Abstract
Hypertension is the major cause of preventable disease burden in China. However, limited evidence is available on sex differences in the awareness, treatment, and control of hypertension. We assessed sex differences in the awareness, treatment, and control of hypertension in China. A systematic search of four English language and four Chinese-language databases was conducted to identify studies conducted from 2005 that reported sex-specific data on the awareness, treatment, and control of hypertension in China. Random-effects meta-analysis weighted by the inverse of the variances were used to obtain pooled sex-specific rates and women-minus-men differences, and their 95% confidence intervals (CI). Overall, 57 studies comprising 2,155,829 individuals (55% women) were included. Awareness (53% in women vs. 47% in men), treatment among all (44% vs. 38%), treatment among aware (65% vs. 60%), control among all (17% vs. 14%), and control among treated (27% vs. 27%) were low for both sexes, but more favourable in women than men. The corresponding women-minus men difference was 7% (95% CI: 6; 8%) for awareness, 6% (5; 8%) for treatment among all, 6% (2; 9%) for treatment among aware, 3% (2; 3%) for control among all, and 0% (−2; 1%) for control among treated. Awareness, treatment, and control of hypertension in China is low in both sexes, but greater in women than men. Sex-specific interventions may be needed to efficiently combat the burden of hypertension.
Similar content being viewed by others
Introduction
Hypertension is the leading modifiable risk factor for cardiovascular diseases and chronic kidney disease globally. In 2015, an estimated 20% of women and 24% of men had hypertension [1], defined as systolic and diastolic blood pressures (BP) of ≥140 mmHg and ≥90 mmHg, respectively. In 2013, one of the voluntary global non-communicable disease targets set by the World Health Assembly was to reduce the prevalence of hypertension by 25% between 2010 and 2025 [2]. Population-based approaches play a fundamental role in this endeavour, with inexpensive BP-lowering therapies being widely available to effectively lower the substantial burden of hypertension among individuals at highest risk. Nevertheless, low awareness, treatment, and control of hypertension across the world foreshadow a substantial preventable disease burden.
With nearly 20% of the world’s population, China represents a large proportion of the global burden of hypertension; 17% of women and 22% of men in China had hypertension in 2015 [1, 3]. The management of hypertension in China is poor [4, 5]; a recent report from a nationally representative survey indicated that ~60% of hypertensive individuals in China are not aware of their condition, about two-thirds are not treated, and less than 10% have proper control [6].
Several studies, from mostly Western populations, have reported that women have greater awareness of their hypertension and higher rates of treatment and control than men [7,8,9,10,11,12,13]. Sex differences in the awareness, treatment, and control of the condition have not been assessed in detail in China. However, these may differ from those in the West because of major cultural and sociodemographic differences, as well as differences in health care delivery and utilization. Accurate information about sex differences in the awareness, treatment, and control of the condition is important, not only to provide a baseline picture from which progress can be monitored, but also to inform the development of better approaches to improve the control of hypertension in both women and men in China.
The aim of this study was to conduct a systematic review with meta-analyses to provide the most comprehensive contemporary estimates of sex differences in the awareness, treatment, and control of hypertension in China.
Methods
Search strategy
We systematically searched four English language (PubMed MEDLINE, EMBASE, Global Health, and Web of Science) and four Chinese-language databases (China National Knowledge Infrastructure, SinoMed, Wanfang, and Weipu) for studies that reported on the awareness, treatment, and control of hypertension separately for women and men in a population-based setting in China. To reflect contemporary health care practice in China, the search was restricted to observational studies conducted after 2005. The search of the English databases was last updated on 1st March 2017. The search of the Chinese databases was last updated on 16th November 2016. The reference lists of all relevant original research and review articles were scanned to capture any potentially missed studies. Four authors, two each for the English and Chinese literature, independently screened the studies and any disagreement was mediated by a third author. The protocol for the systematic review is published in PROSPERO [14].
Study selection
Studies were included if they reported sex-specific awareness, treatment, or control of hypertension in a population-based study in China. Studies were excluded if they included less than 100 individuals or if sex-specific estimates were not provided. In the case of duplicate reports from the same study, the report involving the largest number of participants was included. The quality of the included studies was assessed using a modified version of the Newcastle Ottawa Scale and varied from moderate to good (Supplementary Table 1).
Definitions
The definitions of awareness, treatment, and control of hypertension varied across studies. Most studies defined awareness as a self-report of any prior medical diagnosis of hypertension. Treatment of hypertension was defined as current use of antihypertensive medications. Hypertension was considered as controlled if participants had a systolic BP of <140 mmHg and diastolic BP <90 mmHg.
The terms sex and gender were used interchangeably across studies. Sex refers to the biological and physiological differences between males and females, including differences in hormonal profiles and sex organs, that result from a single chromosomal difference between men (XY) and women (XX). Gender refers to the socially constructed roles, behaviours, activities, and attributes that are considered appropriate for men and women, i.e. the roles that a given society, or individual, considers as masculine and feminine. While differences between women and men in the awareness, treatment, and control of hypertension has both sex and gender elements, we use sex throughout the paper.
Statistical analysis
The primary analysis was a comparison of sex-specific prevalence rates for the awareness, treatment, and control of hypertension. For each study, we calculated the sex difference in prevalence rate by subtracting the rate in men from that in women. Standard errors for the sex-specific prevalence rates, and the women-minus-men differences, were calculated using standard formulae. Prevalence rates and their differences were pooled across studies using random-effects meta-analysis weighted by the inverse of the variances of the prevalence rates. The I² statistic was used to estimate the percentage of variability across studies due to between-study heterogeneity. The presence of publication bias was graphically examined using funnel plots, plotting the women-minus-men differences against its standard error, and tested using Begg’s test. Subgroup analyses were conducted by study region (urban or rural) and by the level of adjustment (crude vs. at least age-adjusted). Data are reported with 95% confidence intervals (CI). All analyses were undertaken with Stata version 12.0.
Results
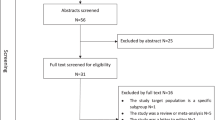
The systematic search identified 10,905 unique records, of which 1401 qualified for full-text evaluation (Fig. 1). Of these, 57 studies reported sex-specific data on the awareness, treatment, and control of hypertension in China for inclusion in further analyses (Supplementary Table 2).
The characteristics of the included studies are summarised in Table 1. Overall, data were available from 2,155,829 individuals (55% women). Twelve studies were conducted in urban areas, 16 in rural areas, and 19 in both urban and rural (i.e. mixed) areas. The median prevalence of hypertension across studies was 32% in women and 37% in men.
Sex differences in the awareness of hypertension
Fifty-one studies including 1,872,289 individuals provided sex-specific data on the awareness of hypertension. The pooled sex-specific prevalence of the awareness of hypertension was 53% (95% CI 49; 58%) in women and 47% (42; 51%) in men (Supplementary Figure 1). The corresponding women-minus men difference in the awareness of hypertension was 7% (6; 8%) and between-study heterogeneity was substantial (I2 = 98%; P < 0.001) (Fig. 2). There was no indication of publication bias (p = 0.83) (Supplementary Figure 2). The sex difference in the awareness of hypertension was 5% (2; 8%) in urban, 7% (4; 9%) in rural, and 7% (5; 8%) in mixed areas and was similar in the crude and adjusted analyses (6% [5; 8%] vs. 7% [5; 9%]).
Pooled women to men difference in the awareness of hypertension. Boxes represent the individual point estimates from each study and the horizontal lines represent the 95% confidence intervals (CI) around the point estimate. The diamond and vertical dashed line represents the pooled summary estimate and 95% CI
Sex differences in the treatment of hypertension
Forty-four studies including 926,276 individuals reported sex-specific treatment rates for hypertension among all those with hypertension. The pooled sex-specific prevalence of the treatment of hypertension was 44% (40; 48%) in women and 38% (34; 42%) in men (Supplementary Figure 3). The women-minus men difference in the treatment of hypertension was 6% (5; 8%) (Fig. 3). Between-study heterogeneity was substantial (I2 = 97%; P < 0.001), but there was limited evidence of publication bias (p = 0.18) (Supplementary Figure 4). The sex difference in the treatment of hypertension was 4% (1; 7%) in urban, 6% (4; 8%) in rural, and 7% (5; 9%) in mixed areas and was somewhat smaller in the crude than in the adjusted analyses (6% [4; 7%] vs. 9% [6; 12%]). Twelve studies comprising 805,053 individuals reported on the treatment of hypertension among those who are aware of their condition. Among those aware, the pooled sex-specific prevalence of treatment of hypertension was 65% (50; 81%) in women and 60% (47; 72%) in men (Supplementary Figure 5). The corresponding women-minus men difference in the treatment of hypertension was 6% (2; 9%) (Supplementary Figure 6). Differences between regions were limited; the women-minus men difference was 9% (1; 16%) in urban, 8% (2; 13%) in rural, and 5% (0; 10%) in mixed areas. The findings were consistent in the crude and adjusted analyses (5% [1; 9%] vs. 6% [3; 11%]).
Pooled women to men difference in the treatment of hypertension among all those with hypertension. Boxes represent the individual point estimates from each study and the horizontal lines represent the 95% confidence intervals (CI) around the point estimate. The diamond and vertical dashed line represents the pooled summary estimate and 95% CI
Sex differences in the control of hypertension
Forty-two studies including 2,022,836 individuals provided sex-specific data on the control of hypertension among all those with the condition. The pooled sex-specific prevalence of the control of hypertension was 17% (14; 20%) in women and 14% (11; 16%) in men (Supplementary Figure 7). The corresponding women-minus men difference in the control of hypertension was 3% (2; 3%), with substantial heterogeneity between studies (I2 = 98%; P < 0.001) (Fig. 4). There was limited evidence of publication bias (p = 0.15) (Supplementary Figure 8). The sex difference in the control of hypertension was 5% (2; 9) in urban, 0% (−0.5; 0.6) in rural, and 2% (1; 3%) in mixed areas, with minimal differences between the crude and adjusted findings (3% [2; 4%] vs. 2% [1; 3%]). Twenty-four studies including 738,057 individuals reported on the control of hypertension among those who are treated for hypertension. Among those treated, the pooled sex-specific prevalence of the control of hypertension was 27% (22; 32%) in women and 27% (22; 32%) in men (Supplementary Figure 9). The corresponding women-minus men difference was −0.2% (−1.5; 1.0%) (Supplementary Figure 10), which did not differ substantially by study region; the difference was −0.4% (−4; 3%) in urban, −2% (−5; 0%) in rural, and 0.3% (−1.5; 2.2%) in mixed areas. The women-minus men difference was −0.6% (−1; 3%) in the crude analyses and −2% (−3; −1%) in the adjusted analyses.
Pooled women to men difference in the control of hypertension among all those with hypertension. Boxes represent the individual point estimates from each study and the horizontal lines represent the 95% confidence intervals (CI) around the point estimate. The diamond and vertical dashed line represents the pooled summary estimate and 95% CI
Discussion
This systematic review with meta-analyses, which included over 2 million individuals in China, demonstrates that the awareness, treatment, and control of hypertension differs between women and men in this large country. While the awareness, treatment, and control of hypertension among all those with hypertension is low in both sexes, women consistently had greater awareness and treatment of their hypertension than men. Overall, the control of hypertension was also better in women than men, but there were no sex differences in the control of hypertension among those receiving antihypertensive medications.
The sex differences in the awareness, treatment, and control of hypertension reported here are broadly consistent with findings from various countries. A report from the US National Health and Nutrition Examination Survey (NHANES) demonstrated that the awareness and treatment of hypertension were higher in women than in men [7]. While the control of hypertension had improved between 1988–1994 and 2007–2008 in both women and men, the sex differences did not change. In Germany, sex differences in the management and control of hypertension persisted between 1998 and 2008–2011, with younger men being considerably more likely than younger women to be unaware, untreated, and uncontrolled [11]. Additionally, the Prospective Urban Rural Epidemiology (PURE) Study among 140,000 adults across 17 different countries demonstrated that women had greater awareness of their hypertension and higher rates of treatment and control than men, irrespective of the economic status of the country [9]. In addition, the PURE study, in agreement with the present analyses, reported substantial differences across study regions, with considerably lower rates of awareness, treatment, and control of hypertension among rural areas compared to urban areas. This present study expands on these findings by showing that the sex differences in awareness and treatment of hypertension are consistent between urban and rural settings. However, sex differences in the control of hypertension were only observed in urban communities, suggesting that strategies to optimise the awareness, treatment, and control of hypertension need to be tailored to the needs of men and women in specific settings.
Factors underpinning these sex differences in the awareness, treatment, and control of hypertension are uncertain, but they may be age-related. A number of studies have shown that the awareness and treatment of hypertension are generally higher among older than among younger individuals, with conflicting evidence on age differences in the control of hypertension [7, 9]. However, few studies have characterised the influence of age on sex differences in the awareness, treatment, and control of hypertension [11,12,13, 15, 16]. NHANES 1999–2004 demonstrated that, in middle-age, antihypertensive medication use was significantly higher among women than among men [15]. However, among the elderly, women were treated less aggressively and had worse hypertension control than men. Further analyses of NHANES 2013-4 showed that the sex differences in the awareness, treatment, and control of hypertension were restricted to young adults, with a considerable awareness and treatment gap in those younger than 40 years of age [12]. Results from the CardioVascular Research Network (CVRN) among 150,000 individuals in the US with hypertension demonstrated that younger women, but older men, had higher rates of hypertension awareness, treatment, and control compared to their similarly aged counterparts [16]. Findings from the China Kadoorie Biobank, which were included in the present study, also indicated that women’s advantage in the awareness, treatment, and control of hypertension deteriorated with age [17]. Reasons for these opposing sex differences across the age spectrum are uncertain. At younger ages, women’s greater awareness, treatment and control may be related to the fact that women who are pregnant are more likely to be detected and treated for hypertension, as their blood pressure is routinely monitored throughout pregnancy.
Differences between women and men in health-seeking behaviour, especially among younger adults, might also contribute to the more favourable rates of awareness, treatment, and control of hypertension in women reported here [18]. A study among 15,000 young adults in the US found that sex differences in the awareness of hypertension could be ascribed to disparities in health care use with more regular visits among women than men [10]. Similarly, NHANES 2013-4 found that more health care visits among young adult women accounted for 30% of the sex-related differences in awareness, 60% of the difference in treatment, and 52% of the difference in control [12]. Thus, little contact with the health care system in men, compared with women, may explain their lower awareness, treatment and control of hypertension.
While the control of hypertension among all those with hypertension was higher in women than men, the absence of sex differences in the control of hypertension among those treated for the condition is perhaps not surprising given evidence from randomised controlled trials which has demonstrated that the effects of blood pressure lowering medications are similar in women and men [19]. Hence, the sex difference in control rates among all those with hypertension is more likely to be explained by sex differences in awareness and treatment of hypertension than by sex differences in the effectiveness of medications.
The strengths of this meta-analysis are its size and inclusion of studies published in both the Chinese and English literature, which enabled us to conduct the most comprehensive analyses to date on sex differences in the awareness, treatment, and control of hypertension in China. However, there are some limitations of this study that are inherent in the use of published data, including the heterogeneity between studies in the ascertainment of hypertension, study design and sampling methods, endpoint definitions, and the degree of adjustment for confounders. While rates of awareness, treatment, and control of hypertension differ by age, some included studies only provided crude results. Sensitivity analyses excluding those studies did not alter the findings. Moreover, since we compared women and men within the same study, any influence of methodological differences between studies is likely to have affected women and men similarly. We therefore assume that this report of sex comparisons remains valid. Further, the nature of our study did not allow us to identify factors explaining the reported sex differences in the awareness, treatment, and control of hypertension in China.
The present study, once again, strengthens the need to address the low levels of awareness, treatment and control of hypertension in China. A [4] recent report from the China PEACE Million Persons Project among 1.7 million Chinese adults aged 35–75 showed that less than a third of those with hypertension were treated. The control of hypertension was ubiquitously low among all of the many subpopulations throughout China, with fewer than one in twelve in control of their blood pressure. As in this study, women had higher awareness, treatment, and control rates than men. The PEACE project also showed that there are major deficiencies in the availability, cost, and prescription of antihypertensive medications across China [5], despite China’s National Essential Medicine Program which mandates the availability and zero-profit prescription of essential medications in public primary health care settings [20]. National integrated efforts, involving multiple stakeholders, will be needed to improve the prevention and control of hypertension in China.
In conclusion, while the awareness, treatment, and control of hypertension in China is low in both sexes, women had greater awareness, treatment and control of their hypertension than men. These findings heighten the need for sex-specific interventions, especially strategies targeted at increasing awareness, treatment and control for men, to combat the economic and health burden of hypertension efficiently and effectively for both men and women.
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37–55.
World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013-20. Geneva, Switzerland: World Health Organization; 2013.
NCD Risk Factor Collaboration. 2017. http://www.ncdrisc.org/index.html (accessed 10-11-2017)
Lu J, Lu Y, Wang X, Li X, Linderman G and Wu C. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017;390:2549–58.
Su M, Zhang Q, Bai X, Wu C, Li Y and Mossialos E. Availability, cost, and prescription patterns of antihypertensive medications in primary health care in China: a nationwide cross-sectional survey. Lancet. 2017;390:2559–68.
Li Y, Yang L, Wang L, Zhang M, Huang Z, Deng Q, et al. Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int J Cardiol. 2017;227:516–23.
Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–50.
Gee ME, Campbell NR, Gwadry-Sridhar F, Nolan RP, Kaczorowski J, Bienek A, et al. Antihypertensive medication use, adherence, stops, and starts in Canadians with hypertension. Can J Cardiol. 2012;28:383–9.
Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–68.
Everett B, Zajacova A. Gender differences in hypertension and hypertension awareness among young adults. Biodemography Social Biol. 2015;61:1–17.
Sarganas G, Neuhauser HK. The persisting gender gap in hypertension management and control in Germany: 1998 and 2008-11. Hypertens Res: Off J Jpn Soc Hypertens. 2016;39:457–66.
Zhang Y and Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. 2017;70:736-42.
Choi HM, Kim HC, Kang DR. Sex differences in hypertension prevalence and control: Analysis of the 2010-4 Korea National Health and Nutrition Examination Survey. PLoS ONE. 2017;12:e0178334.
Redfern A, Luo R, Cheng Y, Li Q, Wang H. A systematic review of access to care and quality of care for women with non-communicable diseases in China. PROSPERO 2016:CRD42016050415 2016. https://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016050415 (accessed 10-11-2017)
Gu Q, Burt VL, Paulose-Ram R, Dillon CF. Gender differences in hypertension treatment, drug utilization patterns, and blood pressure control among US adults with hypertension: data from the National Health and Nutrition Examination Survey 1999-2004. Am J Hypertens. 2008;21:789–98.
Daugherty SL, Masoudi FA, Ellis JL, Ho PM, Schmittdiel JA, Tavel HM, et al. Age-dependent gender differences in hypertension management. J Hypertens. 2011;29:1005–11.
Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176:524–32.
Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. J Fam Pract. 2000;49:147–52.
Turnbull F, Woodward M, Neal B, Barzi F, Ninomiya T, Chalmers J, et al. Do men and women respond differently to blood pressure-lowering treatment? Results of prospectively designed overviews of randomized trials. Eur Heart J. 2008;29:2669–80.
Song Y, Bian Y, Petzold M, Li L, Yin A. The impact of China’s national essential medicine system on improving rational drug use in primary health care facilities: an empirical study in four provinces. BMC Health Serv Res. 2014;14:507.
Funding
This work was supported by a policy grant from the Oxford Martin School at the University of Oxford. SP is supported by a UK Medical Research Council Skills Development Fellowship (MR/P014550/1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Redfern, A., Peters, S.A.E., Luo, R. et al. Sex differences in the awareness, treatment, and control of hypertension in China: a systematic review with meta-analyses. Hypertens Res 42, 273–283 (2019). https://doi.org/10.1038/s41440-018-0154-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0154-x
Keywords
This article is cited by
-
A tryst of ‘blood pressure control- sex- comorbidities’: the odyssey of basic public health services in Yunnan in quest for truth
BMC Public Health (2024)
-
Management of Hypertension in the Asia-Pacific Region: A Structured Review
American Journal of Cardiovascular Drugs (2024)
-
Prevalence and the age of onset patterns of stroke in Jiangsu Province, China
Neurological Sciences (2023)
-
The Burden of Resistant Hypertension Across the World
Current Hypertension Reports (2022)
-
Measuring Knowledge, Attitudes, and Barriers to Medication Adherence in Potential Bariatric Surgery Patients
Obesity Surgery (2021)