Abstract
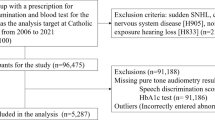
This retrospective longitudinal study examined the association between systolic blood pressure and hearing impairment among 13,187 Japanese individuals (men, 46.5%) aged 20–59 years. The systolic blood pressure of participants was categorized as <120, 120–129, 130–139, 140–149, 150–159, and ≥160 mmHg. Using pure-tone audiometry, hearing impairment at 1 and 4 kHz was defined as hearing thresholds in either ear >30 and >40 dB, respectively. We performed multivariable Cox proportional-hazards regression analysis to examine the association using two multiple-imputation methods (fully conditional specification and Markov chain Monte Carlo). There were 695 and 774 hearing-impairment cases at 1 and 4 kHz, respectively, during ~77,000 person-years of follow-up. Compared with the <120 mmHg group, the hazard ratios (95% confidence intervals) of hearing impairment for the 120–129, 130–139, 140–149, 150–159, and ≥160 mmHg groups after adjustment for age, sex, body mass index, high serum glucose, current smoking, and other potential confounders were 1.35 (1.12–1.63), 1.45 (1.13–1.86), 1.07 (0.73–1.58), 1.91 (1.18–3.07), and 1.81 (1.01–3.25), respectively, at 1 kHz using the first imputation method; 1.36 (1.13–1.63), 1.48 (1.17–1.86), 1.09 (0.76–1.58), 1.99 (1.29–3.06), and 1.92 (1.08–3.41), respectively, at 1 kHz using the second imputation method; 1.04 (0.86–1.24), 1.14 (0.91–1.43), 1.13 (0.83–1.54), 1.45 (0.96–2.19), and 1.35 (0.82–2.23), respectively, at 4 kHz using the first imputation method; and 1.03 (0.86–1.24), 1.17 (0.95–1.44), 1.15 (0.87–1.53), 1.54 (1.06–2.24), and 1.44 (0.88–2.35), respectively, at 4 kHz using the second imputation method. In conclusion, higher systolic blood pressure was associated with hearing impairment at 1 kHz. No clear association was observed at 4 kHz.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Walling AD, Dickson GM. Hearing loss in older adults. Am Fam Physician. 2012;85:1150–6.
Contrera KJ, Wallhagen MI, Mamo SK, Oh ES, Lin FR. Hearing loss health care for older adults. J Am Board Fam Med. 2016;29:394–403. https://doi.org/10.3122/jabfm.2016.03.150235.
Cunningham LL, Tucci DL. Hearing loss in adults. N. Engl J Med. 2017;377:2465–73. https://doi.org/10.1056/NEJMra1616601.
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global burden of disease study 2017. Lancet. 2018;392:1789–858. https://doi.org/10.1016/S0140-6736(18)32279-7.
World Health Organization. Global costs of unaddressed hearing loss and cost-effectiveness of interventions: a WHO report, 2017. https://apps.who.int/iris/handle/10665/254659. Accessed 8 January 2021.
Przewoźny T, Gójska-Grymajło A, Kwarciany M, Gąsecki D, Narkiewicz K. Hypertension and cochlear hearing loss. Blood Press. 2015;24:199–205. https://doi.org/10.3109/08037051.2015.1049466.
Oron Y, Elgart K, Marom T, Roth Y. Cardiovascular risk factors as causes for hearing impairment. Audio Neurootol. 2014;19:256–60. https://doi.org/10.1159/000363215.
Umesawa M, Sairenchi T, Haruyama Y, Nagao M, Kobashi G. Association between hypertension and hearing impairment in health check-ups among Japanese workers: a cross-sectional study. BMJ Open. 2019;9:e028392. https://doi.org/10.1136/bmjopen-2018-028392.
Lasisi AO, Abiona T, Gureje O. The prevalence and correlates of self-reported hearing impairment in the Ibadan study of ageing. Trans R Soc Trop Med Hyg. 2010;104:518–23. https://doi.org/10.1016/j.trstmh.2010.03.009.
Lin BM, Curhan SG, Wang M, Eavey R, Stankovic KM, Curhan GC. Hypertension, diuretic use, and risk of hearing loss. Am J Med. 2016;129:416–22. https://doi.org/10.1016/j.amjmed.2015.11.014.
Shargorodsky J, Curhan SG, Eavey R, Curhan GC. A prospective study of cardiovascular risk factors and incident hearing loss in men. Laryngoscope. 2010;120:1887–91. https://doi.org/10.1002/lary.21039.
Brant LJ, Gordon-Salant S, Pearson JD, Klein LL, Morrell CH, Metter EJ, et al. Risk factors related to age-associated hearing loss in the speech frequencies. J Am Acad Audio. 1996;7:152–60.
Rolim LP, Samelli AG, Moreira RR, Matas CG, Santos IS, Bensenor IM, et al. Effects of diabetes mellitus and systemic arterial hypertension on elderly patients’ hearing. Braz J Otorhinolaryngol. 2018;84:754–63. https://doi.org/10.1016/j.bjorl.2017.08.014.
Reed NS, Huddle MG, Betz J, Power MC, Pankow JS, Gottesman R, et al. Association of midlife hypertension with late-life hearing loss. Otolaryngol Head Neck Surg. 2019;161:996–1003. https://doi.org/10.1177/0194599819868145.
Linssen AM, van Boxtel MP, Joore MA, Anteunis LJ. Predictors of hearing acuity: cross-sectional and longitudinal analysis. J Gerontol A Biol Sci Med Sci. 2014;69:759–65. https://doi.org/10.1093/gerona/glt172.
Olusanya BO, Davis AC, Hoffman HJ. Hearing loss grades and the International classification of functioning, disability and health. Bull World Health Organ. 2019;97:725–8. https://doi.org/10.2471/BLT.19.230367.
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes–2018. Diabetes Care. 2018;41:S13–S27. https://doi.org/10.2337/dc18-S002.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. American college of cardiology/American heart association task force on practice guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. 2014;129:S1–45. https://doi.org/10.1161/01.cir.0000437738.63853.7a.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Hypertension. 2018;71:e13–e115. https://doi.org/10.1161/HYP.0000000000000065.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. List of authors/task force members:. 2018 practice guidelines for the management of arterial hypertension of the European society of hypertension and the European society of cardiology: ESH/ESC task force for the management of arterial hypertension. J Hypertens. 2018;36:2284–309. https://doi.org/10.1097/HJH.0000000000001961.
van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16:219–42. https://doi.org/10.1177/0962280206074463.
Schafer JL. Analysis of incomplete multivariate data. Chapman & Hall: London, UK 1997.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–99. https://doi.org/10.1002/sim.4067.
Rubin DB. Multiple Imputation for Nonresponse in Surveys. Wiley: New York, USA, 1987.
Tachibana M, Yamamichi I, Nakae S, Hirasugi Y, Machino M, Mizukoshi O. The site of involvement of hypertension within the cochlea. a comparative study of normotensive and spontaneously hypertensive rats. Acta Otolaryngol. 1984;97:257–65. https://doi.org/10.3109/00016488409130987.
Makishima K. Arteriolar sclerosis as a cause of presbycusis. Otolaryngology. 1978;86:ORL322–326. https://doi.org/10.1177/019459987808600225.
McCormick JG, Harris DT, Hartley CB, Lassiter RB. Spontaneous genetic hypertension in the rat and its relationship to reduced ac cochlear potentials: implications for preservation of human hearing. Proc Natl Acad Sci USA. 1982;79:2668–72. https://doi.org/10.1073/pnas.79.8.2668.
Ikeda K, Morizono T. Electrochemical profiles for monovalent ions in the stria vascularis: cellular model of ion transport mechanisms. Hear Res. 1989;39:279–86. https://doi.org/10.1016/0378-5955(89)90047-6.
Yamasoba T, Lin FR, Someya S, Kashio A, Sakamoto T, Kondo K. Current concepts in age-related hearing loss: epidemiology and mechanistic pathways. Hear Res. 2013;303:30–8. https://doi.org/10.1016/j.heares.2013.01.021.
Scherer EQ, Arnold W, Wangemann P. Pharmacological reversal of endothelin-1 mediated constriction of the spiral modiolar artery: a potential new treatment for sudden sensorineural hearing loss. BMC Ear Nose Throat Disord. 2005;5:10. https://doi.org/10.1186/1472-6815-5-10.
Yasuda H, Kamide K, Takiuchi S, Matayoshi T, Hanada H, Kada A, et al. Association of single nucleotide polymorphisms in endothelin family genes with the progression of atherosclerosis in patients with essential hypertension. J Hum Hypertens. 2007;21:883–92. https://doi.org/10.1038/sj.jhh.1002234.
Uchida Y, Sugiura S, Ando F, Nakashima T, Shimokata H. Molecular genetic epidemiology of age-related hearing impairment. Auris Nasus Larynx. 2011;38:657–65. https://doi.org/10.1016/j.anl.2011.02.005.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective studies collaboration. age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. https://doi.org/10.1016/s0140-6736(02)11911-8.
Han M, Li Q, Liu L, Zhang D, Ren Y, Zhao Y, et al. Prehypertension and risk of cardiovascular diseases: a meta-analysis of 47 cohort studies. J Hypertens. 2019;37:2325–32. https://doi.org/10.1097/HJH.0000000000002191.
Passchier-Vermeer W, Passchier WF. Noise exposure and public health. Environ Health Perspect. 2000;108:123–31. https://doi.org/10.1289/ehp.00108s1123.
Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and non-auditory effects of noise on health. Lancet. 2014;383:1325–32. https://doi.org/10.1016/S0140-6736(13)61613-X.
Acknowledgements
We thank Satoshi Hattori, Ph.D., Sho Komukai, Ph.D., and Rei Monden, Ph.D. (Department of Biomedical Statistics, Osaka University Graduate School of Medicine, respectively), for their valuable advice on statistical analysis, and our colleagues from Osaka University Center of Medical Data Science, Advanced Clinical Epidemiology Investigator’s Research Project for providing their insight and expertise for our research. We are grateful to all the staff, particularly to Hirokazu Takeda, health information manager (Keiju Health Management Center), and Asako Izumiya, M.D. (Keiju Health Management Center), in Keiju Medical Center, Nanao, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Miyata, J., Umesawa, M., Yoshioka, T. et al. Association between high systolic blood pressure and objective hearing impairment among Japanese adults: a facility-based retrospective cohort study. Hypertens Res 45, 155–161 (2022). https://doi.org/10.1038/s41440-021-00737-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00737-8
Keywords
This article is cited by
-
Effects of cooking with solid fuel on hearing loss in Chinese adults—Based on two cohort studies
Scientific Reports (2024)
-
Hypertension facilitates age-related diseases. ~ Is hypertension associated with a wide variety of diseases?~
Hypertension Research (2024)
-
Hypertension and the development of hearing loss
Hypertension Research (2022)