Abstract
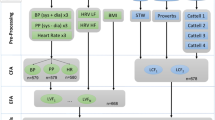
Hypertension is one of the most prevalent chronic conditions and has been proven to be related to cognitive function. However, there is no evidence regarding the heterogeneity in cognitive trajectories among persons with hypertension. The aims of the current study were to characterize the heterogeneity in longitudinal trajectories of cognitive performance among Chinese middle-aged and older individuals with hypertension and to explore the potential determinants of trajectory memberships. Data from the 2011 to 2018 Chinese Health and Retirement Longitudinal Study (CHARLS) were utilized. Two cognitive measures of executive function and episodic memory were assessed, and conditional growth mixture modeling (GMM) was performed to identify the trajectories of cognitive performance and explore the related factors of cognitive change. The findings revealed three trajectory classes of executive function (stable, sharp decline, smooth decline) and two trajectory classes of episodic memory (stable, decline). Individuals with hypertension who had a higher educational level, moderate nighttime sleep duration, and lower depressive symptoms as well as those who reported consuming alcohol at least once a month were more likely to belong to the optimal stable executive function group. Subjects with a higher educational level, adequate daytime napping duration, and higher BMI were more likely to exhibit stable episodic memory over time. Other factors, including age, sex, community type, marital status, and hypertension treatment, exhibited class-specific effects on growth parameters of cognitive trajectory. Targeting intervention designation is proposed to ameliorate the burdens of cognitive impairment among individuals with hypertension.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Okusaga O, Stewart MCW, Butcher I, Deary I, Fowkes FGR, Price JF. Smoking, hypercholesterolaemia and hypertension as risk factors for cognitive impairment in older adults. Age Ageing. 2013;42:306–11.
Elias MF, Goodell AL, Dore GA. Hypertension and cognitive functioning a perspective in historical context. Hypertension. 2012;60:260–8.
Leys D, Hénon H, Mackowiak-Cordoliani M-A, Pasquier F. Poststroke dementia. Lancet Neurol. 2005;4:752–9.
Uiterwijk R, Huijts M, Staals J, Duits A, Gronenschild E, Kroon AA, et al. Subjective cognitive failures in patients with hypertension are related to cognitive performance and cerebral microbleeds. Hypertension 2014;64:653–7.
Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10:819–28.
Johnson KC, Margolis KL, Espeland MA, Colenda CC, Fillit H, Manson JE, et al. A prospective study of the effect of hypertension and baseline blood pressure on cognitive decline and dementia in postmenopausal women: the Women’s Health Initiative Memory Study. J Am Geriatr Soc. 2010;56:1449–58.
Gombojav B, Yi S-W, Sull JW, Nam CM, Ohrr H. Combined effects of cognitive impairment and hypertension on total mortality in elderly people: The Kangwha Cohort study. Gerontology. 2011;57:490–6.
Yano Y, Bakris GL, Inokuchi T, Ohba Y, Tamaki N, Nagata M, et al. Association of cognitive dysfunction with cardiovascular disease events in elderly hypertensive patients. J Hypertens. 2014;32:423–31.
Cho MH, Shin DW, Chang S-A, Lee JE, Jeong S-M, Kim SH, et al. Association between cognitive impairment and poor antihypertensive medication adherence in elderly hypertensive patients without dementia. Sci Rep. 2018;8:11688.
Liu H-Y, Tsai W-C, Chiu M-J, Tang L-Y, Lee H-J, Shyu Y-I. L Mild cognitive impairment in combination with comorbid diabetes mellitus and hypertension is negatively associated with health-related quality of life among older persons in Taiwan. Qual Life Res. 2019;28:1281–91.
Vinyoles E, Figuera MDL, Gonzalez-Segura D. Cognitive function and blood pressure control in hypertensive patients over 60 years of age: COGNIPRES study. Curr Med Res Opin. 2008;24:3331–9.
Alakuş F, Helvaci A, Temizel M, Arman Y. Estimation of cognitive functions and effective factors in middle and advance aged hypertensive patients. J Am Coll Cardiol. 2013;62:C87–C88. Supplement 2.
Pál T, Marta GS, Nemes-Nagy E, Baróti B, Tripon R, Csomay K, et al. Relationship between obesity and cognitive function in middle-aged and elderly hypertensive patients. J Hypertens. 2019;37:e275.
Frith E, Loprinzi PD. Physical activity and cognitive function among older adults with hypertension. J Hypertens. 2017;35:1271–5.
Sakakura K, Hoshide S, Ishikawa J, Momomura S-i, Kawakami M, Shimada K, et al. Association of body mass index with cognitive function in elderly hypertensive Japanese. Am J Hypertens. 2008;21:627–32.
Zuo M, Gan C, Liu T, Tang J, Dai J, Hu X. Physical predictors of cognitive function in individuals with hypertension: Evidence from the CHARLS basline survey. West J Nurs Res. 2019;41:592–614.
Pál T, Preg Z, Bálint-Szentendrey D, Salló ZG, Márton HZ, Nagy EN, et al. Which cognitive domains are affected in hypertensive patients? An analysis according to age, sex, depression and comorbidities. J Hypertens. 2018;36:e89. Supplement 1.
Cervilla JA, Prince M, Joels S, Lovestone S, Mann A. Long-term predictors of cognitive outcome in a cohort of older people with hypertension. Br J Psychiatry. 2000;177:66–71.
Vicario A, Sueldo MAD, Zilberman JM, Cerezo GH. Cognitive evolution in hypertensive patients: A six-year follow-up. Vasc health risk Manag. 2011;7:281–5.
Zhang J, Tang G, Xie H, Wang B, He M, Fu J, et al. Higher adiposity is associated with slower cognitive decline in hypertensive patients: Secondary analysis of the china stroke primary prevention trial. J Am Heart Assoc. 2017;6:e005561.
Desjardins-Crépeau L. Bherer L, Hypertension and Age-Related Cognitive Decline, In Hypertension and the Brain as an End-Organ Target. 2016, Springer International Publishing. p. 21–38.
Nagin D. Group-Based Modeling of Development. 2005: Harvard University Press.
Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass. 2010;2:302–17.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: The China health and retirement longitudinal study (CHARLS). Int J Epidemiol. 2014;63:61–8.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: Data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet Neurol. 2017;390:2549–58.
Song H, Feng D, Wang R, Tang S, Ghose B, Li G, et al. Urban-rural disparity in the utilization of national community-based hypertension monitoring service-results from the China Health and Retirement Longitudinal Study, 2015. Peer J. 2019;15:e7842.
Lei X, Hu Y, McArdle JJ, Smith JP, Zhao Y. Gender differences in cognition among older adults in China. J Hum Resour. 2012;47:951–71.
Sha T, Cheng W, Yan Y. Prospective association between sleep-related factors and the trajectories of cognitive performance in the elderly Chinese population across a 5-year period cohort study. PLoS ONE. 2019;14:e0222192.
Beeri MS, Werner P, Davidson M, Schmidler J, Silverman J. Validation of the modified telephone interview for cognitive status (TICS-m) in Hebrew. Int J Geriatr Psychiatry. 2003;18:381–6.
McArdle JJ, Fisher GG, Kadlec KM. Latent variable analyses of age trends of cognition in the health and retirement study, 1992-2004. Psychology. Aging. 2007;22:525–45.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Preventive Med. 1994;10:77–84.
Clark SL, Muthén B. Relating latent class analysis results to variables not included in the analysis. Submitted Publ. 2009;21:402.
Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol Meth. 2002;7:147–77.
Asparouhov T, Muthén B. Using Mplus TECH11 and TECH14 to test the number of latent classes (Mplus Web Notes No. 14). 2012.Retrieved from http://www.statmodel.com/examples/webnotes/webnote14.pdf.
Palta P, Albert MS, Gottesman RF. Heart health meets cognitive health: Evidence on the role of blood pressure. Lancet Neurol. 2021;20:854–67.
Yu W, Chen R, Zhang M, Li Z, Gao F, Yu S, et al. Cognitive decline trajectories and influencing factors in China: A non-normal growth mixture model analysis. Arch Gerontol Geriatrics. 2021;95:104381.
Whalley LJ, Deary IJ, Appleton CL, Starr JM. Cognitive reserve and the neurobiology of cognitive aging. Ageing Res Rev. 2004;3:369–82.
Bruandet A, Richard F, Bombois S, Maurage CA, Masse I, Amouyel P, et al. Cognitive decline and survival in Alzheimer’s disease according to education level. Dement Geriatr Cogn Disord. 2008;25:74–80.
Xu H, Dupre ME, Østbye T, Vorderstrasse AA, Wu B. Residential mobility and cognitive function among middle-aged and older adults in China. Res Aging. 2018;41:3–30.
Gildner TE, Salinas-Rodríguez A, Manrique-Espinoza B, Moreno-Tamayo K, Kowal P. Does poor sleep impair cognition during aging? Longitudinal associations between changes in sleep duration and cognitive performance among older Mexican adults. Archives of Gerontology. Geriatrics. 2019;83:161–8.
Ma Y, Liang L, Zheng F, Shi L, Zhong B, Xie W. Association between sleep duration and cognitive decline. JAMA Netw Open. 2020;3:e2013573.
Scullin MK, Fairley J, Decker MJ, Bliwise DL. The effects of an afternoon nap on episodic memory in young and older adults. Sleep. 2017;40:zsx035.
Poluektov MG, Narbut AM, Dorokhov VB. Daytime napping and its effects on memory consolidation. Zh nevrologii i psikhiatrii Im S S Korsakova. 2020;120:127–32.
Basta M, Koutentaki E, Vgontzas A, Zaganas I, Vogiatzi E, Gouna G, et al. Objective daytime napping is associated with disease severity and inflammation in patients with mild to moderate dementia1. J Alzheimer’s Dis. 2020;74:803–15.
Paolillo EW, Pasipanodya EC, Moore RC, Pence BW, Atkinson JH, Grelotti DJ, et al. Cumulative burden of depression and neurocognitive decline among persons with HIV: A longitudinal study. J Acquir Immun Defic Syndr. 2020;84:304–12.
Acknowledgements
We thank all the participants involved in the survey design and data collection and the CHARLS research team for collecting high-quality, nationally representative data and making the data public.
Author information
Authors and Affiliations
Contributions
Conceptualization: BZ and SJ; Methodology, BZ; software, BZ, Formal analysis, BZ and SJ; writing—original draft preparation, BZ; writing—review and editing, BZ and SJ.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhang, B., Jiang, S. Heterogeneity in longitudinal trajectories of cognitive performance among middle-aged and older individuals with hypertension: Growth mixture modeling across an 8-year cohort study. Hypertens Res 45, 1037–1046 (2022). https://doi.org/10.1038/s41440-021-00829-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00829-5
Keywords
This article is cited by
-
Obstructive sleep apnea and non-dipper: epiphenomena or risks of Alzheimer’s disease?: a review from the HOPE Asia Network
Hypertension Research (2023)
-
The Association of Age at Diagnosis of Hypertension with Cognitive Decline: the China Health and Retirement Longitudinal Study (CHARLS)
Journal of General Internal Medicine (2023)
-
Association between Sarcopenia and Cognitive Trajectories among Middle-Aged and Older Adults in China: A Nationally Representative Cohort Study
The journal of nutrition, health & aging (2023)
-
Hypertension management to prevent dementia
Hypertension Research (2022)
-
Is it possible to prevent cognitive decline among middle-aged and older hypertensive individuals?
Hypertension Research (2022)