Abstract
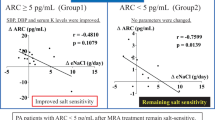
Primary aldosteronism (PA) is typically managed with mineralocorticoid receptor antagonists (MRAs) barring adrenalectomy. The efficacy of esaxerenone, a nonsteroidal MRA, were explored in patients with PA. Various parameters such as the urinary albumin to creatinine ratio (UACR) and serum levels of N-terminal prohormone of brain natriuretic peptide (NT-proBNP) were evaluated in 25 PA patients before and 3 and 6 months after esaxerenone treatment. Systolic and diastolic blood pressure (BP), and the estimated glomerular filtration rate decreased after treatment, while serum levels of potassium and active renin increased. Significant reductions were observed in UACR 3 and 6 months after treatment. A significant decrease in NT-proBNP was evident at 6 months but not 3 months after treatment. Correlation analysis indicated that the reductions in BP and UACR at 3 months were independent of estimated daily salt intake. Furthermore, the effect of esaxerenone treatment on lowering UACR and NT-proBNP levels was independent of BP reduction. Responders whose systolic BP decreased 6 months after esaxerenone treatment by more than 10 mmHg compared to pretreatment had higher pretreatment NT-proBNP and similar UACR before and after treatment when compared with nonresponders. Esaxerenone improved mental, physical, and social quality of life (QOL) 6 months after treatment compared to healthy controls and increased over time. No patients discontinued treatment due to severe hyperkalemia or renal dysfunction. In conclusion, esaxerenone is a safe and effective MRA for PA treatment, offering significant benefits in terms of hypertension, albuminuria, NT-proBNP levels, and QOL improvement.

Esaxerenone effectively lowers BP, UACR, and serum levels of NT-proBNP independent of dietary salt intake in mild PA patients. ARC active renin concentration, DBP diastolic blood pressure, MR mineralocorticoid receptor, MRA mineralocorticoid receptor antagonist, NT-proBNP N-terminal pro-brain natriuretic peptide, PA primary aldosteronism, QOL quality of life, SBP systolic blood pressure, SF-36 Medical Outcomes Study 36-Item Short-Form Health Survey, UACR urinary albumin to creatinine ratio.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Mulatero P, Stowasser M, Loh KC, Fardella CE, Gordon RD, Mosso L, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab. 2004;89:1045–50.
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48:2293–300.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Born-Frontsberg E, Reincke M, Rump LC, Hahner S, Diederich S, Lorenz R, et al. Cardiovascular and cerebrovascular comorbidities of hypokalemic and normokalemic primary aldosteronism: results of the German Conn’s Registry. J Clin Endocrinol Metab. 2009;94:1125–30.
Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of Cardiovascular Disease and Its Risk Factors in Primary Aldosteronism: A Multicenter Study in Japan. Hypertension. 2018;71:530–7.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–17.
Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348:1309–21.
Zannad F, McMurray JJ, Krum H, van Veldhuisen DJ, Swedberg K, Shi H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11–21.
Saiki A, Otsuki M, Tamada D, Kitamura T, Mukai K, Yamamoto K, et al. Increased Dosage of MRA Improves BP and Urinary Albumin Excretion in Primary Aldosteronism With Suppressed Plasma Renin. J Endocr Soc. 2022;6:bvab174.
Bianchi S, Bigazzi R, Campese VM. Long-term effects of spironolactone on proteinuria and kidney function in patients with chronic kidney disease. Kidney Int. 2006;70:2116–23.
Epstein M, Williams GH, Weinberger M, Lewin A, Krause S, Mukherjee R, et al. Selective aldosterone blockade with eplerenone reduces albuminuria in patients with type 2 diabetes. Clin J Am Soc Nephrol. 2006;1:940–51.
Ito S, Itoh H, Rakugi H, Okuda Y, Yoshimura M, Yamakawa S. Double-Blind Randomized Phase 3 Study Comparing Esaxerenone (CS-3150) and Eplerenone in Patients With Essential Hypertension (ESAX-HTN Study). Hypertension. 2020;75:51–8.
Ito S, Kashihara N, Shikata K, Nangaku M, Wada T, Okuda Y, et al. Esaxerenone (CS-3150) in Patients with Type 2 Diabetes and Microalbuminuria (ESAX-DN): Phase 3 Randomized Controlled Clinical Trial. Clin J Am Soc Nephrol. 2020;15:1715–27.
Uchida HA, Nakajima H, Hashimoto M, Nakamura A, Nunoue T, Murakami K, et al. Efficacy and Safety of Esaxerenone in Hypertensive Patients with Diabetic Kidney Disease: A Multicenter, Open-Label, Prospective Study. Adv Ther. 2022;39:5158–75.
Satoh F, Ito S, Itoh H, Rakugi H, Shibata H, Ichihara A, et al. Efficacy and safety of esaxerenone (CS-3150), a newly available nonsteroidal mineralocorticoid receptor blocker, in hypertensive patients with primary aldosteronism. Hypertens Res. 2021;44:464–72.
Fujimoto M, Watanabe S, Igarashi K, Ruike Y, Ishiwata K, Naito K, et al. Antihypertensive Effects of Esaxerenone in Older Patients with Primary Aldosteronism. Int J Hypertens. 2023;2023:6453933.
Brown MJ, Auchus RJ, Honzel B, Luther MJ, Yozamp N, Vaidya A. Re-Calibrating Interpretations of Aldosterone Assays Across the Physiologic Range: Immunoassay and Liquid Chromatography-Tandem Mass Spectrometry Measurements Under Multiple Controlled Conditions. J Endocr Soc. 2022;7:bvac049.
Ozeki Y, Tanimura Y, Nagai S, Nomura T, Kinoshita M, Shibuta K, et al. Development of a New Chemiluminescent Enzyme Immunoassay Using a Two-Step Sandwich Method for Measuring Aldosterone Concentrations. Diagnostics (Basel). 2021;11.
Nishikawa T, Satoh F, Takashi Y, Yanase T, Itoh H, Kurihara I, et al. Comparison and commutability study between standardized liquid chromatography-mass spectrometry/mass spectrometry (LC-MS/MS) and chemiluminescent enzyme immunoassay for aldosterone measurement in blood. Endocr J. 2022;69:45–54.
Teruyama K, Naruse M, Tsuiki M, Kobayashi H. Novel chemiluminescent immunoassay to measure plasma aldosterone and plasma active renin concentrations for the diagnosis of primary aldosteronism. J Hum Hypertens. 2022;36:77–85.
Naruse M, Katabami T, Shibata H, Sone M, Takahashi K, Tanabe A, et al. Japan Endocrine Society clinical practice guideline for the diagnosis and management of primary aldosteronism 2021. Endocr J. 2022;69:327–59.
Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Fukuhara S, Ware JE Jr, Kosinski M, Wada S, Gandek B. Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. J Clin Epidemiol. 1998;51:1045–53.
Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol. 1998;51:1037–44.
Brazier JE, Fukuhara S, Roberts J, Kharroubi S, Yamamoto Y, Ikeda S, et al. Estimating a preference-based index from the Japanese SF-36. J Clin Epidemiol. 2009;62:1323–31.
Rose BD. Diuretics. Kidney Int. 1991;39:336–52.
Yoshida Y, Fujiki R, Kinoshita M, Sada K, Miyamoto S, Ozeki Y, et al. Importance of dietary salt restriction for patients with primary aldosteronism during treatment with mineralocorticoid receptor antagonists: The potential importance of post-treatment plasma renin levels. Hypertens Res. 2023;46:100–7.
Shibata H, Itoh H. Mineralocorticoid receptor-associated hypertension and its organ damage: clinical relevance for resistant hypertension. Am J Hypertens. 2012;25:514–23.
Shibata S, Nagase M, Yoshida S, Kawarazaki W, Kurihara H, Tanaka H, et al. Modification of mineralocorticoid receptor function by Rac1 GTPase: implication in proteinuric kidney disease. Nat Med. 2008;14:1370–6.
Collard D, Brouwer TF, Olde Engberink RHG, Zwinderman AH, Vogt L, van den Born BH. Initial Estimated Glomerular Filtration Rate Decline and Long-Term Renal Function During Intensive Antihypertensive Therapy: A Post Hoc Analysis of the SPRINT and ACCORD-BP Randomized Controlled Trials. Hypertension. 2020;75:1205–12.
Sonino N, Fallo F, Fava GA. Psychological aspects of primary aldosteronism. Psychother Psychosom. 2006;75:327–30.
Sukor N, Kogovsek C, Gordon RD, Robson D, Stowasser M. Improved quality of life, blood pressure, and biochemical status following laparoscopic adrenalectomy for unilateral primary aldosteronism. J Clin Endocrinol Metab. 2010;95:1360–4.
Ahmed AH, Gordon RD, Sukor N, Pimenta E, Stowasser M. Quality of life in patients with bilateral primary aldosteronism before and during treatment with spironolactone and/or amiloride, including a comparison with our previously published results in those with unilateral disease treated surgically. J Clin Endocrinol Metab. 2011;96:2904–11.
Sonino N, Tomba E, Genesia ML, Bertello C, Mulatero P, Veglio F, et al. Psychological assessment of primary aldosteronism: a controlled study. J Clin Endocrinol Metab. 2011;96:E878–83.
Kunzel HE, Apostolopoulou K, Pallauf A, Gerum S, Merkle K, Schulz S, et al. Quality of life in patients with primary aldosteronism: gender differences in untreated and long-term treated patients and associations with treatment and aldosterone. J Psychiatr Res. 2012;46:1650–4.
Velema M, Dekkers T, Hermus A, Timmers H, Lenders J, Groenewoud H, et al. Quality of Life in Primary Aldosteronism: A Comparative Effectiveness Study of Adrenalectomy and Medical Treatment. J Clin Endocrinol Metab. 2018;103:16–24.
Citton M, Viel G, Torresan F, Rossi GP, Iacobone M. Effect of unilateral adrenalectomy on the quality of life of patients with lateralized primary aldosteronism. BMC Surg. 2019;18:105.
Ishidoya S, Kawasaki Y, Namiki S, Morimoto R, Takase K, Ito A. Changes in quality of life after laparoscopic adrenalectomy for patients with primary aldosteronism: Prospective 2-year longitudinal cohort study in a Japanese tertiary center. Int J Urol. 2019;26:752–3.
Yoshida Y, Yoshida R, Shibuta K, Ozeki Y, Okamoto M, Gotoh K, et al. Quality of Life of Primary Aldosteronism Patients by Mineralocorticoid Receptor Antagonists. J Endocr Soc. 2021;5:bvab020.
Hlavacova N, Jezova D. Chronic treatment with the mineralocorticoid hormone aldosterone results in increased anxiety-like behavior. Horm Behav. 2008;54:90–7.
Hlavacova N, Bakos J, Jezova D. Eplerenone, a selective mineralocorticoid receptor blocker, exerts anxiolytic effects accompanied by changes in stress hormone release. J Psychopharmacol. 2010;24:779–86.
Gard PR. Angiotensin as a target for the treatment of Alzheimer’s disease, anxiety and depression. Expert Opin Ther Targets. 2004;8:7–14.
Saavedra JM, Ando H, Armando I, Baiardi G, Bregonzio C, Juorio A, et al. Anti-stress and anti-anxiety effects of centrally acting angiotensin II AT1 receptor antagonists. Regul Pept. 2005;128:227–38.
Velema MS, de Nooijer AH, Burgers VWG, Hermus A, Timmers H, Lenders JWM, et al. Health-Related Quality of Life and Mental Health in Primary Aldosteronism: A Systematic Review. Horm Metab Res. 2017;49:943–50.
Gaddam K, Pimenta E, Thomas SJ, Cofield SS, Oparil S, Harding SM, et al. Spironolactone reduces severity of obstructive sleep apnoea in patients with resistant hypertension: a preliminary report. J Hum Hypertens. 2010;24:532–7.
Acknowledgements
We thank the physicians and medical staff of the Department of Endocrinology and Diabetology, Oita University Hospital, who treated the patients who participated in this study.
Funding
This study was funded by Daiwa Securities Health Foundation #48-①-24and by Grand-in-Aid for the Intractable Adrenal Disorders Research by the Ministry of Health, Labour and Welfare (HS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HS has honorarium from Daiichi-Sankyo Company, Bayer, Mochida Pharmaceuticals, Astrazeneca, Novartis Pharma, and Astellas. HS also received scholarship from Chugai and Bayer.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoshida, Y., Fujiwara, M., Kinoshita, M. et al. Effects of esaxerenone on blood pressure, urinary albumin excretion, serum levels of NT-proBNP, and quality of life in patients with primary aldosteronism. Hypertens Res 47, 157–167 (2024). https://doi.org/10.1038/s41440-023-01412-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01412-w
Keywords
This article is cited by
-
No “U-shaped” associations of estimated glomerular filtration rate with adverse cardiovascular outcomes in patients with primary aldosteronism
Hypertension Research (2024)
-
Relations between glomerular hyperfiltration and podocyte injury: potential role of Piezo1 in the Rac1-mineralocorticoid receptor activation pathway
Hypertension Research (2024)