Abstract
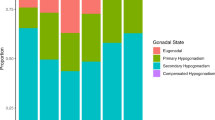
Male solid organ transplant patients are at increased risk of hypogonadism and the safety of treating these patients for hypogonadism is unknown. We sought to evaluate the safety of treating hypogonadism in the solid organ transplant recipient. To accomplish this, we performed a retrospective review between 2009 and 2017 of patients treated at a single academic urology clinic. Men who underwent a solid organ transplant with a diagnosis of hypogonadism (Testosterone <350 ng/dl) were included. In total, 87 hypogonadal transplant recipients were included (29 no treatment; 58 treated). Treatment modalities included non-testosterone therapies (human chorionic gonadotropin, clomiphene), topical, injectable, and subcutaneous T preparations. There was no difference between groups for baseline characteristics including age, length of follow-up since transplant, baseline testosterone, and transplant type. There was no difference in prostate cancer diagnoses, erythrocytosis, rejection, infections, number of unplanned admissions per patient. While there was no difference in the proportion of deaths in untreated (21%; n = 6) and treated transplant recipients (7%; n = 4; p = 0.08), the median survival was longer in men treated with T (p = 0.03). Treatment of hypogonadism in solid organ recipients did not increase the risk for adverse effects related to treatment of hypogonadism or solid organ transplant.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

References
2018 Annual Report of the U.S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: Transplant Data 1994-2018. Rockville, MD: Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation; Richmond, VA: United Network for Organ Sharing; Ann Arbor, MI: University Renal Research and Education Association; 2018.
Opelz G, Döhler B, Ruhenstroth A, Cinca S, Unterrainer C, Stricker L, et al. The collaborative transplant study registry. 2013. https://doi.org/10.1016/j.trre.2013.01.004.
Thirumavalavan N, Scovell JM, Link RE, Lamb DJ, Lipshultz LI. Does solid organ transplantation affect male reproduction?. Eur Urol Focus. 2018;4:307–10.
Thirumavalavan N, Wilken NA, Ramasamy R. Hypogonadism and renal failure: an update. Indian J Urol. 2015;31:89.
Carrero JJ, Qureshi AR, Nakashima A, Arver S, Parini P, Lindholm B, et al. Prevalence and clinical implications of testosterone deficiency in men with end-stage renal disease. Nephrol Dial Transpl. 2011;26:184–90.
Reinhardt W, Kübber H, Dolff S, Benson S, Führer D, Tan S. Rapid recovery of hypogonadism in male patients with end stage renal disease after renal transplantation. Endocrine. 2018;60:159–66.
Albaaj F, Sivalingham M, Haynes P, McKinnon G, Foley RN, Waldek S, et al. Prevalence of hypogonadism in male patients with renal failure. Postgrad Med J. 2006;82:693–6.
Serra E, Porcu M, Minerba L, Serra S, Oppo A, Orrù P, et al. High prevalence of male hypogonadism and sexual dysfunction in long-term clinically stable heart transplantation recipients. Int J Cardiol. 2012;155:476–7.
Poglajen G, Jensterle M, Kravos N, Janež A, Vrtovec B. Low serum testosterone is associated with impaired graft function early after heart transplantation. Clin Transpl. 2017;31:e12970.
Nitsche R, Coelho JCU, de Freitas ACT, Zeni Neto C, Martins E. Testosterone changes in patients with liver cirrhosis before and after orthotopic liver transplantation and its correlation with meld. Arq Gastroenterol. 2014;51:59–63.
Yeap BB, Alfonso H, Paul Chubb SA, Handelsman DJ, Hankey GJ, Almeida OP, et al. In older men an optimal plasma testosterone is associated with reduced all-cause mortality and higher dihydrotestosterone with reduced ischemic heart disease mortality, while estradiol levels do not predict mortality. J Clin Endocrinol Metab. 2014;99:9–18.
Grossmann M, Hoermann R, Ng Tang Fui M, Zajac JD, Ierino FL, Roberts MA. Sex steroids levels in chronic kidney disease and kidney transplant recipients: associations with disease severity and prediction of mortality. Clin Endocrinol (Oxf). 2015;82:767–75.
Shoskes DA, Kerr H, Askar M, Goldfarb DA, Schold J. Low testosterone at time of transplantation is independently associated with poor patient and graft survival in male renal transplant recipients. J Urol. 2014;192:1168–71.
Dean JD, McMahon CG, Guay AT, Morgentaler A, Althof SE, Becher EF, et al. The International Society for Sexual Medicine’s process of care for the assessment and management of testosterone deficiency in adult men. J Sex Med. 2015;12:1660–86.
Majzoub A, Shoskes DA. A case series of the safety and efficacy of testosterone replacement therapy in renal failure and kidney transplant patients. Transl Androl Urol. 2016;5:814–8.
Amory JK, Chansky HA, Chansky KL, Camuso MR, Hoey CT, Anawalt BD, et al. Preoperative supraphysiological testosterone in older men undergoing knee replacement surgery. J Am Geriatr Soc. 2002;50:1698–701.
Wu B, Lorezanza D, Badash I, Berge M, Lane C, Sum JC, et al. Perioperative testosterone supplementation increases lean mass in healthy men undergoing anterior cruciate ligament reconstruction: a randomized controlled trial. Orthop J Sport Med. 2017;5. https://doi.org/10.1177/2325967117722794.
Wu BW, Berger M, Sum JC, Hatch GF III, Todd Schroeder, E. Randomized control trial to evaluate the effects of acute testosterone administration in men on muscle mass, strength, and physical function following ACL reconstructive surgery: rationale, design, methods. BMC Surg. 2014. https://doi.org/10.1186/1471-2482-14-102.
Burch PT, Spigarelli MG, Lambert LM, Loftus PD, Sherwin CM, Linakis MW, et al. Use of oxandrolone to promote growth in neonates following surgery for complex congenital heart disease: an open-label pilot trial. Congenit Heart Dis. 2016;11:693–9.
Maggio M, Nicolini F, Cattabiani C, Beghi C, Gherli T, Schwartz RS, et al. Effects of testosterone supplementation on clinical and rehabilitative outcomes in older men undergoing on-pump CABG. Contemp Clin Trials. 2012;33:730–8.
Toma M, Mcalister FA, Coglianese EE, Vidi V, Vasaiwala S, Bakal JA, et al. Testosterone supplementation in heart failure: a meta-analysis. 2012. https://doi.org/10.1161/CIRCHEARTFAILURE.111.965632/-/DC1.
Argalious MY, You J, Mao G, Ramos D, Khanna S, Maheshwari K, et al. Association of testosterone replacement therapy and the incidence of a composite of postoperative in-hospital mortality and cardiovascular events in men undergoing noncardiac surgery. Anesthesiology. 2017;127:457–65.
Corona G, Monami M, Rastrelli G, Aversa A, Tishova Y, Saad F, et al. Testosterone and metabolic syndrome: a meta-analysis study. J Sex Med. 2011;8:272–83.
Zhang LT, Shin YS, Kim JY, Park JK. Could testosterone replacement therapy in hypogonadal men ameliorate anemia, a cardiovascular risk factor? An observational, 54-week cumulative registry study. J Urol. 2016;195:1057–64.
Trigunaite A, Dimo J. Suppressive effects of androgens on the immune system. Cell Immunol. 2015;294:87–94.
Uchiyama M, Jin X, Zhang Q, Amano A, Watanabe T, Niimi M. Induction of regulatory CD4+ cells and prolongation of survival of fully allogeneic murine cardiac grafts by danazol. TPS. 2012;44:1067–9.
Neff GW, O’Brien CB, Shire NJ, DeManno A, Kahn S, Rideman E, et al. Topical testosterone treatment for chronic allograft failure in liver transplant recipients with recurrent hepatitis C virus. Transpl Proc. 2004;36:3071–4.
Funding
This work is supported in part by National Institute of General Medical Sciences of the National Institutes of Health under Award Number T32GM088129, NIH grant K12 DK0083014, the Multidisciplinary K12 Urologic Research (KURe) Career Development Program (NT is a K12 Scholar). AWP is a National Institutes of Health K08 Scholar supported by a Mentored Career Development Award (K08DK115835-01) from the National Institute of Diabetes and Digestive and Kidney Diseases. This work is also supported in part through a Urology Care Foundation Rising Stars in Urology Award (to AWP).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Thirumavalavan, N., Scovell, J.M., Lo, E. et al. Is treatment of hypogonadism safe for men after a solid organ transplant? Results from a retrospective controlled cohort study. Int J Impot Res 34, 50–54 (2022). https://doi.org/10.1038/s41443-020-00361-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-00361-z
This article is cited by
-
Testosterone deficiency in men with end stage renal disease and kidney transplantation: a narrative review
International Journal of Impotence Research (2024)
-
Testosterone deficiency in male organ transplant recipients
International Journal of Impotence Research (2022)