Abstract
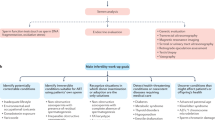
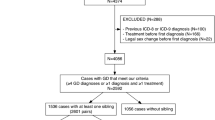
The role of genetics in the etiology of gender dysphoria (GD) is an important yet understudied area. Yet whether genetic analysis should be carried out during the gender affirmation process at all is a matter of debate. This study aims to evaluate the cytogenetic and molecular genetic findings of individuals with GD. We retrospectively reviewed the medical records of individuals with GD who were followed up in a tertiary clinic. After the exclusion criteria were applied, the study sample consisted of 918 individuals with GD; 691 of whom had female-to-male (FtM) and 227 male-to-female (MtF) GD. The cytogenetic analysis revealed that 223 out of 227 (98.2%) individuals with MtF GD had the 46,XY karyotype, while 683 out of 691 (98.8%) individuals with FtM GD had the 46,XX karyotype. In the Y chromosome microdeletion analysis, azospermic factor c (AZFc) deletion was detected in only two individuals with MtF GD. Our findings suggest that there are few chromosomal abnormalities in individuals with GD. Thus, this research calls into question both the role of chromosomal abnormalities in GD etiology and why the application of chromosomal analysis is in Turkey a routine part of the baseline evaluation of GD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Data are available upon request due to restrictions privacy or ethics. The data presented in this study are available on request from the corresponding author.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. American Psychiatric Association; 2013. https://doi.org/10.1176/appi.books.9780890425596.
Arcelus J, Bouman WP, Van Den Noortgate W, Claes L, Witcomb G, Fernandez-Aranda F. Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry. 2015;30:807–15. https://doi.org/10.1016/j.eurpsy.2015.04.005.
Collin L, Reisner SL, Tangpricha V, Goodman M. Prevalence of transgender depends on the “case” definition: a systematic review. J Sex Med. 2016;13:613–26. https://doi.org/10.1016/j.jsxm.2016.02.001.
Roselli CE. Neurobiology of gender identity and sexual orientation. J Neuroendocrinol. 2018;30:e12562. https://doi.org/10.1111/jne.12562.
Smith ES, Junger J, Derntl B, Habel U. The transsexual brain–a review of findings on the neural basis of transsexualism. Neurosci Biobehav Rev. 2015;59:251–66. https://doi.org/10.1016/j.neubiorev.2015.09.008.
Mueller SC, Guillamon A, Zubiaurre-Elorza L, Junque C, Gomez-Gil E, Uribe C, et al. The neuroanatomy of transgender identity: mega-analytic findings from the ENIGMA transgender persons working group. J Sex Med. 2021;18:1122–9. https://doi.org/10.1016/j.jsxm.2021.03.079.
Foreman M, Hare L, York K, Balakrishnan K, Sánchez FJ, Harte F, et al. Genetic link between gender dysphoria and sex hormone signaling. J Clin Endocrinol Metab. 2019;104:390–6. https://doi.org/10.1210/jc.2018-01105.
Polderman TJC, Kreukels BPC, Irwig MS, Beach L, Chan Y-M, Derks EM, et al. The biological contributions to gender identity and gender diversity: bringing data to the table. Behav Genet. 2018;48:95–108. https://doi.org/10.1007/s10519-018-9889-z.
Gómez-Gil E, Esteva I, Almaraz MC, Pasaro E, Segovia S, Guillamon A. Familiality of gender identity disorder in non-twin siblings. Arch Sex Behav. 2010;39:546–52. https://doi.org/10.1007/s10508-009-9524-4.
Heylens G, De Cuypere G, Zucker KJ, Schelfaut C, Elaut E, Vanden Bossche H, et al. Gender identity disorder in twins: a review of the case report literature. J Sex Med. 2012;9:751–7. https://doi.org/10.1111/j.1743-6109.2011.02567.x.
Bao A-M, Swaab DF. Sexual differentiation of the human brain: Relation to gender identity, sexual orientation and neuropsychiatric disorders. Front Neuroendocrinol. 2011;32:214–26. https://doi.org/10.1016/j.yfrne.2011.02.007.
Savic I, Garcia-Falgueras A, Swaab DF. Sexual differentiation of the human brain in relation to gender identity and sexual orientation. Prog Brain Res. 2010;186:41–62. https://doi.org/10.1016/B978-0-444-53630-3.00004-X.
Turan Ş, Boysan M, Tarakçıoğlu MC, Sağlam T, Yassa A, Bakay H, et al. 2D:4D digit ratios in adults with gender dysphoria: a comparison to their unaffected same-sex heterosexual siblings, cisgender heterosexual men, and cisgender heterosexual women. Arch Sex Behav. 2021;50:885–95. https://doi.org/10.1007/s10508-021-01938-5.
Zucker KJ, Lawrence AA, Kreukels BPC. Gender dysphoria in adults. Annu Rev Clin Psychol. 2016;12:217–47. https://doi.org/10.1146/annurev-clinpsy-021815-093034.
Coolidge FL, Thede LL, Young SE. The heritability of gender identity disorder in a child and adolescent twin sample. Behav Genet. 2002;32:251–7. https://doi.org/10.1023/a:1019724712983.
Ujike H, Otani K, Nakatsuka M, Ishii K, Sasaki A, Oishi T, et al. Association study of gender identity disorder and sex hormone-related genes. Prog Neuro Psychopharmacol Biol Psychiatry. 2009;33:1241–4. https://doi.org/10.1016/j.pnpbp.2009.07.008.
Fernández R, Guillamon A, Cortés-Cortés J, Gómez-Gil E, Jácome A, Esteva I, et al. Molecular basis of Gender Dysphoria: androgen and estrogen receptor interaction. Psychoneuroendocrinology. 2018;98:161–7. https://doi.org/10.1016/j.psyneuen.2018.07.032.
Fernández R, Ramírez K, Gómez-Gil E, Cortés-Cortés J, Mora M, Aranda G, et al. Gender-affirming hormone therapy modifies the CpG methylation pattern of the ESR1 gene promoter after six months of treatment in transmen. J Sex Med. 2020;17:1795–806. https://doi.org/10.1016/j.jsxm.2020.05.027.
Fernandez R, Collet S, Ramirez K, Kiyar M, Delgado-Zayas E, Guy T, et al. The (epi)genetic basis of gender incongruence. Endocr Abstr. 2021. https://doi.org/10.1530/endoabs.73.AEP451.
Swaab DF, Wolff SEC, Bao A-M. Sexual differentiation of the human hypothalamus: relationship to gender identity and sexual orientation. Handb Clin Neurol. 2021;181:427–43. https://doi.org/10.1016/B978-0-12-820683-6.00031-2.
Hare L, Bernard P, Sánchez FJ, Baird PN, Vilain E, Kennedy T, et al. Androgen receptor repeat length polymorphism associated with male-to-female transsexualism. Biol Psychiatry. 2009;65:93–96. https://doi.org/10.1016/j.biopsych.2008.08.033.
Fernández R, Esteva I, Gómez-Gil E, Rumbo T, Almaraz MC, Roda E, et al. Association study of ERβ, AR, and CYP19A1 genes and MtF transsexualism. J Sex Med. 2014;11:2986–4. https://doi.org/10.1111/jsm.12673.
Cortés-Cortés J, Fernández R, Teijeiro N, Gómez-Gil E, Esteva I, Almaraz MC, et al. Genotypes and haplotypes of the estrogen receptor α gene (ESR1) are associated with female-to-male gender dysphoria. J Sex Med. 2017;14:464–72. https://doi.org/10.1016/j.jsxm.2016.12.234.
Fernández R, Esteva I, Gómez‐Gil E, Rumbo T, Almaraz MC, Roda E, et al. The (CA)n polymorphism of ERβ gene is associated with FtM transsexualism. J Sex Med. 2014;11:720–8. https://doi.org/10.1111/jsm.12398.
Fernández R, Delgado-Zayas E, Ramírez K, Cortés-Cortés J, Gómez-Gil E, Esteva I, et al. Analysis of four polymorphisms located at the promoter of the estrogen receptor alpha ESR1 gene in a population with gender incongruence. Sex Med. 2020;8:490–500. https://doi.org/10.1016/j.esxm.2020.04.002.
Karasic DH, Fraser L. Multidisciplinary care and the standards of care for transgender and gender nonconforming individuals. Clin Plast Surg. 2018;45:295–9.https://doi.org/10.1016/j.cps.2018.03.016.
Auer MK, Fuss J, Stalla GK, Athanasoulia AP. Twenty years of endocrinologic treatment in transsexualism: analyzing the role of chromosomal analysis and hormonal profiling in the diagnostic work-up. Fertil Steril. 2013;100:1103–10. https://doi.org/10.1016/j.fertnstert.2013.05.047.
Lee PA, Houk CP, Ahmed SF, Hughes IA. Consensus statement on management of intersex disorders. Pediatrics. 2006;118:e488–e500. https://doi.org/10.1542/peds.2006-0738.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th ed. Text Revision. Washington, DC: American Psychiatric Association; 2000.
World Health Organization. The ICD-10 classification of mental and behavioral disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
Bağcaz A, Boduroğlu OK, Başar K. Chromosome analysis in the assessment for gender affirmation process: a retrospective study. Turk Psikiyatr Derg. 2019;30:157–62.
Inoubli A, De Cuypere G, Rubens R, Heylens G, Elaut E, Van Caenegem E, et al. Karyotyping, is it worthwhile in transsexualism? J Sex Med. 2011;8:475–8. https://doi.org/10.1111/j.1743-6109.2010.02130.x.
Vujovic S, Popovic S, Sbutega-Milosevic G, Djordjevic M, Gooren L. Transsexualism in Serbia: a twenty-year follow-up study. J Sex Med. 2009;6:1018–23. https://doi.org/10.1111/j.1743-6109.2008.00799.x.
Hengstschläger M, van Trotsenburg M, Repa C, Marton E, Huber JC, Bernaschek G. Sex chromosome aberrations and transsexualism. Fertil Steril. 2003;79:639–40. https://doi.org/10.1016/s0015-0282(02)04805-7.
Fernández R, Guillamón A, Gómez-Gil E, Esteva I, Almaraz MC, Cortés-Cortés J, et al. Analyses of karyotype by G-banding and high-resolution microarrays in a gender dysphoria population. Genes Genomics. 2018;40:465–73. https://doi.org/10.1007/s13258-017-0646-0.
Wylie KR, Steward D. A consecutive series of 52 transsexual people presenting for assessment and chromosomal analysis at a gender identity clinic. Int J Transgenderism. 2008;10:147–8.
Pang KC, Feldman D, Oertel R, Telfer M. Molecular karyotyping in children and adolescents with gender dysphoria. Transgender Health. 2018;3:147–53.
Bearman G. Karyotyping and genetics in the transgendered population. In: Ettner R, Monstrey S, Eyler AE, editors. Principles of transgender medicine and surgery. Binghamton: The Haworth Press; 2007. p. 223–32.
Bosman FT, Schaberg A. A new G-banding modification for metaphase chromosomes. Nat N Biol. 1973;241:216–7. https://doi.org/10.1038/newbio241216a0.
Wenz HM. Capillary electrophoresis as a technique to analyze sequence-induced anomalously migrating DNA fragments. Nucleic Acids Res. 1994;22:4002–8. https://doi.org/10.1093/nar/22.19.4002.
Turan Ş, Aksoy Poyraz C, İnce E, Sakalli Kani̇ A, Emül HM, Duran A. Sociodemographic and clinical characteristics of transsexual individuals who presented to a psychiatry clinic for sex reassignment surgery. Turkish J Psychiatry. 2015;26:153–60.
Aranda G, Fernández-Rebollo E, Pradas-Juni M, Hanzu FA, Kalko SG, Halperin I, et al. Effects of sex steroids on the pattern of methylation and expression of the promoter region of estrogen and androgen receptors in people with gender dysphoria under cross-sex hormone treatment. J Steroid Biochem Mol Biol. 2017;172:20–28. https://doi.org/10.1016/j.jsbmb.2017.05.010.
Egozcue S, Blanco J, Vendrell JM, García F, Veiga A, Aran B, et al. Human male infertility: chromosome anomalies, meiotic disorders, abnormal spermatozoa and recurrent abortion. Hum Reprod Update. 2000;6:93–105. https://doi.org/10.1093/humupd/6.1.93.
Scriven PN, Flinter FA, Braude PR, Ogilvie CM. Robertsonian translocations–reproductive risks and indications for preimplantation genetic diagnosis. Hum Reprod. 2001;16:2267–73. https://doi.org/10.1093/humrep/16.11.2267.
Choi BH, Kim UH, Lee KS, Ko CW. Various endocrine disorders in children with t(13;14)(q10;q10) Robertsonian translocation. Ann Pediatr Endocrinol Metab. 2013;18:111. https://doi.org/10.6065/apem.2013.18.3.111.
Riehn M, Klopocki E, Molkentin M, Reinhardt R, Burmeister T. A BACH2-BCL2L1 fusion gene resulting from a lymphoma cell line BLUE-1. Cancer. 2011;396:389–96. https://doi.org/10.1002/gcc.20863.
Huret J. T(3;18)(Q26;Q11). Atlas Genet Cytogenet Oncol Haematol. 2011;12:2008.
Matsumoto AM, Bremner WJ. Testicular disorders. In: Williams textbook of endocrinology. Elsevier; 2016, pp 694–784.
Lombardo F, Toselli L, Grassetti D, Paoli D, Masciandaro P, Valentini F, et al. Hormone and genetic study inmale to female transsexual patients. J Endocrinol Invest. 2013;36:550–7. https://doi.org/10.3275/8813.
Acknowledgements
We thank Dr. Deniz Agirbasli for her support. No financial disclosure was received.
Author information
Authors and Affiliations
Contributions
AKY, ST, and MS were responsible for designing the review protocol, writing the protocol and report, interpreting results, and updating the reference lists. MTA, YK, and OD were responsible for extracting and analyzing the data, interpreting the results and providing feedback on the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and conformed to the ethical standards of the Helsinki Declaration.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kalaycı Yigin, A., Turan, Ş., Alay, M.T. et al. Should chromosomal analysis be performed routinely during the baseline evaluation of the gender affirmation process? The outcomes of a large cohort of gender dysphoric individuals. Int J Impot Res 35, 472–477 (2023). https://doi.org/10.1038/s41443-022-00582-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-022-00582-4