Abstract
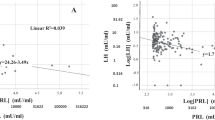
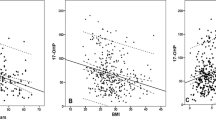
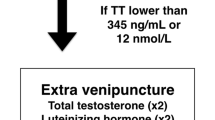
We aimed to evaluate the relationship between serum testosterone (T) levels and penile curvature in a cohort of men presenting for chronic phase Peyronie’s disease (PD). Clinical data from 149 patients assessed for chronic phase PD between 2016 and 2019 at a single academic center were analyzed. Deformity assessment was conducted during an intracavernosal injection-induced rigid erection. Both total T (tT) and calculated free T (cFT) were assessed in every patient and considered as continuous variables or according to quartiles of the normal range. Hypogonadism was defined for tT < 10.4 nmol/L. Descriptive statistics and linear regression models tested the association between T values and the severity of penile curvature. Overall, median tT value was 15.9 (11.4–20.8) nmol/L in the whole cohort; median curvature magnitude and plaque size were 45 (30–60) degrees and 1.5 (0.8–2.0) cm, respectively. Penile curvature (40.0 vs. 45.0 degree; p = 0.7) and plaque size (1.5 vs. 1.3 cm; p = 0.4) were similar between eugonadal and hypogonadal patients. The magnitude of penile curvature did not differ across tT quartiles (p = 0.31). Both at univariable (β 1.32; p < 0.01) and multivariable (β 1.34; p < 0.01) linear regression model, only duration of PD was associated with the severity of penile curvature magnitude. The results of this cross-sectional study confirmed that there is no association between serum T values and the severity of penile curvature in patients with chronic phase PD. Only PD duration is associated with penile deformity severity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Brock G, Hsu GL, Nunes L, Von Heyden B, Lue TF. The anatomy of the tunica albuginea in the normal penis and Peyronie’s disease. J Urol. 1997;157:276–81.
Mulhall JP, Schiff J, Guhring P. An analysis of the natural history of Peyronie’s disease. J Urol. 2006;175:2115–8.
Berookhim BM, Choi J, Alex B, Mulhall JP. Deformity stabilization and improvement in men with untreated Peyronie’s disease. BJU Int. 2014;113:133–6.
Kadioglu A, Tefekli A, Erol B, Oktar T, Tunc M, Tellaloglu S. A retrospective review of 307 men with peyronie’s disease. J Urol. 2002;168:1075–9.
Sharma KL, Alom M, Trost L. The etiology of Peyronie’s disease: pathogenesis and genetic contributions. Sex Med Rev. 2020;8:314–23.
Casabé A, Bechara A, Cheliz G, De Bonis W, Rey H. Risk factors of Peyronie’s disease. What does our clinical experience show? J Sex Med. 2011;8:518–23.
Rhoden EL, Riedner CE, Fuchs S, Ribeiro EP, Halmenschlager G. A cross-sectional study for the analysis of clinical, sexual and laboratory conditions associated to Peyronie’s disease. J Sex Med. 2010;7:1529–37.
La Pera G, Pescatori ES, Calabrese M, Boffini A, Colombo F, Andriani E, et al. Peyronie’s disease: prevalence and association with cigarette smoking: a multicenter population-based study in men aged 50–69 years. Eur Urol. 2001;40:525–30.
Ventimiglia E, Capogrosso P, Colicchia M, Boeri L, Serino A, La Croce G, et al. Peyronie’s disease and autoimmunity-a real-life clinical study and comprehensive review. J Sex Med. 2015;12:1062–9.
Moreno SA, Morgentaler A. Testosterone deficiency and Peyronie’s disease: pilot data suggesting a significant relationship. J Sex Med. 2009;6:1729–35.
Iacono F, Prezioso D, Ruffo A, Illiano E, Romis L, Di Lauro G, et al. Testosterone deficiency causes penile fibrosis and organic erectile dysfunction in aging men. Evaluating association among Age, TDS and ED. BMC Surg. 2012;12(Suppl 1):S24.
Cavallini G, Biagiotti G, Giudice C. Lo. Association between Peyronie disease and low serum testosterone levels: detection and therapeutic considerations. J Androl. 2012;33:381–8.
Mulhall JP, Matsushita K, Nelson CJ. Testosterone levels are not associated with magnitude of deformity in men with Peyronie’s disease. J Sex Med. 2019;16:1283–9.
Salonia A, Bettocchi C, Carvalho J, Corona G, Jones TH, Kadioglu A, et al. EAU guidelines on sexual and reproductive health. 2020. Available at: https://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Sexual-and-Reproductive-Health-2020.pdf. Accessed May 2020.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Quan H, Sundararajan V, Halfon P, Fong A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Liguori G, Salonia A, Garaffa G, Chiriacò G, Pavan N, Cavallini G, et al. Objective measurements of the penile angulation are significantly different than self-estimated magnitude among patients with penile curvature. Int Braz J Urol. 2018;44:555–62.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30.
Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999;54:346–51.
Hellstrom WJG, Feldman R, Rosen RC, Smith T, Kaufman G, Tursi J. Bother and distress associated with Peyronie’s disease: validation of the Peyronie’s disease questionnaire. J Urol. 2013;190:627–34.
Salonia A, Rastrelli G, Hackett G, Seminara SB, Huhtaniemi IT, Rey RA, et al. Paediatric and adult-onset male hypogonadism. Nat Rev Dis Prim. 2019;5:38.
Vermeulen A, Verdonck L, Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab. 1999;84:3666–72.
Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, Matsumoto AM, et al. Testosterone therapy in men with hypogonadism: an endocrine society. J Clin Endocrinol Metab. 2018;103:1715–44.
Bennette C, Vickers A. Against quantiles: categorization of continuous variables in epidemiologic research, and its discontents. BMC Med Res Methodol. 2012;12:21.
Garaffa G, Trost LW, Serefoglu EC, Ralph D, Hellstrom WJG. Understanding the course of Peyronie’s disease. Int J Clin Pract. 2013;67:781–8.
Kirby EW, Verges D, Matthews J, Carson CC, Coward RM. Low testosterone has a similar prevalence among men with sexual dysfunction due to either Peyronie’s disease or erectile dysfunction and does not correlate with Peyronie’s disease severity. J Sex Med. 2015;12:690–6.
Aditya I, Grober ED, Krakowsky Y. Peyronie’s disease and testosterone deficiency: is there a link? World J Urol. 2019;37:1035–41.
Karavitakis M, Komninos C, Simaioforidis V, Kontos S, Lefakis G, Politis V, et al. The relationship between androgens, regulators of collagen metabolism, and Peyronie’s disease: a case control study. J Sex Med. 2010;7:4011–7.
Demling RH. The role of anabolic hormones for wound healing in catabolic states. J Burns Wounds. 2005;4:e2.
Shen ZJ, Zhou XL, Lu YL, Chen ZD. Effect of androgen deprivation on penile ultrastructure. Asian J Androl. 2003;5:33–6.
Guay AT, Traish A. Testosterone deficiency and risk factors in the metabolic syndrome: implications for erectile dysfunction. Urol Clin N Am. 2011;38:175–83.
Nam HJ, Park HJ, Park NC. Does testosterone deficiency exaggerate the clinical symptoms of Peyronie’s disease? Int J Urol. 2011;18:796–800.
Müller A, Mulhall JP. Peyronie’s disease intervention trials: methodological challenges and issues. J Sex Med. 2009;6:848–61.
Diver MJ, Imtiaz KE, Ahmad AM, Vora JP, Fraser WD. Diurnal rhythms of serum total, free and bioavailable testosterone and of SHBG in middle-aged men compared with those in young men. Clin Endocrinol. 2003;58:710–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Candela, L., Boeri, L., Capogrosso, P. et al. Serum testosterone levels are not associated with the severity of penile curvature in men with Peyronie’s disease—findings from a cross-sectional study. Int J Impot Res 33, 832–838 (2021). https://doi.org/10.1038/s41443-020-0340-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-0340-7
This article is cited by
-
Are finasteride-related penile curvature/Peyronie’s disease Adverse Event Reports worthy of further clinical investigation? Disproportionality analysis based on both the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) pharmacovigilance databases
International Journal of Impotence Research (2023)