Abstract
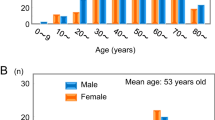
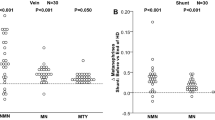
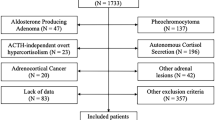
Urinary measurement of fractionated metanephrines is one of the best available biochemical tests for the diagnosis of pheochromocytoma and paraganglioma; however, false-positive results remain an issue. In addition, despite their convenience, there is no evidence to suggest that spot urine samples should replace the standard 24-h urine collection method. The objective of this study is to elucidate clinical variables that may influence the levels of spot urine fractionated metanephrines and to examine their instability. The study is a retrospective review of prospectively collected data from 949 patients whose spot urine fractionated metanephrines were measured under suspicion of pheochromocytoma or paraganglioma at our institution from January 2011 to June 2017. The effects of clinical factors such as age, sex, renal function, and medications on the level of spot urine fractionated metanephrines were evaluated. Urinary fractionated metanephrines were significantly higher in female subjects. They correlated with age but not with estimated glomerular filtration rate (eGFR). A multivariate regression model for urinary fractionated metanephrine levels revealed that age, female sex, eGFR, and the presence of α1-blocker medication were significantly positively correlated with urinary metanephrine (M) levels. Age, female sex, eGFR, and presence of α1-blockers and antidepressant and antipsychotic medications positively correlated with urinary normetanephrine (NM). In addition, age, female sex, eGFR, and presence of α1-blockers and antidepressant and antipsychotic medications were positively correlated with urinary M + NM. In conclusion, sex, age, eGFR, and treatment with α1-blockers, antidepressants, and antipsychotics may affect the levels of urinary fractionated metanephrines. When assessing urinary fractionated metanephrines in patients with suspected PPGLs, we must consider these factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Lenders JW, Eisenhofer G, Armando I, Keiser HR, Goldstein DS, Kopin IJ. Determination of metanephrines in plasma by liquid chromatography with electrochemical detection. Clin Chem. 1993;39:97–103.
Eisenhofer G, Goldstein DS, Walther MM, Friberg P, Lenders JW, Keiser HR, et al. Biochemical diagnosis of pheochromocytoma: how to distinguish true- from false-positive test results. J Clin Endocrinol Metab. 2003;88:2656–66.
Davidson DF. Phaeochromocytoma with normal urinary catecholamines: the potential value of urinary free metadrenalines. Ann Clin Biochem. 2002;39:557–66.
Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99:1915–42.
Lenders JW, Pacak K, Walther MM, Linehan WM, Mannelli M, Friberg P, et al. Biochemical diagnosis of pheochromocytoma: which test is best? J Am Med Assoc. 2002;287:1427–34.
Sawka AM, Jaeschke R, Singh RJ, Young WF Jr. A comparison of biochemical tests for pheochromocytoma: measurement of fractionated plasma metanephrines compared with the combination of 24-hour urinary metanephrines and catecholamines. J Clin Endocrinol Metab. 2003;88:553–8.
Manger WM, Gifford RW. Pheochromocytoma. J Clin hypertension. 2002;4:62–72.
Sinclair AM, Isles CG, Brown I, Cameron H, Murray GD, Robertson JW. Secondary hypertension in a blood pressure clinic. Arch Intern Med. 1987;147:1289–93.
Anderson GH Jr., Blakeman N, Streeten DH. The effect of age on prevalence of secondary forms of hypertension in 4429 consecutively referred patients. J Hypertens. 1994;12:609–15.
Ariton M, Juan CS, AvRuskin TW. Pheochromocytoma: clinical observations from a Brooklyn tertiary hospital. Endocr Pract. 2000;6:249–52.
Omura M, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T. Prospective study on the prevalence of secondary hypertension among hypertensive patients visiting a general outpatient clinic in Japan. Hypertension Res. 2004;27:193–202.
Goldstein DS, Lake CR, Chernow B, Ziegler MG, Coleman MD, Taylor AA, et al. Age-dependence of hypertensive-normotensive differences in plasma norepinephrine. Hypertension. 1983;5:100–4.
Poehlman ET, Gardner AW, Goran MI, Arciero PJ, Toth MJ, Ades PA, et al. Sympathetic nervous system activity, body fatness, and body fat distribution in younger and older males. J Appl Physiol. 1995;78:802–6.
Iwase S, Mano T, Watanabe T, Saito M, Kobayashi F. Age-related changes of sympathetic outflow to muscles in humans. J Gerontol. 1991;46:M1–5.
Marker JC, Cryer PE, Clutter WE. Simplified measurement of norepinephrine kinetics: application to studies of aging and exercise training. Am J Physiol. 1994;267:E380–387.
Seals DR, Esler MD. Human ageing and the sympathoadrenal system. J Physiol. 2000;528:407–17.
Becker LC, Pepine CJ, Bonsall R, Cohen JD, Goldberg AD, Coghlan C, et al. Left ventricular, peripheral vascular, and neurohumoral responses to mental stress in normal middle-aged men and women. Reference Group for the Psychophysiological Investigations of Myocardial Ischemia (PIMI) Study. Circulation. 1996;94:2768–77.
Owens JF, Stoney CM, Matthews KA. Menopausal status influences ambulatory blood pressure levels and blood pressure changes during mental stress. Circulation. 1993;88:2794–802.
Komesaroff PA, Esler MD, Sudhir K. Estrogen supplementation attenuates glucocorticoid and catecholamine responses to mental stress in perimenopausal women. J Clin Endocrinol Metab. 1999;84:606–10.
Lindheim SR, Legro RS, Bernstein L, Stanczyk FZ, Vijod MA, Presser SC, et al. Behavioral stress responses in premenopausal and postmenopausal women and the effects of estrogen. Am J Obstet Gynecol. 1992;167:1831–6.
Niculescu DA, Ismail G, Poiana C. Plasma free metanephrine and normetanephrine levels are increased in patients with chronic kidney disease. Endocr Pract. 2014;20:139–44.
Neumann J, Ligtenberg G, Klein II, Koomans HA, Blankestijn PJ. Sympathetic hyperactivity in chronic kidney disease: pathogenesis, clinical relevance, and treatment. Kidney Int. 2004;65:1568–76.
Esler MD, Wallin G, Dorward PK, Eisenhofer G, Westerman R, Meredith I, et al. Effects of desipramine on sympathetic nerve firing and norepinephrine spillover to plasma in humans. Am J Physiol. 1991;260:R817–23.
Veith RC, Lewis N, Linares OA, Barnes RF, Raskind MA, Villacres EC, et al. Sympathetic nervous system activity in major depression. Basal and desipramine-induced alterations in plasma norepinephrine kinetics. Arch Gen Psychiatry. 1994;51:411–22.
Neary NM, King KS, Pacak K. Drugs and pheochromocytoma–don’t be fooled by every elevated metanephrine. N. Engl J Med. 2011;364:2268–70.
Acknowledgements
This study was supported in part by a JSPS KAKENHI Grant Number 16H05316 to AI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bokuda, K., Yatabe, M., Seki, Y. et al. Clinical factors affecting spot urine fractionated metanephrines in patients suspected pheochromocytoma/paraganglioma. Hypertens Res 43, 543–549 (2020). https://doi.org/10.1038/s41440-020-0406-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-020-0406-4
Key words
This article is cited by
-
Predictive model of pheochromocytoma based on the imaging features of the adrenal tumours
Scientific Reports (2022)