Abstract
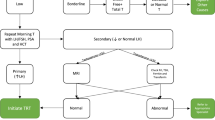
A subcutaneous testosterone enanthate-autoinjector (SCTE-AI) was recently approved by the Food and Drug Administration for patient-administered weekly testosterone replacement therapy (TRT). From January 2019 to October 2019, 110 hypogonadal men were treated with SCTE-AI at two institutions. Patients were assessed in a pretherapy visit prior to receiving SCTE-AI and re-assessed 6 weeks after treatment initiation. Patients with a history of prostate cancer were excluded. Trough serum total testosterone (TT), estradiol (E2), prostate-specific antigen (PSA), and hematocrit (HCT) levels were collected at clinic visits. Therapeutic phlebotomy was recommended for HCT > 54%, and treatment was discontinued for significant increases in PSA as well as for significant treatment-related adverse events. Values from each visit were compared with univariate analysis. 110 patients completed the 6 weeks of observation with a mean age of 40.3 (SD: 10.5). TT significantly rose from 246.6 ng/dL (SD:113.3) pretherapy to 538.4 ng/dL (SD: 209.3) at 6 weeks (p < 0.001). Post-therapy, 101/110 (91.8%) of patients had TT > 300 ng/dL. No patients had HCT > 54%. 74 patients (70.5%) had PSA increase with only 3 (2.9%) experiencing an increase >1.0 ng/dL. There was a significant increase in mean PSA from 1.07 ng/dL (SD: 0.8) pretherapy to 1.18 ng/dL (SD: 0.9) at 6 weeks (p = 0.01). One patient had immediate treatment cessation following diagnosis of prostate cancer. This is the largest non-industry sponsored safety and efficacy profile of SCTE-AI application in urology clinics. After 6 weeks of observation, TT levels increased significantly without any reports of adverse events. SCTE-AI is a safe and effective alternative delivery system of TRT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Zitzmann M, Nieschlag E. Hormone substitution in male hypogonadism. Mol Cell Endocrinol. 2000;161:73–88.
Kalyani RR, Gavini S, Dobs AS. Male Hypogonadism in Systemic Disease. Endocrinol Metab Clin North Am. 2007;36):333–48.
Muller M, Grobbee DE, den Tonkelaar I, Lamberts SWJ, van der Schouw YT. Endogenous sex hormones and metabolic syndrome in aging men. J Clin Endocrinol Metab. 2005;90:2618–23.
Kupelian V, Page ST, Araujo AB, Travison TG, Bremner WJ, McKinlay JB. Low sex hormone-binding globulin, total testosterone, and symptomatic androgen deficiency are associated with development of the metabolic syndrome in nonobese men. J Clin Endocrinol Metab. 2006;91:843–50.
Mulhall JP, Trost LW, Brannigan RE, Kurtz EG, Redmon JB, Chiles KA, et al. Evaluation and management of testosterone deficiency: AUA guideline. J Urol. 2018;200:423–32.
Dohle G, Arver S, Bettocchi C, Jones T, Kliesch S, Punab M. EAU guidelines on male hypogonadism. In Arnhem: The Netherlands: uropean Association of Urology; 2016.
Sexual Medicine Society of North America (SMSNA). Consensus Statement and White Paper Executive Summary: Adult Onset Hypogonadism (AOH). 2015.
Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, Matsumoto AM, et al. Testosterone therapy in men with hypogonadism: an endocrine Society* clinical practice guideline. J Clin Endocrinol Metab. 2018;103:1715–44.
Feldman HA, Longcope C, Derby CA, Johannes CB, Araujo AB, Coviello AD, et al. Age trends in the level of serum testosterone and other hormones in middle-aged men: longitudinal results from the massachusetts male aging study. J Clin Endocrinol Metab. 2002;87:589–98.
Araujo AB, O’Donnell AB, Brambilla DJ, Simpson WB, Longcope C, Matsumoto AM, et al. Prevalence and incidence of androgen deficiency in middle-aged and older men: estimates from the massachusetts male aging study. J Clin Endocrinol Metab. 2004;89:5920–6.
Kaminetsky J, Jaffe JS, Swerdloff RS. Pharmacokinetic profile of subcutaneous testosterone enanthate delivered via a novel, prefilled single‐use autoinjector: a phase II study. Sex Med. 2015;3:269–79.
Mackey MA, Conway AJ, Handelsman DJ. Tolerability of intramuscular injections of testosterone ester in oil vehicle. Hum Reprod Oxf Engl. 1995;10:862–5.
de Ronde W. Hyperandrogenism after transfer of topical testosterone gel: case report and review of published and unpublished studies. Hum Reprod Oxf Engl. 2009;24:425–8.
Xu P, Choi E, El-Khatib FM, Yafi FA. Post-market single center experience with a subcutaneous auto-injector of testosterone enanthate (Xyosted). Eur Urol Open Sci. 2020;19:e129.
Kaminetsky JC, McCullough A, Hwang K, Jaffe JS, Wang C, Swerdloff RS. A 52-week study of dose adjusted subcutaneous testosterone enanthate in oil self-administered via disposable auto-injector. J Urol. 2019;201:587–94.
Gittelman M, Jaffe JS, Kaminetsky JC. Safety of a new subcutaneous testosterone enanthate auto-injector: results of a 26-week study. J Sex Med. 2019;16(Nov):1741–8.
Lee H-K, Lee JK, Cho B. The role of androgen in the adipose tissue of males. World J Mens Health. 2013;31(Aug):136–40.
Tan RS, Cook KR, Reilly WG. High estrogen in men after injectable testosterone therapy: the low T experience. Am J Mens Health. 2015;9:229–34.
Shahani S, Braga-Basaria M, Maggio M, Basaria S. Androgens and erythropoiesis: past and present. J Endocrinol Invest. 2009;32:704–16.
Jones SD, Dukovac T, Sangkum P, Yafi FA, Hellstrom WJG. Erythrocytosis and polycythemia secondary to testosterone replacement therapy in the aging male. Sex Med Rev. 2015;3:101–12.
Kavoussi PK, Machen GL, Wenzel JL, Ellis AM, Kavoussi M, Kavoussi KM, et al. Medical treatments for hypogonadism do not significantly increase the risk of deep vein thrombosis over general population risk. Urology 2019;124:127–30.
Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, et al. Testosterone therapy in men with androgen deficiency syndromes: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:2536–59.
Cooper CS, MacIndoe JH, Perry PJ, Yates WR, Williams RD. The effect of exogenous testosterone on total and free prostate specific antigen levels in healthy young men. J Urol. 1996;156:438–41. discussion 441–2.
Guay AT, Perez JB, Fitaihi WA, Vereb M. Testosterone treatment in hypogonadal men: prostate-specific antigen level and risk of prostate cancer. Endocr Pr J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2000;6:132–8.
Gerstenbluth RE, Maniam PN, Corty EW, Seftel AD. Prostate-specific antigen changes in hypogonadal men treated with testosterone replacement. J Androl. 2002;23:922–6.
Boyle P, Koechlin A, Bota M, d’Onofrio A, Zaridze DG, Perrin P, et al. Endogenous and exogenous testosterone and the risk of prostate cancer and increased prostate-specific antigen (PSA) level: a meta-analysis. BJU Int. 2016;118:731–41.
Loeb S, Folkvaljon Y, Damber J-E, Alukal J, Lambe M, Stattin P. Testosterone replacement therapy and risk of favorable and aggressive prostate cancer. J Clin Oncol J Am Soc Clin Oncol. 2017;35:1430–6.
ClinicalTrials.gov. A study to evaluate the effect of testosterone replacement therapy (TRT) on the incidence of major adverse cardiovascular events (MACE) and efficacy measures in hypogonadal men (TRAVERSE). 2020. https://clinicaltrials.gov/ct2/show/NCT03518034.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FAY: Antares Pharmaceuticals, Clarus Therapeutics, Coloplast, Promescent, Viome; PKK: Antares Pharmaceuticals, Acerus Pharmaceuticals, Clarus Therapeutics. The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Choi, E.J., Xu, P., El-Khatib, F.M. et al. Post-market safety and efficacy profile of subcutaneous testosterone enanthate-autoinjector: a cohort analysis. Int J Impot Res 34, 467–470 (2022). https://doi.org/10.1038/s41443-021-00435-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-021-00435-6