Abstract
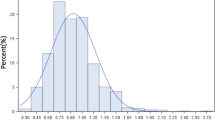
Patient satisfaction after inflatable penile prosthesis (IPP) has been linked to preexisting curvature; however the association with intraoperative asymmetric corporal measurements (ACM) has not been well described. We sought to identify incidence of ACM during IPP surgery, and relationship to penile curvature. A retrospective review of all patients undergoing primary IPP placement between 6/2019 and 6/2021 was performed. Logistic regression analysis was performed to identify factors associated with ACM and need for adjunct straightening techniques. A total of 273 patients underwent primary IPP. 27.8% had Peyronie’s disease (PD) diagnosed preoperatively or detected intraoperatively. ACM was identified in 20.1% (55/273) patients. There was no significant difference in ACM in PD versus non-PD patients (p = 0.55). Most patients with ACM (78.2%, 43/55) underwent placement of asymmetric device. ACM did not predict need for invasive straightening maneuvers (p = 0.12). However ACM patients were significantly more likely to have mild residual curvature than those with symmetry (p < 0.0001). Our study is first to address management of idiopathic ACM and association with curvature, providing new insight into a common situation. While ACM was detected in 20%, it did not predict need for adjunct straightening techniques. Our findings may provide reassurance to urologists troubleshooting idiopathic ACM during corporal dilation during IPP surgery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data available from corresponding author on reasonable request.
References
Govier FE, Gibbons RP, Correa RJ, Pritchett TR, Kramer-Levien D. Mechanical reliability, surgical complications, and patient and partner satisfaction of the modern three-piece inflatable penile prosthesis. Urology. 1998;52:282–6.
Mulhall JP, Ahmed A, Branch J, Parker M. Serial assessment of efficacy and satisfaction profiles following penile prosthesis surgery. J Urol. 2003;169:1429–33.
El-Sakka AI. Prevalence of Peyronie’s disease among patients with erectile dysfunction. Eur Urol. 2006;49:564–9.
Nehra A, Alterowitz R, Culkin DJ, Faraday MM, Hakim LS, Heidelbaugh JJ, et al. Peyronie’s disease: AUA guideline. J Urol. 2015;194:745–53.
Henry GD, Kansal NS, Callaway M, Grigsby T, Henderson J, Noble J, et al. Centers of excellence concept and penile prostheses: an outcome analysis. J Urol. 2009;181:1264–8.
Montorsi F, Rigatti P, Carmignani G, Corbu C, Campo B, Ordesi G, et al. AMS three-piece inflatable implants for erectile dysfunction: a long-term multi-institutional study in 200 consecutive patients. Eur Urol. 2000;37:50–5.
Henry GD, Jennermann C, Eid JF. Evaluation of satisfaction and axial rigidity with Titan XL cylinders. Adv Urol. 2012;2012:896070.
Scherzer ND, Dick B, Gabrielson AT, Alzweri LM, Hellstrom WJG. Penile prosthesis complications: planning, prevention, and decision making. Sex Med Rev. 2019;7:349–59.
Henry GD, Mahle P, Caso J, Eisenhart E, Carrion R, Kramer A. Surgical techniques in penoscrotal implantation of an inflatable penile prosthesis: a guide to increasing patient satisfaction and surgeon ease. Sex Med Rev. 2015;3:36–47.
Chung PH, Scott JF, Morey AF. High patient satisfaction of inflatable penile prosthesis insertion with synchronous penile plication for erectile dysfunction and Peyronie’s disease. J Sex Med. 2014;11:1593–8.
Hatzichristodoulou G, Yang DY, Ring JD, Hebert KJ, Ziegelman MJ, Köhler TS. Multicenter experience using collagen fleece for plaque incision with grafting to correct residual curvature at the time of inflatable penile prosthesis placement in patients with peyronie’s disease. J Sex Med. 2020;17:1168–74.
Tausch TJ, Chung PH, Siegel JA, Gliga L, Klein AK, Morey AF. Intraoperative decision-making for precise penile straightening during inflatable penile prosthesis surgery. Urology. 2015;86:1048–52.
Gupta NK, Ring J, Trost L, Wilson SK, Köhler TS. The penoscrotal surgical approach for inflatable penile prosthesis placement. Transl Androl Urol. 2017;6:628–38.
Agrawal V, Ralph D. An audit of implanted penile prostheses in the UK. BJU Int. 2006;98:393–5.
Oberlin DT, Matulewicz RS, Bachrach L, Hofer MD, Brannigan RE, Flury SC. National practice patterns of treatment of erectile dysfunction with penile prosthesis implantation. J Urol. 2015;193:2040–4.
Lotan Y, Roehrborn CG, McConnell JD, Hendin BN. Factors influencing the outcomes of penile prosthesis surgery at a teaching institution. Urology. 2003;62:918–21.
Akin-Olugbade O, Parker M, Guhring P, Mulhall J. Determinants of patient satisfaction following penile prosthesis surgery. J Sex Med. 2006;3:743–8.
Trost LW, Baum N, Hellstrom WJG. Managing the difficult penile prosthesis patient. J Sex Med. 2013;10:893–906; quiz 907.
Welliver C. Optimizing outcomes in the virgin penile implant patient. Curr Urol Rep. 2019;20:14.
Welliver C, Kottwitz M, Ahmad AE, Wilson SK, Köhler TS. Manufacturers’ data show increasing implanted cylinder sizes and measured corporal lengths in inflatable penile implants. World J Urol. 2016;34:993–8.
Djordjevic ML, Kojovic V. Penile prosthesis implantation and tunica albuginea incision without grafting in the treatment of Peyronie’s disease with erectile dysfunction. Asian J Androl. 2013;15:391–4.
Lucas JW, Gross MS, Barlotta RM, Sudhakar A, Hoover CRV, Wilson SK, et al. Optimal modeling: an updated method for safely and effectively eliminating curvature during penile prosthesis implantation. Urology. 2020;146:133–9.
Deebel NA, Scarberry K, Dutta R, Matz E, Terlecki RP. Salvage penile plication is an effective modality for resolving residual curvature after surgery for peyronie’s disease. Sex Med. 2020;8:686–90.
Berookhim BM, Karpman E, Carrion R. Adjuvant maneuvers for residual curvature correction during penile prosthesis implantation in men with peyronie’s disease. J Sex Med. 2015;12:449–54.
Yachia D, Beyar M, Aridogan IA, Dascalu S. The incidence of congenital penile curvature. J Urol. 1993;1501:1478–9.
Author information
Authors and Affiliations
Contributions
RB, MA, EH, MA, MZ, TK and SH designed the work/acquired data and played an important role in interpreting the results, RB, MA, EH, MA, MZ, TK and SH drafted or revised the manuscript, RB, MA, EH, MA, MZ, TK and SH approved the final version and RB, MA, EH, MA, MZ, TK and SH agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bole, R., Alom, M., Habashy, E. et al. The clinical significance of imperfection: is idiopathic corporal asymmetry related to curvature during penile prosthesis placement?. Int J Impot Res (2023). https://doi.org/10.1038/s41443-023-00669-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-023-00669-6
This article is cited by
-
Commentary on ‘Anatomic considerations of inflatable penile prosthetics: lessons gleaned from surgical body donor workshops’
International Journal of Impotence Research (2023)
-
Response to the Commentary on “Anatomic considerations of inflatable penile prosthetics: lessons gleaned from surgical body donor workshops”
International Journal of Impotence Research (2023)