort was published over a decade ago including 1001 patients over an 18-year period assessing relationship between degree of curvature and the clinical parameters of patients with PD. Penile deformity without curvature was detected in 12.3% of patients, curvature was < 30° in 39.5%, 30–60° in 34.5% of patients, and >60° in 13.5% of patients [24]. In comparison, our current cohort is much larger at 1263 patients seen over a 5-year period, with 65-year age range of patient presentation, emphasizing that the disease is not isolated to the 5th decade and is widely present. Additionally, in our cohort, there was more severe curvature deformities with primary curvature of 49.8 ± 20.8° and 27.5% > 60° curve. These increasing deformities, led to a 1.03-fold higher rate of surgical intervention, reiterating that, with larger degree of primary curvature, the more likely conservative managements may fail. We found similar rates to previous studies of dorsal plaque location with 77.9% being dorsal, but also acknowledge 11.9% ventral, and 10.2% with circumferential, or distinct plaques on both dorsum and ventral penile locations [23]. Lastly, consistent with prior analysis, we found penile calcifications are not uncommon with it seen in 30% of our patients, and presence of calcification alone did not predict surgery, but grade 3 calcification versus grade 1–2 remained a significant predictor of surgical intervention [14].
Even more recently, the annual percentage of men with PD treated with at least one treatment form increased from 23.3% to 35.4% from 2010 to 2016. During this time, an insurance claims database (2008-2017) identified men 45-54 years old and in southern regions of the USA were more likely to be treated with at least one treatment form. The use of oral medications increased (0.66% to 20.5%), surgical intervention decreased (14.7% to 7.9%), and intralesional injections decreased (84.7% to 71.7%), yet it remains the most used treatment option for men with PD [25]. Also, this study found that just 28% of men with PD were treated on initial presentation. All patients were offered treatment when appropriate in our study, as a result, we found much higher rates of oral PD treatment with 75.4% of our patients using this as part of a trimodal treatment regimen, ultimately leading to a 43% reduction of surgical intervention on multivariate analysis. Our standard protocol utilizes a combination of pentoxifylline 400 mg 3 times a day, an over-the-counter available capsule containing- L-arginine 1,340 mg, L-citrulline 670 mg, and L-carnitine 670 mg, daily external traction therapy, and tadalafil 5 mg daily (if concurrent ED is present) [26]. Our intralesional injection therapy (ILI) rate was much lower with only 21% of patients having undergone ILI and found a 2.94-fold higher rate of surgical intervention in patients who had prior CCH injections. The lower usage rate may be in part patient desire for surgical intervention, and thus seeking out this provider, and possibly patients who had already been deemed not a candidate for ILI with another provider and sought more aggressive treatment in presenting to our clinic.
Prior series reported atypical features (ventral plaques, hourglass deformities, unilateral indentations, severely shortened penile length, and multiplanar curvatures) in 10-39% of patients with PD. More specifically, these atypical features have been reported to occur in patients at rates of 10% with unilateral indentation, 9% with ventral plaques, 1% with hourglass (with 68% of patients with hourglass having concomitant ED) [11, 27]. We found rates of these “atypical” features with ventral plaques present in 11.9%, circumferential or both dorsal and ventral plaques in 10.2%, hourglass deformities in 10.1%, indentation/narrowing in 76.0%, subjective severely shortened penile length in 64.8% at a mean of 3.8 cm reported length loss, and multiplanar curvatures present in 36.5% of patients. Advanced curvature alone (i.e., >60 degrees) for which patients are often referred, is not the only predictor of surgical intervention, as analysis showed hourglass deformities and poor elasticity to be 1.82- and 1.20-fold independent predictors of surgical intervention respectively. The increased rates of these deformities are important for practicing urologists to understand, they are not as atypical or uncommon as previously reported. Additionally, these features if seen in practice can be helpful to refer early to a high-volume PD specialist.
Mean reported duration of PD symptoms prior to presentation was 33.2 ± 42.5 months, emphasizing a large delay with most patients presenting already in the stable phase with a mean duration of stability of 12.5 ± 28.3 months. While this information is self-reported and may be skewed by some patients, it does pertain to an issue of delay in presentation given the overall advanced deformities seen in our cohort with 52% of patients presenting in a delayed fashion. Given the advanced duration of disease, there is concern for inadequate treatment early in the acute phase. Mulhall et al., previously identified patients with delayed presentation to be significantly older (OR = 4.0), in long-term relationships (OR = 3.6), have dorsal curvature (OR = 2.5), have curvature <45° (OR = 3.3), be heterosexual (OR = 2.0), and have simple deformity (OR = 1.5) [28]. We did not find significant differences in age, dorsal curvature or simple versus complex deformity in our patients, unfortunately it appears many patients referring late had more severe curvature, higher rate of shortening, and ultimately a higher rate of surgical intervention.
Our study contains several limitations, including its retrospective single-center nature, although at our center, patients are referred both locally, nationally, and internationally for evaluation. Selection bias may be present as those who are candidates for multimodal conservative therapy are less likely in an advanced state and thus are less likely to be referred to a subspecialist. Additionally, risk of attrition due to patients seeking care for PD from multiple providers makes accurate tracking of outcomes in isolation challenging. Despite these limitations, it is important that all patients were examined by a highly experienced PD expert at baseline and subsequent encounters with rigorous objective assessment of penile deformity making it a uniform cohort for analysis of baseline PD characteristics seen at a tertiary referral center.
Conclusions
This study reviews the largest PD cohort including 1263 patients for presenting features over a 5-year period. PD remains a poorly understood disease but presenting features should not purely focus on curvature, with functional deformities, and “atypical” characteristics being increasingly seen. Ventral curvature, multiplanar curvatures, indentation deformity, hourglass deformity, and severe loss of penile length have been described as “atypical” suggesting they are uncommon. On the contrary, these presentations are common in our contemporary cohort of referred patients. Lastly, referral patterns to tertiary centers and high-volume surgeons are often delayed past the acute phase and more progressive deformities are likely more frequently being seen with advanced curvature and penile shortening. While there is great variation in the pre-, intra-, and post-operative strategies in PD care, awareness of risk factors on presentation such as hourglass deformities, poor elasticity, and advanced degree of primary curvature can help educate patients and providers on the likelihood of eventual operative intervention as well as optimize early treatment for patients.
Data availability
Additional data are available from the corresponding author on request.
References
Al-Thakafi S, Al-Hathal N. Peyronie’s disease: a literature review on epidemiology, genetics, pathophysiology, diagnosis and work-up. Transl Androl Urol. 2016;5:280–9.
Devine CJ Jr., Somers KD, Jordan SG, Schlossberg SM. Proposal: trauma as the cause of the Peyronie’s lesion. J Urol. 1997;157:285–90.
Ziegelmann MJ, Bajic P, Levine LA. Peyronie’s disease: contemporary evaluation and management. Int J Urol. 2020;27:504–16.
Ziegelmann M, Bole R, Avant R, Yang D, Montgomery B, Trost L. Conservatively managed Peyronie’s disease-long-term survey results from patients undergoing nonsurgical and noninjection therapies. Urology. 2018;113:99–104.
Mulhall JP, Schiff J, Guhring P. An analysis of the natural history of Peyronie’s disease. J Urol. 2006;175:2115–8.
Williams JL, Thomas GG. The natural history of Peyronie’s disease. J Urol. 1970;103:75–6.
Ralph D, Gonzalez-Cadavid N, Mirone V, Perovic S, Sohn M, Usta M, et al. The management of Peyronie’s disease: evidence-based 2010 guidelines. J Sex Med. 2010;7:2359–74.
Manka MG, White LA, Yafi FA, Mulhall JP, Levine LA, Ziegelmann MJ. Comparing and contrasting Peyronie’s disease guidelines: points of consensus and deviation. J Sex Med. 2021;18:363–75.
Levine LA, Greenfield JM. Establishing a standardized evaluation of the man with Peyronie’s disease. Int J Impot Res. 2003;15:S103–12.
Pryor JP, Ralph DJ. Clinical presentations of Peyronie’s disease. Int J Impot Res. 2002;14:414–7.
Yafi FA, Hatzichristodoulou G, Delay KJ, Hellstrom WJ. Review of management options for patients with atypical Peyronie’s disease. Sex Med Rev. 2017;5:211–21.
Margolin EJ, Pagano MJ, Aisen CM, Onyeji IC, Stahl PJ. Beyond curvature: prevalence and characteristics of penile volume-loss deformities in men with Peyronie’s disease. Sex Med. 2018;6:309–15.
Ziegelmann MJ, Heslop D, Houlihan M, Bajic P, Helo S, Trost L, et al. The influence of indentation deformity on outcomes with intralesional collagenase clostridium histolyticum monotherapy for Peyronie’s disease. Urology. 2020;139:122–8.
Levine L, Rybak J, Corder C, Farrel MR. Peyronie’s disease plaque calcification–prevalence, time to identification, and development of a new grading classification. J Sex Med. 2013;10:3121–8.
Levine LA, Lenting EL. A surgical algorithm for the treatment of Peyronie’s disease. J Urol. 1997;158:2149–52.
Levine LA, Dimitriou RJ. A surgical algorithm for penile prosthesis placement in men with erectile failure and Peyronie’s disease. Int J Impot Res. 2000;12:147–51.
Nesbit RM. Congenital curvature of the phallus: report of three cases with description of corrective operation. J Urol. 1965;93:230–2.
Levine LA, Estrada CR. Human cadaveric pericardial graft for the surgical correction of Peyronie’s disease. J Urol. 2003;170:2359–62.
Gholami SS, Lue TF. Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol. 2002;167:2066–9.
Wilson SK, Delk JR 2nd. A new treatment for Peyronie’s disease: modeling the penis over an inflatable penile prosthesis. J Urol. 1994;152:1121–3.
Gelbard M, Goldstein I, Hellstrom WJ, McMahon CG, Smith T, Tursi J, et al. Clinical efficacy, safety and tolerability of collagenase clostridium histolyticum for the treatment of Peyronie disease in 2 large double-blind, randomized, placebo controlled phase 3 studies. J Urol. 2013;190:199–207.
Kadioglu A, Tefekli A, Erol B, Oktar T, Tunc M, Tellaloglu S. A retrospective review of 307 men with Peyronie’s disease. J Urol. 2002;168:1075–9.
Perimenis P, Athanasopoulos A, Gyftopoulos K, Katsenis G, Barbalias G. Peyronie’s disease: epidemiology and clinical presentation of 134 cases. Int Urol Nephrol. 2001;32:691–4.
Kadioglu A, Sanli O, Akman T, Canguven O, Aydin M, Akbulut F, et al. Factors affecting the degree of penile deformity in Peyronie disease: an analysis of 1001 patients. J Androl. 2011;32:502–8.
Moghalu OI, Das R, Horns J, Campbell A, Hotaling JM, Pastuszak AW. Trends in treatment of Peyronie’s disease in adult men in the United States from 2008 to 2017-results from an encounter and claims database. Int J Impot Res. 2022;34:280–8.
Valente EG, Vernet D, Ferrini MG, Qian A, Rajfer J, Gonzalez-Cadavid NF. L-arginine and phosphodiesterase (PDE) inhibitors counteract fibrosis in the Peyronie’s fibrotic plaque and related fibroblast cultures. Nitric Oxide. 2003;9:229–44.
Cakan M, Akman T, Oktar T, Gurkan L, Celtik M, Kadioglu A. The clinical characteristics of Peyronie’s patients with notching deformity. J Sex Med. 2007;4:1174–8.
Mulhall JP, Alex B, Choi JM. Predicting delay in presentation in men with Peyronie’s disease. J Sex Med. 2010;7:2226–30.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Study conceptualization was performed by DR, VW, and LL. Methodology, formal data collection, and investigation were performed by DR, VW, AB. Formal data analysis was performed by DR, VW, AB, and LL. Writing of original manuscript draft was performed by DR and AB. Review and editing of subsequent drafts were performed by VW and LL.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Ethical approval
Institutional Review Board approval was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Roadman, D., Wang, V., Beer, A. et al. A contemporary assessment of the evaluation and management of patients presenting to a tertiary medical center with Peyronie’s disease. Int J Impot Res 36, 118–124 (2024). https://doi.org/10.1038/s41443-023-00738-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-023-00738-w
This article is cited by
-
Unveiling treatment horizons and contemporary perspectives in Peyronie’s disease – take home messages from Laurance A. Levine special issue
International Journal of Impotence Research (2024)