Abstract
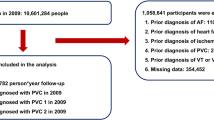
Atrial fibrillation (AF) is common in hypertension, and electrophysiological remodelling may contribute to the early stage of the disease. This study aimed to develop electrocardiography (ECG) prediction models on new-onset AF (NAF) in early-onset hypertension (e-HTN). This matched case-control study included primary hypertension patients with onset <5 years defined as e-HTN and without documented AF. Developed NAF was the risk group and non-developed NAF was control group with 1:2 ratio. Group was matched according to age, gender, follow-up time, and duration of hypertension. Parameters of ECG and echocardiography between the groups at the baseline and end of follow-up will be compared. A total of 348 e-HTN with 116 developed NAF during follow-up (60.2 ± 14.5 months) were included. At baseline ECG, duration of QRS (100.84 ms ± 15.69 ms vs 94.80 ms ± 15.68 ms), Pmax (106.75 ms ± 7.93 ms vs 101.77 ms ± 6.78 ms), Pmin (70.24 ms ± 5.59 ms vs 68.17 ms ± 5.61 ms), P-wave dispersion (PD) (36.50 ms ± 5.25 ms vs 33.60 ms ± 5.46 ms), P-wave Peak Time (PWPT) II (62.01 ms ± 3.92 ms vs 54.29 ms ± 6.73 ms), and PWPT V1 (55.31 ms ± 2.89 ms vs 51.24 ms ± 4.05 ms) were significantly higher in developed NAF (all P-value < 0.05). LVMI was also significantly higher in bivariate analysis, but only Pmax, Pmin, PD, PWPT, non-RAAS inhibitor, and uncontrolled hypertension were independently associated with developed NAF. Baseline PWPT II with cut-off ≥57.9 ms and PD ≥ 35.5 ms has high sensitivity and specificity on NAF prediction. In conclusion, baseline PWPT and PD are potential electrophysiological parameters for predicting NAF in e-HTN.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Karamitanha F, Ahmadi F, Fallahabadi H. Difference Between Various Countries in Mortality and Incidence Rate of the Atrial Fibrillation Based on Human Development Index in Worldwide: Data From Global Burden of Disease 2010–2019. Curr Probl Cardiol. 2023;48:1–17.
Jones NR, Taylor CJ, Hobbs FDR, Bowman L, Casadei B. Screening for atrial fibrillation: A call for evidence. Eur Heart J. 2020;41:1075–85.
Khurshid S, Healey JS, McIntyre WF, Lubitz SA. Population-Based Screening for Atrial Fibrillation. Circ Res. 2020;127:143–54.
Eckstein J, Conen D, Kühne M. Atrial fibrillation: A moving target. Swiss Med Wkly. 2014;144:1–11.
Verdecchia P, Angeli F, Reboldi G. Hypertension and atrial fibrillation: Doubts and certainties from basic and clinical studies. Circ Res. 2018;122:352–68.
Verdecchia P, Staessen JA, Angeli F, de Simone G, Achilli A, Ganau A, et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial. Lancet. 2009;374:525–33.
Verdecchia P, Dagenais G, Healey J, Gao P, Dans AL, Chazova I, et al. Blood pressure and other determinants of new-onset atrial fibrillation in patients at high cardiovascular risk in the Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial/Telmisartan Randomized AssessmeNt Study in ACE iNtolerant subjects with cardiovascular Disease studies. J Hypertens. 2012;30:1004–14.
Kawakami H, Ramkumar S, Nolan M, Wright L, Yang H, Negishi K, et al. Left Atrial Mechanical Dispersion Assessed by Strain Echocardiography as an Independent Predictor of New-Onset Atrial Fibrillation: A Case-Control Study. J Am Soc Echocardiogr. 2019;32:1268–76.e3.
Rosenberg MA, Gottdiener JS, Heckbert SR, Mukamal KJ. Echocardiographic diastolic parameters and risk of atrial fibrillation: The cardiovascular health study. Eur Heart J. 2012;33:904–12.
Potter A, Pearce K, Hilmy N. The benefits of echocardiography in primary care. Br J Gen Pract. 2019;69:358–9.
Kabutoya T, Kario K. P-wave changes as an index of hypertensive organ damage and a predictor of cardiovascular events: can the P wave be used to assess atrial reverse remodeling? Hypertens Res. 2022;45:1400–3.
Kabutoya T, Hoshide S, Kario K. Notched P-Wave on Digital Electrocardiogram Predicts Cardiovascular Events in Patients with Cardiovascular Risks: The Japan Morning Surge Home Blood Pressure Study. Cardiology. 2022;147:307–14.
Duyuler TP, Duyuler S, Demirtas B, Cicekcioglu H, Cayhan V. P wave peak time and P wave dispersion in severe COVID-19 infection. Eur Rev Med Pharmacol Sci. 2022;26:4456–62.
Keleşoğlu Ş. Assessment of P Wave Peak Time and P Wave Dispersion in Patients with COVID-19 Infection. Erciyes Med J. 2022;44:375–81.
Tachmatzidis D, Filos D, Chouvarda I, Tsarouchas A, Mouselimis D, Bakogiannis C, et al. Beat-to-beat p-wave analysis outperforms conventional p-wave indices in identifying patients with a history of paroxysmal atrial fibrillation during sinus rhythm. Diagnostics 2021;11:1–17.
Dogan U, Apaydin Dogan E, Tekinalp M, Serhat Tokgoz O, Aribas A, Akilli H, et al. P-wave Dispersion for Predicting Paroxysmal Atrial Fibrillation in Acute Ischemic Stroke. Int J Med Sci. 2012. http://www.medsci.org108.
Yıldırım E, Günay N, Bayam E, Keskin M, Ozturkeri B, Selcuk M. Relationship between paroxysmal atrial fibrillation and a novel electrocardiographic parameter P wave peak time. J Electrocardiol. 2019;57:81–6.
Boyraz B, İbişoğlu E. Effects of COVID-19 Infection on P-Wave Dispersion, P-Wave Peak Time and Atrial Conduction Times. e-J Cardiovasc Med. 2021;9:143–9.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75:1334–57.
Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15:155–63.
Burak C, Çağdaş M, Rencüzoğulları I, Karabağ Y, Artaç I, Yesin M, et al. Association of P wave peak time with left ventricular end-diastolic pressure in patients with hypertension. J Clin Hypertens. 2019;21:608–15.
Çağdaş M, Karakoyun S, Rencüzoğulları İ, Karabağ Y, Yesin M, Gürsoy MO, et al. P wave peak time; a novel electrocardiographic parameter in the assessment of coronary no-reflow. J Electrocardiol. 2017;50:584–90.
Rosenberg MA, Manning WJ. Diastolic dysfunction and risk of atrial fibrillation: a mechanistic appraisal. Circulation 2012;126:2353–62.
Jarasunas J, Aidietis A, Aidietiene S. Left atrial strain - An early marker of left ventricular diastolic dysfunction in patients with hypertension and paroxysmal atrial fibrillation. Cardiovasc Ultrasound. 2018;16:1–9.
Tsang TSM, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left Atrial Volume as a Morphophysiologic Expression of Left Ventricular Diastolic Dysfunction and Relation to Cardiovascular Risk Burden. Am J Cardiol. 2002;90:1284–9.
Ikejder Y, Sebbani M, Hendy I, Khramz M, Khatouri A, Bendriss L. Impact of Arterial Hypertension on Left Atrial Size and Function. Biomed Res Int. 2020;2020:1–7.
Verdecchia P, Reboldi GP, Gattobigio R, Bentivoglio M, Borgioni C, Angeli F, et al. Atrial fibrillation in hypertension: Predictors and outcome. Hypertension 2003;41:218–23.
Goda T, Sugiyama Y, Ohara N, Ikegami T, Watanabe K, Kobayashi J, et al. P-Wave Terminal Force in Lead V1 Predicts Paroxysmal Atrial Fibrillation in Acute Ischemic Stroke. J Stroke Cerebrovasc Dis. 2017;26:1912–5.
Baturova MA, Sheldon SH, Carlson J, Brady PA, Lin G, Rabinstein AA, et al. Electrocardiographic and Echocardiographic predictors of paroxysmal atrial fibrillation detected after ischemic stroke. BMC Cardiovasc Disord. 2016;16:1–8.
Platonov PG. Atrial conduction and atrial fibrillation: What can we learn from surface ECG? Rev Artic Cardiol J. 2008;15:402–7. www.cardiologyjournal.org.
Jurkko R, Väänänen H, Mäntynen V, Kuusisto J, Mäkijärvi M, Toivonen L. High-Resolution Signal-Averaged Analysis of Atrial Electromagnetic Characteristics in Patients with Paroxysmal Lone Atrial Fibrillation. Ann Noninvasive Electrocardiol. 2008;13:378–85.
Nemirovsky D, Hutter R, Anthony, Gomes J, the F, Weiner MA. The Electrical Substrate of Vagal Atrial Fibrillation as Assessed by the Signal-Averaged Electrocardiogram of the P Wave. PACE. 2008;31:308–13.
Lee DH, Lee KM, Yoon JM, Lim JW, Kho KO, Kil HR, et al. P wave dispersion on 12-lead electrocardiography in adolescents with neurocardiogenic syncope. Korean J Pediatr. 2016;59:451–5.
Öz A, Cinar T, Güler CK, Efe SÇ, Emre U, Karabǎ T, et al. Novel electrocardiography parameter for paroxysmal atrial fibrillation in acute ischaemic stroke patients: P wave peak time. Postgrad Med J. 2020;96:584–8.
Okutucu S, Aytemir K, Oto A. P-wave dispersion: What we know till now? JRSM Cardiovasc Dis. 2016;5:1–9.
Dilaveris PE, Gialafos EJ, Sideris SK, Theopistou AM, Andrikopoulos GK, Kyriakidis M, et al. Simple electrocardiography markers for the prediction of paroxysmal idiopathic atrial fibrillation. Am Heart J. 1998;135:734–8.
Cortez D, Baturova M, Lindgren A, Carlson J, Shubik YV, Olsson B, et al. Atrial time and voltage dispersion are both needed to predict new-onset atrial fibrillation in ischemic stroke patients. BMC Cardiovasc Disord. 2017;17:1–8.
Patrick DM, Van Beusecum JP, Kirabo A. The role of inflammation in hypertension: novel concepts. Curr Opin Physiol. 2021;19:92–8.
Goette A, Lendeckel U. Electrophysiological effects of angiotensin II. Part I: Signal transduction and basic electrophysiological mechanisms. Europace 2008;10:238–41.
De Mello WC. Intracellular Angiotensin II Regulates the Inward Calcium Current in Cardiac Myocytes. Hypertension. 1998;32:976–82. http://www.hypertensionaha.org.
Ferron L, Capuano V, Ruchon Y, Deroubaix E, Coulombe A, Renaud JF. Angiotensin II Signaling Pathways Mediate Expression of Cardiac T-Type Calcium Channels. Circ Res. 2003;93:1241–8.
Daleau P, Turgeon J. Angiotensin II modulates the delayed rectifier potassium current of guinea pig ventricular myocytes. Eur J Physiol. 1994;427:553–5.
Kumagai K, Nakashima H, Urata H, Gondo N, Arakawa K, Saku K. Effects of angiotensin II type 1 receptor antagonist on electrical and structural remodeling in atrial fibrillation. J Am Coll Cardiol. 2003;41:2197–204.
Chaugai S, Meng WY, Sepehry AA. Effects of RAAS blockers on atrial fibrillation prophylaxis: An updated systematic review and meta-analysis of randomized controlled trials. J Cardiovasc Pharm Ther. 2016;21:388–404.
Thomas MC, Dublin S, Kaplan RC, Glazer NL, Lumley T, Longstreth WT, et al. Blood pressure control and risk of incident atrial fibrillation. Am J Hypertens. 2008;21:1111–6.
Conen D, Tedrow UB, Koplan BA, Glynn RJ, Buring JE, Albert CM. Influence of systolic and diastolic blood pressure on the risk of incident atrial ribrillation in women. Circulation. 2009;119:2146–52.
Wuopio J, Orho-Melander M, Ärnlöv J, Nowak C. Estimated salt intake and risk of atrial fibrillation in a prospective community-based cohort. J Intern Med. 2021;289:700–8.
Jin MN, Yang PS, Song C, Yu HT, Kim TH, Uhm JS, et al. Physical Activity and Risk of Atrial Fibrillation: A Nationwide Cohort Study in General Population. Sci Rep. 2019;9:1–9.
Acknowledgements
We acknowledge I Made Junior Rina Artha, MD, PhD, FIHA, FAsCC, FAPSIC, FSCAI, FESC as our Head Department of Cardiology and Vascular Medicine, Prof. Dr. I.G.N.G Ngoerah General Hospital, Denpasar, Bali, Indonesia who gives us opportunity and general support to do this research.
Funding
All of financial on this manuscript was funded by author and co-author itself.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jagannatha, G.N.P., Antara, I.M.P.S., Kosasih, A.M. et al. P-wave peak time and P-wave dispersion in surface electrocardiography as initial predictors of new-onset atrial fibrillation in early-onset hypertension. Hypertens Res 47, 137–148 (2024). https://doi.org/10.1038/s41440-023-01357-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01357-0