Abstract
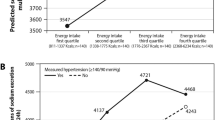
In Black populations excessive salt intake may exacerbate the genetic predisposition to hypertension and promote the early onset of cardiovascular disease. Ethnic differences in the interaction between sodium intake and the metabolome may play a part in hypertension and cardiovascular disease development. We determined (1) urinary amino acid and acylcarnitine profiles of young Black and White adults according to low, moderate, and high dietary salt intake, and (2) investigated the triad of salt intake, systolic blood pressure (SBP), and the associated metabolomics profile. This study included 447 White and 380 Black adults aged 20–30 years from the African-PREDICT study. Estimated salt intake was determined from 24-hour urinary sodium levels. Urinary amino acids and acylcarnitines were measured using liquid chromatography-tandem mass spectrometry. Black adults exhibited no significant differences in SBP, amino acids, or acylcarnitines across low (<5g/day), moderate (5–10g/day), and high (>10g/day) salt intake. White adults with a high salt intake had elevated SBP compared to those with low or moderate intakes (p < 0.001). Furthermore, gamma-aminobutyric acid (GABA) (q = 0.020), citrulline (q = 0.020), glutamic acid (q = 0.046), serine (q = 0.054) and proline (q = 0.054) were lowest in those with higher salt intake. Only in White and not Black adults did we observe inverse associations of clinic SBP with GABA (Adj. R2 = 0.34; Std. β = −0.133; p = 0.003), serine (Adj. R2 = 0.33; Std. β = −0.109; p = 0.014) and proline (Adj. R2 = 0.33; Std. β = −0.109; p = 0.014). High salt intake in White, but not in black adults, were related to metabolomic changes and may contribute to pathophysiological mechanisms associated with increased BP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982–3021.
Said MA, Verweij N, van der Harst P. Associations of combined genetic and lifestyle risks with incident cardiovascular disease and diabetes in the UK Biobank Study. JAMA Cardiol. 2018;3:693–702.
Qiao J, Lin X, Wu Y, Huang X, Pan X, Xu J, et al. Global burden of non-communicable diseases attributable to dietary risks in 1990-2019. J Hum Nutr Dietetics. 2022;35:202–13.
Schutte AE Ethnicity and cardiovascular disease. Textbook of Vascular Medicine: Springer; 2019. pp. 287-959
Elijovich F, Weinberger MH, Anderson CA, Appel LJ, Bursztyn M, Cook NR, et al. Salt sensitivity of blood pressure: a scientific statement from the American Heart Association. Hypertension. 2016;68:e7–e46.
Schutte AE, Botha S, Fourie CMT, Gafane-Matemane LF, Kruger R, Lammertyn L, et al. Recent advances in understanding hypertension development in sub-Saharan Africa. J Hum Hypertens. 2017;31:491–500.
He FJ, Tan M, Ma Y, MacGregor GA. Salt reduction to prevent hypertension and cardiovascular disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:632–47.
Chen L, He FJ, Dong Y, Huang Y, Wang C, Harshfield GA, et al. Modest sodium reduction increases circulating short-chain fatty acids in untreated hypertensives. Hypertension. 2020;76:73–9.
Derkach A, Sampson J, Joseph J, Playdon MC, Stolzenberg-Solomon RZ. Effects of dietary sodium on metabolites: the Dietary Approaches to Stop Hypertension (DASH)-Sodium Feeding Study. Am. Clin Nutr. 2017;106:1131–41.
Jablonski KL, Klawitter J, Chonchol M, Bassett CJ, Racine ML, Seals DR. Effect of dietary sodium restriction on human urinary metabolomic profiles. Clin J Am Soc Nephrol. 2015;10:1227–34.
Chen L, He FJ, Dong Y, Huang Y, Harshfield GA, Zhu H. Sodium reduction, metabolomic profiling, and cardiovascular disease risk in untreated black hypertensives. Hypertension. 2019;74:194–200.
Schutte AE, Gona PN, Delles C, Uys AS, Burger A, Mels CM, et al. The African Prospective study on the Early Detection and Identification of Cardiovascular disease and Hypertension (African-PREDICT): Design, recruitment and initial examination. Eur. J Prev Cardiol. 2019;26:458–70.
WHO/PAHO Regional Expert Group for Cardiovascular Disease Prevention through Population‐wide Dietary Salt Reduction. Protocol for population level sodium determination in 24‐hour urine samples. World Health Organization Geneva, Switzerland; 2010.
Stevens LA, Claybon MA, Schmid CH, Chen J, Horio M, Imai E, et al. Evaluation of the Chronic Kidney Disease Epidemiology Collaboration equation for estimating the glomerular filtration rate in multiple ethnicities. Kidney Int. 2011;79:555–62.
Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerová J, Richart T, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305:1777–85.
Strauss-Kruger M, Kruger R, Jansen Van Vuren E, Jacobs A, Louw R, Mels C Identifying a metabolomics profile associated with masked hypertension in two independent cohorts: Data from the African-PREDICT and SABPA studies. Hypertension Research 2022; https://doi.org/10.1038/s41440-022-01010-2.
World Health Organization. Guideline: Sodium intake for adults and children. World Health Organization; 2012.
Paapstel K, Kals J. Metabolomics of arterial stiffness. Metabolites. 2022;1212:370 https://doi.org/10.3390/metabo12050370.
Breet Y, Huisman HW, Kruger R, Van Rooyen JM, Gafane-Matemane LF, Ware LJ, et al. Pulse pressure amplification and its relationship with age in young, apparently healthy black and white adults: the African-PREDICT study. 2017; 249:387-91.
Mokwatsi GG, Schutte AE, Kruger R. Ethnic differences regarding arterial stiffness of 6‐8‐year-old black and white boys. J Hypertens. 2017;35:960–67.
Erasmus D, Mels CM, Louw R, Lindeque JZ, Kruger RJP. Urinary metabolites and their link with premature arterial stiffness in black boys: the ASOS study. Pulse. 2018;6:144–53.
Rédei GP Glucogenic Amino Acids. In: Rédei GP, editor. Encyclopedia of genetics, genomics, proteomics and informatics. Dordrecht: Springer; 2008. p. 803.
Chung ST, Hsia DS, Chacko SK, Rodriguez LM, Haymond MW. Increased gluconeogenesis in youth with newly diagnosed type 2 diabetes. Diabetologia. 2015;58:596–603.
Chung ST, Courville AB, Onuzuruike AU, Galvan-De La Cruz M, Mabundo LS, DuBose CW, et al. Gluconeogenesis and risk for fasting hyperglycemia in Black and White women. JCI insight. 2018;3:e121495.
Balakrishna Y, Manda S, Mwambi H, van Graan A. Identifying nutrient patterns in south african foods to support national nutrition guidelines and policies. Nutrients. 2021;13:3194.
Carmichael CY, Wainford RD. Hypothalamic signaling mechanisms in hypertension. Curr Hypertens Rep. 2015;17:39.
Ngo D-H, Vo TS. An updated review on pharmaceutical properties of gamma-aminobutyric acid. Molecules. 2019;24:2678.
Stamler J, Brown IJ, Daviglus ML, Chan Q, Kesteloot H, Ueshima H, et al. Glutamic acid, the main dietary amino acid, and blood pressure: the INTERMAP Study (International Collaborative Study of Macronutrients, Micronutrients and Blood Pressure). Circulation. 2009;120:221–8.
Jennings A, MacGregor A, Welch A, Chowienczyk P, Spector T, Cassidy A. Amino acid intakes are inversely associated with arterial stiffness and central blood pressure in women. J Nutr. 2015;145:2130–8.
McGee MA, Abdel-Rahman AA. N-Methyl-D-Aspartate receptor signaling and function in cardiovascular tissues. J Cardiovasc Pharm. 2016;68:97–105.
Shabeeh H, Khan S, Jiang B, Brett S, Melikian N, Casadei B, et al. Blood pressure in healthy humans is regulated by neuronal NO synthase. Hypertension. 2017;69:970–6.
Dietrich S, Floegel A, Weikert C, Prehn C, Adamski J, Pischon T, et al. Identification of serum metabolites associated with incident hypertension in the European Prospective Investigation Into Cancer and Nutrition-Potsdam Study. Hypertension. 2016;68:471–7.
Louca P, Nogal A, Moskal A, Goulding NJ, Shipley MJ, Alkis T, et al. Cross-sectional blood metabolite markers of hypertension: a multicohort analysis of 44,306 individuals from the COnsortium of METabolomics Studies. Metabolites. 2022;12:601.
Maralani MN, Movahedian A, Javanmard Sh H. Antioxidant and cytoprotective effects of L-Serine on human endothelial cells. Res Pharm Sci. 2012;7:209–15.
Teymoori F, Asghari G, Farhadnejad H, Nazarzadeh M, Atifeh M, Mirmiran P, et al. Various proline food sources and blood pressure: substitution analysis. Int J Food Sci Nutr. 2019;71:1–9.
Karna E, Szoka L, Huynh TYL, Palka JA. Proline-dependent regulation of collagen metabolism. Cell Mol Life Sci. 2020;77:1911–8.
Charlton KE, Schutte AE, Wepener L, Corso B, Kowal P, Ware LJ. Correcting for intra-individual variability in sodium excretion in spot urine samples does not improve the ability to predict 24 h urinary sodium excretion. Nutrients. 2020;12:2026.
Acknowledgements
The authors are grateful to all individuals who voluntarily participated in the African-PREDICT study. The dedication of the support and research staff as well as students at the Hypertension Research and Training Clinic at the North-West University are also duly acknowledged.
Funding
The research funded in this manuscript is part of an ongoing larger research project financially supported by the South African Medical Research Council (SAMRC) with funds from National Treasury under its Economic Competitiveness and Support Package; the South African Research Chairs Initiative (SARChI) of the Department of Science and Technology and National Research Foundation (NRF) of South Africa (GUN 86895); SAMRC with funds received from the South African National Department of Health, GlaxoSmithKline R&D (Africa Non-Communicable Disease Open Lab grant), the UK Medical Research Council and with funds from the UK Government’s Newton Fund; and corporate social investment grants from Pfizer (South Africa), Boehringer-Ingelheim (South Africa), Novartis (South Africa), the Medi Clinic Hospital Group (South Africa) and in-kind contributions of Roche Diagnostics (South Africa). This work is based on the research supported in part by the NRF of South Africa (Grant Number: UID: 138499). Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors, and therefore, the NRF does not accept any liability in this regard.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
TvZ, MP, RK, LGM, GM, HM, AJ, RL and CM reported no COI. Honoraria (lecture fees): AES (Abbott, Servier); Research Funding: AES (Medical Research Future Fund, Australia). Scholarship or donation: MSK (Postdoctoral grant from the National Research Foundation, South Africa).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Strauss-Kruger, M., van Zyl, T., Pieters, M. et al. Urinary metabolomics, dietary salt intake and blood pressure: the African-PREDICT study. Hypertens Res 46, 175–186 (2023). https://doi.org/10.1038/s41440-022-01071-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01071-3