Abstract
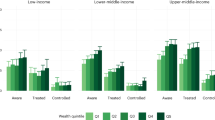
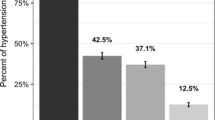
Few studies focused on the equity of hypertension prevalence before and after the diagnostic threshold change. The study aimed to analyze the 130/80 mmHg hypertension diagnostic threshold on the equity of hypertension prevalence in China. The baseline survey data from the China Health and Retirement Longitudinal Study (CHARLS) conducted from 2011 to 2012 were utilized to evaluate the impact of the 130/80 mmHg diagnostic threshold on the equity of hypertension prevalence in China using the concentration index and its decomposition which was an index reflecting the health inequality caused by social and economic factors. The prevalence of hypertension was 41.56% and 57.33% under the diagnostic thresholds of 140/90 mmHg and 130/80 mmHg, respectively. The concentration index for hypertension prevalence in China was −0.017 (95%CI: −0.028, −0.006) under the 140/90 mmHg threshold and −0.010 (95%CI: −0.018, −0.002) under the 130/80 mmHg threshold. Concentration index decomposition analysis of hypertension prevalence diagnosed at both diagnostic thresholds showed that age, BMI, and economic status contributed more to the inequitable situation of hypertension prevalence. Higher age, higher BMI, and poorer economic status increased the inequity of hypertension prevalence. No significant difference in the increase in hypertension among individuals of different economic status after implementing the blood pressure control standard (130/80 mmHg), and the prevalence of hypertension in the region did not show a significant bias towards the low economic status population. Therefore, implementing this standard will not increase the risk of hypertension prevalence biased toward people of low economic status.

Implementing the 130/80 mmHg diagnostic threshold will not increase the risk of hypertension prevalence biased towards people of low economic status.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All datasets are available from the China Health and Retirement Longitudinal Study (CHARLS) database (http://charls.pku.edu.cn/). Researchers who want to use these data can register accounts via the website.
References
Lou Y, Ma WJ, Wang ZJ, Yang L, Sun YJ, Liu YL, et al. Writing protocols for the Chinese clinical practice guidelines of hypertension. Chin J Cardiol. 2022;50:671–5.
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018;137:2344–56.
Wang Z, Hao G, Wang X, Chen Z, Zhang L, Zhang Z, et al. Clinical outcomes and economic impact of the 2017 ACC/AHA guidelines on hypertension in China. J Clin Hypertens. 2019;21:1212–20.
Ma S, Yang L, Zhao M, Magnussen CG, Xi B. Trends in hypertension prevalence, awareness, treatment and control rates among Chinese adults, 1991-2015. J Hypertens. 2021;39:740–8.
National Health Commission of the People’s Republic of China. The national diagnostic criteria for hypertension in adults have not been adjusted. https://news.cctv.com/2022/11/16/ARTIwrEoTU2HoiDlunwQYT1h221116.shtml.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–248.
Khera R, Lu Y, Lu J, Saxena A, Nasir K, Jiang L, et al. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross-sectional study. BMJ. 2018;362:K2357.
Li C, Chen K, Cornelius V, Tomeny E, Wang Y, Yang X, et al. Applicability and cost-effectiveness of the Systolic Blood Pressure Intervention Trial (SPRINT) in the Chinese population: a cost-effectiveness modeling study. Plos Med. 2021;18:e1003515.
Bress AP, Bellows BK, King JB, Hess R, Beddhu S, Zhang Z, et al. Cost-Effectiveness of Intensive versus Standard Blood-Pressure Control. N. Engl J Med. 2017;377:745–55.
Lee YS, Lee H-Y, Kim TH. Cost-effectiveness analysis of intensive blood pressure control in Korea. Hypertens Res. 2022;45:507–15.
Chinese Hypertension Prevention and Treatment Guidelines Revision Committee. Chinese hypertension prevention and treatment guidelines 2018 revised edition. Prev Treat Cardiovasc Cerebrovasc Dis. 2019;19:1–44.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: The China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43:61–68.
Kakwani N, Wagstaff A, vanDoorslaer E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. J Econ. 1997;77:87–103.
Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek F, Hosseinpour AR, et al. Inequality in household catastrophic health care expenditure in a low-income society of Iran. Health Policy Plan. 2012;27:613–23.
Omotoso KO, Koch SF. Assessing changes in social determinants of health inequalities in South Africa: a decomposition analysis. Int J Equity Health. 2018;17:1–13.
Mutyambizi C, Booysen F, Stokes A, Pavlova M, Groot W. Lifestyle and socio-economic inequalities in diabetes prevalence in South Africa: a decomposition analysis. PloS One. 2019;14:e0211208.
Li D, Zeng X, Huang Y, Lei H, Li G, Zhang N, et al. Increased risk of hypertension in young adults in Southwest China: impact of the 2017 ACC/AHA high blood pressure guideline. Curr Hypertens Rep. 2019;21:21.
Liu N, Yang JJ, Meng R, Pan X-F, Zhang X, He M, et al. Associations of blood pressure categories defined by 2017 ACC/AHA guidelines with mortality in China: pooled results from three prospective cohorts. Eur J Prev Cardiol. 2020;27:345–54.
Lai S, Shen C, Yang X, Zhang X, Xu Y, Li Q, et al. Socioeconomic inequalities in the prevalence of chronic diseases and preventive care among adults aged 45 and older in Shaanxi Province, China. BMC Public Health. 2019;19:1–12.
Bono F, Matranga D. Socioeconomic inequality in non-communicable diseases in Europe between 2004 and 2015: evidence from the SHARE survey. Eur J Public Health. 2019;29:105–10.
de Gaudemaris R, Lang T, Chatellier G, Larabi L, Lauwers-Cances V, Maitre A, et al. Socioeconomic inequalities in hypertension prevalence and care—the IHPAF study. Hypertension. 2002;39:1119–25.
Wu X, Wang Z. Role of socioeconomic status in hypertension among Chinese middle-aged and elderly individuals. Int J Hypertens. 2019; 2019:1–6.
Lei X, Yin N, Zhao Y. Socioeconomic status and chronic diseases: the case of hypertension in China. China Econ Rev. 2012;23:105–21.
Cao D, Zhou Z, Si Y, Xiao X, Wang X, Shen C, et al. Prevalence and income-related equity in hypertension in rural China from 1991 to 2011: differences between self-reported and tested measures. BMC Health Serv Res. 2019;19:1–11.
Dalstra JAA, Kunst AE, Borrell C, Breeze E, Cambois E, Costa G, et al. Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. Int J Epidemiol. 2005;34:316–26.
Fu Y, Lin W, Yang Y, Du R, Gao D. Analysis of diverse factors influencing the health status as well as medical and health service utilization in the floating elderly of China. BMC Health Serv Res. 2021;21:438.
Wang W, Lv J, Yu C, Guo Y, Pei P, Zhuang Z, et al. Lifestyle factors and fetal and childhood origins of type 2 diabetes: a prospective study of Chinese and European adults. Am J Clin Nutr. 2022;115:749–58.
Song C, Lv J, Yu C, Zhu M, Yu C, Guo Y, et al. Adherence to healthy lifestyle and liver cancer in Chinese: a prospective cohort study of 0.5 million people. Br J Cancer. 2022;126:815–21.
Phelan JC, Link BG. Controlling disease and creating disparities: a fundamental cause perspective. J Gerontol Ser B: Psychol Sci Soc Sci. 2005;60:S27–33.
Bonaccio M, Di Castelnuovo A, Costanzo S, Persichillo M, Donati MB, de Gaetano G, et al. Interaction between education and income on the risk of all-cause mortality: prospective results from the MOLI-SANI study. Int J Public Health. 2016;61:765–76.
Schutte AE, Srinivasapura Venkateshmurthy N, Mohan S, Prabhakaran D. Hypertension in low-and middle-income countries. Circ Res. 2021;128:808–26.
Geldsetzer P, Manne-Goehler J, Marcus M-E, Ebert C, Zhumadilov Z, Wesseh CS, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1.1 million adults. Lancet. 2019;394:652–62.
Rosengren A, Smyth A, Rangarajan S, Ramasundarahettige C, Bangdiwala SI, AlHabib KF, et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob Health. 2019;7:e748–60.
Acknowledgements
This article received support from the Education Department of Shaanxi Provincial Government under Grant No. 21JK0340. We thank all the CHARLS (China Health and Retirement Longitudinal Study) study participants and trial investigators. This article was prepared using research materials obtained from the Peking University Open Research Data Platform.
Funding
This work was supported by the Education Department of Shaanxi Provincial Government under Grant No. 21JK0340.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethnics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki. The original CHARLS was approved by the Ethical Review Committee of Peking University, and all the participants from CHARLS provided signed informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Z., Shi, G., Xing, Y. et al. Examining the potential impacts of intensive blood pressure treatment on the socioeconomic inequity in hypertension prevalence in China: a nationally representative cross-sectional study. Hypertens Res 46, 2746–2753 (2023). https://doi.org/10.1038/s41440-023-01441-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01441-5