Abstract
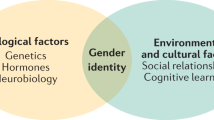
Gender dysphoria (GD) in children and adolescents is a condition that is characterized by an incongruence between the assigned and experienced gender. Despite the diversity in clinical presentation, literature demonstrates that GD might lead to poor mental health and high rates of co-occurring psychopathology. Due to the overlap of physical aspects as well as psychological needs in these children, a multidisciplinary approach is highly desirable. The aim of this narrative review is to give an overview of recent literature on several topics relevant in this domain. Guidelines on psychological counseling and hormonal treatment are given and challenging topics subject to controversy are explained. Furthermore, attention is drawn to the risks and protective factors in psychological functioning, including the growing evidence of a frequent co-occurrence with Autism Spectrum Disorder. Finally the psycho-sexual development in these children, the impact on fertility and fertility preservation are discussed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Alberse AE, de Vries AL, Elzinga WS, Steensma TD. Self-perception of transgender clinic referred gender diverse children and adolescents. Clin Child Psychol Psychiatry. 2019;24:388–401.
Association AP. Diagnostic and statistical manual of mental disorders (5th ed.). 2013.
Beek TF, Cohen-Kettenis PT, Bouman WP, de Vries AL, Steensma TD, Witcomb GL, et al. Gender incongruence of childhood: clinical utility and stakeholder agreement with the World Health Organization’s proposed ICD-11 criteria. PLoS ONE 2017;12:e0168522.
Steensma TD, Cohen-Kettenis PT, Zucker KJ. Evidence for a change in the sex ratio of children referred for gender dysphoria: data from the center of expertise on gender dysphoria in Amsterdam (1988-2016). J Sex Marital Ther. 2018;44:713–5.
Aitken M, Steensma TD, Blanchard R, VanderLaan DP, Wood H, Fuentes A, et al. Evidence for an altered sex ratio in clinic-referred adolescents with gender dysphoria. J Sex Med. 2015;12:756–63.
de Graaf NM, Carmichael P, Steensma TD, Zucker KJ. Evidence for a change in the sex ratio of children referred for gender dysphoria: data from the gender identity development service in London (2000–2017). J Sex Med. 2018;15:1381–3.
Hsieh S, Leininger J. Resource list: clinical care programs for gender-nonconforming children and adolescents. Pediatr Ann 2014;43:238–44.
Kaltiala-Heino R, Sumia M, Tyolajarvi M, Lindberg N. Two years of gender identity service for minors: overrepresentation of natal girls with severe problems in adolescent development. Child Adolesc Psychiatry Ment Health. 2015;9:9.
Khatchadourian K, Amed S, Metzger DL. Clinical management of youth with gender dysphoria in Vancouver. J Pediatr 2014;164:906–11.
Spack NP, Edwards-Leeper L, Feldman HA, Leibowitz S, Mandel F, Diamond DA, et al. Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics 2012;129:418–25.
Rosenthal SM. Approach to the patient: transgender youth: endocrine considerations. J Clin Endocrinol Metab. 2014;99:4379–89.
Sherer I, Rosenthal SM, Ehrensaft D, Baum J. Child and Adolescent Gender Center: a multidisciplinary collaboration to improve the lives of gender nonconforming children and teens. Pediatr Rev 2012;33:273–5.
de Vries AL, Cohen-Kettenis PT. Clinical management of gender dysphoria in children and adolescents: the Dutch approach. J Homosex. 2012;59:301–20.
Zucker KJ, Bradley SJ, Owen-Anderson A, Kibblewhite SJ, Cantor JM. Is gender identity disorder in adolescents coming out of the closet? J Sex Marital Ther. 2008;34:287–90.
Byne W, Bradley SJ, Coleman E, Eyler AE, Green R, Menvielle EJ, et al. Report of the American Psychiatric Association Task Force on treatment of gender identity disorder. Arch Sex Behav. 2012;41:759–96.
Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, Version 7. Int J Transgenderism. 2012;13:165–232.
Adelson SL. Practice parameter on gay, lesbian, or bisexual sexual orientation, gender nonconformity, and gender discordance in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2012;51:957–74.
Obedin-Maliver J, Goldsmith ES, Stewart L, White W, Tran E, Brenman S, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA 2011;306:971–7.
Association A. Guidelines for psychological practice with transgender and gender nonconforming people. Am Psychologist 2015;70:832–64.
Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society clinical practice guideline. Endocr Pract 2017;23:1437.
de Vries AL, McGuire JK, Steensma TD, Wagenaar EC, Doreleijers TA, Cohen-Kettenis PT. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics 2014;134:696–704.
Drescher J. Controversies in gender diagnoses. LGBT Health. 2014;1:10–4.
Steensma TD, Biemond R, de Boer F, Cohen-Kettenis PT. Desisting and persisting gender dysphoria after childhood: a qualitative follow-up study. Clin Child Psychol Psychiatry. 2011;16:499–516.
Cohen-Kettenis PT, van Goozen SH. Pubertal delay as an aid in diagnosis and treatment of a transsexual adolescent. Eur Child Adolesc Psychiatry. 1998;7:246–8.
Delamarre-van der Waal H, Cohen-Kettenis P. Clinical management of gender identity disorder in adolescents: a protocol on psychological and paediatric endocrinology aspects. Eur J Endocrinol. 2006;155:131–7.
Boepple PA, Mansfield MJ, Wierman ME, Rudlin CR, Bode HH, Crigler JF Jr., et al. Use of a potent, long acting agonist of gonadotropin-releasing hormone in the treatment of precocious puberty. Endocr Rev 1986;7:24–33.
Tack LJ, Craen M, Dhondt K, Vanden Bossche H, Laridaen J, Cools M. Consecutive lynestrenol and cross-sex hormone treatment in biological female adolescents with gender dysphoria: a retrospective analysis. Biol Sex Differ. 2016;7:14.
Tack LJW, Craen M, Lapauw B, Goemaere S, Toye K, Kaufman JM, et al. Proandrogenic and antiandrogenic progestins in transgender youth: differential effects on body composition and bone metabolism. J Clin Endocrinol Metab. 2018;103:2147–56.
Klink D, Caris M, Heijboer A, van Trotsenburg M, Rotteveel J. Bone mass in young adulthood following gonadotropin-releasing hormone analog treatment and cross-sex hormone treatment in adolescents with gender dysphoria. J Clin Endocrinol Metab. 2015;100:E270–5.
Kreukels BP, Guillamon A. Neuroimaging studies in people with gender incongruence. Int Rev Psychiatry. 2016;28:120–8.
Hulshoff Pol H, Cohen-Kettenis P, Haren NEM, Peper J, Brans R, Cahn W, et al. Changing your sex changes your brain: Influences of testosterone and estrogen on adult human brain structure. Eur J Endocrinol. 2006;155:107–14.
Zubiaurre-Elorza L, Junque C, Gomez-Gil E, Segovia S, Carrillo B, Rametti G, et al. Cortical thickness in untreated transsexuals. Cereb Cortex. 2013;23:2855–62.
Rametti G, Carrillo B, Gomez-Gil E, Junque C, Zubiaurre-Elorza L, Segovia S, et al. Effects of androgenization on the white matter microstructure of female-to-male transsexuals. A diffusion tensor imaging study. Psychoneuroendocrinology. 2012;37:1261–9.
Jarin J, Pine-Twaddell E, Trotman G, Stevens J, Conard LA, Tefera E, et al. Cross-sex hormones and metabolic parameters in adolescents with gender dysphoria. Pediatrics. 2017;139:e20163173. https://doi.org/10.1542/peds.2016-3173.
Iwamoto SJ, Defreyne J, Rothman MS, Van Schuylenbergh J, Van de Bruaene L, Motmans J, et al. Health considerations for transgender women and remaining unknowns: a narrative review. Ther Adv Endocrinol Metab. 2019;10:2042018819871166.
Defreyne J, Van de Bruaene LDL, Rietzschel E, Van Schuylenbergh J, T’Sjoen GGR. Effects of gender-affirming hormones on lipid, metabolic, and cardiac surrogate blood markers in transgender persons. Clin Chem. 2019;65:119–34.
Ikeda K, Baba T, Noguchi H, Nagasawa K, Endo T, Kiya T, et al. Excessive androgen exposure in female-to-male transsexual persons of reproductive age induces hyperplasia of the ovarian cortex and stroma but not polycystic ovary morphology. Hum Reprod. 2013;28:453–61.
Baba T, Endo T, Honnma H, Kitajima Y, Hayashi T, Ikeda H, et al. Association between polycystic ovary syndrome and female-to-male transsexuality. Hum Reprod. 2007;22:1011–6.
De Roo C, Tilleman K, Vercruysse C, Declercq H, T’Sjoen G, Weyers S, et al. Texture profile analysis reveals a stiffer ovarian cortex after testosterone therapy: a pilot study. J Assist Reprod Genet. 2019;36:1837–43.
de Vries ALC, Steensma TD, Doreleijers TAH, Cohen-Kettenis PT. Puberty suppression in adolescents with gender identity disorder: a prospective follow-up study. J Sex Med. 2011;8:2276–83.
Steensma TD, Zucker KJ, Kreukels BPC, Vanderlaan DP, Wood H, Fuentes A, et al. Behavioral and emotional problems on the Teacher’s Report Form: a cross-national, cross-clinic comparative analysis of gender dysphoric children and adolescents. J Abnorm Child Psychol. 2014;42:635–47.
Cohen-Kettenis PT, Owen A, Kaijser VG, Bradley SJ, Zucker KJ. Demographic characteristics, social competence, and behavior problems in children with gender identity disorder: a cross-national, cross-clinic comparative analysis. J Abnorm Child Psychol. 2003;31:41–53.
de Vries ALC, Doreleijers TAH, Steensma TD, Cohen-Kettenis PT. Psychiatric comorbidity in gender dysphoric adolescents. J Child Psychol Psychiatry. 2011;52:1195–202.
Wallien MSC, Swaab H, Cohen-Kettenis PT. Psychiatric comorbidity among children with gender identity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:1307–14.
Veale JF, Watson RJ, Peter T, Saewyc EM. Mental health disparities among Canadian transgender youth. J Adolesc Health. 2017;60:44–9.
Reisner SL, Vetters R, Leclerc M, Zaslow S, Wolfrum S, Shumer D, et al. Mental health of transgender youth in care at an adolescent urban community health center: a matched retrospective cohort study. J Adolesc Health. 2015;56:274–9.
Carter B, McCloskey L A. LM. Peers and the maintenance of sex-typed behavior: the development of children’s conceptions of cross-gender behavior in their peers. Soc Cogn. 1984;2:294–314.
Levy GD, Taylor MG, Gelman SA. Traditional and evaluative aspects of flexibility in gender roles, social conventions, moral rules, and physical laws. Child Dev. 1995;66:515–31.
Liben LS, Signorella ML. Gender-schematic processing in children: the role of initial interpretations of stimuli. Dev Psychol. 1993;29:141–9.
Stoddart T, Turiel E. Children’s concepts of cross-gender activities. Blackwell Publishing; 1985. p. 1241–52.
de Vries AL, Steensma TD, Cohen-Kettenis PT, VanderLaan DP, Zucker KJ. Poor peer relations predict parent- and self-reported behavioral and emotional problems of adolescents with gender dysphoria: a cross-national, cross-clinic comparative analysis. Eur Child Adolesc Psychiatry. 2016;25:579–88.
de Graaf NM, Cohen-Kettenis PT, Carmichael P, de Vries ALC, Dhondt K, Laridaen J, et al. Psychological functioning in adolescents referred to specialist gender identity clinics across Europe: a clinical comparison study between four clinics. Eur Child Adolesc Psychiatry. 2018;27:909–19.
de Vries AL, Noens IL, Cohen-Kettenis PT, van Berckelaer-Onnes IA, Doreleijers TA. Autism spectrum disorders in gender dysphoric children and adolescents. J Autism Dev Disord. 2010;40:930–6.
Skagerberg E, Di Ceglie D, Carmichael P. Brief report: autistic features in children and adolescents with gender dysphoria. J Autism Dev Disord. 2015;45:2628–32.
Strang JF, Kenworthy L, Dominska A, Sokoloff J, Kenealy LE, Berl M, et al. Increased gender variance in autism spectrum disorders and attention deficit hyperactivity disorder. Arch Sex Behav. 2014;43:1525–33.
Janssen A, Huang H, Duncan C. Gender variance among youth with autism spectrum disorders: a retrospective chart review. Transgend Health 2016;1:63–8.
May T, Pang K, Williams KJ. Gender variance in children and adolescents with autism spectrum disorder from the National Database for Autism Research. Int J Transgenderism. 2017;18:7–15.
van der Miesen AIR, de Vries ALC, Steensma TD, Hartman CA. Autistic symptoms in children and adolescents with gender dysphoria. J Autism Dev Disord. 2018;48:1537–48.
Nabbijohn AN, van der Miesen AIR, Santarossa A, Peragine D, de Vries ALC, Popma A, et al. Gender variance and the autism spectrum: an examination of children ages 6-12 years. J Autism Dev Disord. 2019;49:1570–85.
Turban JL, van Schalkwyk GI. “Gender Dysphoria” and autism spectrum disorder: is the link real? J Am Acad Child Adolesc Psychiatry. 2018;57:8–9.e2.
van der Miesen AIR, Cohen-Kettenis PT, de Vries ALC. Is there a link between gender dysphoria and autism spectrum disorder? J Am Acad Child Adolesc Psychiatry. 2018;57:884–5.
Strang JF, Janssen A, Tishelman A, Leibowitz SF, Kenworthy L, McGuire JK, et al. Revisiting the link: evidence of the rates of autism in studies of gender diverse individuals. J Am Acad Child Adolesc Psychiatry. 2018;57:885–7.
Baron-Cohen S. The extreme male brain theory of autism. Trends Cogn Sci. 2002;6:248–54.
Parkinson J. Gender dysphoria in Asperger’s syndrome: a caution. Australas Psychiatry 2014;22:84–5.
Strang JF, Meagher H, Kenworthy L, de Vries ALC, Menvielle E, Leibowitz S, et al. Initial clinical guidelines for co-occurring autism spectrum disorder and gender dysphoria or incongruence in adolescents. J Clin Child Adolesc Psychol. 2018;47:105–15.
Pache TD, Chadha S, Gooren LJ, Hop WC, Jaarsma KW, Dommerholt HB, et al. Ovarian morphology in long-term androgen-treated female to male transsexuals. A human model for the study of polycystic ovarian syndrome? Histopathology 1991;19:445–52.
Schulze C. Response of the human testis to long-term estrogen treatment: morphology of Sertoli cells, Leydig cells and spermatogonial stem cells. Cell Tissue Res. 1988;251:31–43.
Finlayson C, Johnson EK, Chen D, Dabrowski E, Gosiengfiao Y, Campo-Engelstein L, et al. Proceedings of the working group session on fertility preservation for individuals with gender and sex diversity. Transgend Health 2016;1:99–107.
Johnson EK, Finlayson C. Preservation of fertility potential for gender and sex diverse individuals. Transgend Health 2016;1:41–4.
Hagen CP, Sorensen K, Anderson RA, Juul A. Serum levels of antimullerian hormone in early maturing girls before, during, and after suppression with GnRH agonist. Fertil Steril 2012;98:1326–30.
Grynberg M, Fanchin R, Dubost G, Colau JC, Bremont-Weil C, Frydman R, et al. Histology of genital tract and breast tissue after long-term testosterone administration in a female-to-male transsexual population. Reprod Biomed Online. 2010;20:553–8.
De Roo C, Lierman S, Tilleman K, Peynshaert K, Braeckmans K, Caanen M, et al. Ovarian tissue cryopreservation in female-to-male transgender people: insights into ovarian histology and physiology after prolonged androgen treatment. Reprod Biomed Online. 2017;34:557–66.
Kent MA, Winoker JS, Grotas AB. Effects of feminizing hormones on sperm production and malignant changes: microscopic examination of post orchiectomy specimens in transwomen. Urology 2018;121:93–6.
Schneider F, Kliesch S, Schlatt S, Neuhaus N. Andrology of male-to-female transsexuals: influence of cross-sex hormone therapy on testicular function. Andrology. 2017;5:873–80.
Wyns C, Curaba M, Vanabelle B, Van Langendonckt A, Donnez J. Options for fertility preservation in prepubertal boys. Hum Reprod Update. 2010;16:312–28.
Donnez J, Dolmans MM. Ovarian cortex transplantation: 60 reported live births brings the success and worldwide expansion of the technique towards routine clinical practice. J Assist Reprod Genet. 2015;32:1167–70.
Chen D, Simons L, Johnson EK, Lockart BA, Finlayson C. Fertility preservation for transgender adolescents. J Adolesc Health. 2017;61:120–3.
Nahata L, Tishelman AC, Caltabellotta NM, Quinn GP. Low fertility preservation utilization among transgender youth. J Adolesc Health. 2017;61:40–4.
Sutter P, Kira K, Verschoor A, Hotimsky A. The desire to have children and the preservation of fertility in transsexual women: A survey. Int J Transgend. 2002;6:215–21.
Wierckx K, Van Caenegem E, Pennings G, Elaut E, Dedecker D, Van de Peer F, et al. Reproductive wish in transsexual men. Hum Reprod 2012;27:483–7.
Strang JF, Jarin J, Call D, Clark B, Wallace GL, Anthony LG, et al. Transgender youth fertility attitudes questionnaire: measure development in nonautistic and autistic transgender youth and their parents. J Adolesc Health. 2018;62:128–35.
Wenzel L, Dogan-Ates A, Habbal R, Berkowitz R, Goldstein DP, Bernstein M, et al. Defining and measuring reproductive concerns of female cancer survivors. J Natl Cancer Inst Monogr. 2005;34:94–8.
Quinn GP, Murphy D, Wang H, Sawczyn KK, Knapp C. Having cancer does not change wanting a baby: healthy adolescent girls’ perceptions of cancer-related infertility. J Adolesc Health. 2013;52:164–9.
Meneses K, McNees P, Azuero A, Jukkala A. Development of the fertility and cancer project: an internet approach to help young cancer survivors. Oncol Nurs Forum. 2010;37:191–7.
Bungener SL, Steensma TD, Cohen-Kettenis PT, de Vries ALC. Sexual and romantic experiences of transgender youth before gender-affirmative treatment. Pediatrics. 2017;139:e20162283. https://doi.org/10.1542/peds.2016-2283.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baetens, L., Dhondt, K. Psychosocial challenges and hormonal treatment in gender diverse children and adolescents. A narrative review. Int J Impot Res 33, 217–227 (2021). https://doi.org/10.1038/s41443-020-0291-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-0291-z
This article is cited by
-
The role of the pediatrician in the management of the child and adolescent with gender dysphoria
Italian Journal of Pediatrics (2023)
-
Out of the dark, into the light: sexuality and fertility in pediatric urological conditions
International Journal of Impotence Research (2021)