Abstract
Purpose
The COVID-19 pandemic has forced reorganization of clinical services to minimize face-to-face contact between patients and health-care providers. Specialist services, including clinical genetics, must consider methods of remote delivery including videoconferencing—termed telegenetics. This review evaluates the evidence for telegenetics and its applicability to future service development.
Methods
A systematic review of six databases was conducted to identify studies from 2005 onward using synchronous videoconferencing to deliver clinical genetics services. Included studies compared telegenetics to an alternative method or used a before and after design.
Results
Thirteen studies met the inclusion criteria (eight compared telegenetics to in-person consultations and three to telephone delivery). Patient satisfaction, genetic knowledge, and psychosocial outcomes were similar for in-person and telegenetic counseling. There was some evidence that telegenetics may be superior to telephone delivery for knowledge gain and reduction in anxiety and depression. There is limited evidence concerning the effect of telegenetics on provider satisfaction and behavioral outcomes. Conclusions are limited by at least moderate risk of bias in all evaluated studies and small sample sizes.
Conclusion
Across most outcomes measured, telegenetics had equivalent outcomes to in-person appointment; however, the extent to which the available evidence is applicable to longer-term use is debatable.
Similar content being viewed by others
INTRODUCTION
Technological advances are causing major changes in all aspects of medical practice, from diagnosis to management. The implementation of technology to remotely communicate with patients is one example. Telemedicine can be broadly defined as “[...] The delivery of health care services, where distance is a critical factor, […] using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease […].” 1 Within clinical genetics services, four modes of telemedicine have been identified globally.2 The most commonly used is live synchronous videoconferencing—commonly referred to as telegenetics.3,4,5,6 Although some reports use the term "telegenetics" to cover both telephone and video communication,6 for the purpose of this review we will use “telegenetics” to refer to live synchronous videoconferencing between the provider and the patient or family.
Some aspects of genetics services, in particular genetic counseling, are theoretically well-suited to remote delivery via videoconferencing, as the clinical interaction consists largely of communication rather than physical examination. Videoconferencing software can also allow use of the supportive tools used for in-person counseling such as disease information brochures. Previous reviews of the use of telegenetics have concluded that across a range of genetics services, subspecialities, and countries, patient satisfaction with telegenetics is generally high, and affective outcomes are comparable to in-person services.2,4,7 Despite this, the uptake of telegenetics has been varied, with cross-sectional surveys reporting prevalence (for delivery of genetic counseling) between 9% in Europe8 and 33% in the United States.9
The COVID-19 pandemic has forced a sudden and rapid increase in telemedicine usage to deliver clinical services. There is a new imperative to minimize face-to-face contact between patients and clinical staff to reduce the risk of transmission of the virus to patients or staff10,11,12 including in the field of clinical genetics.13,14 The extent to which this rapid expansion of telemedicine will remain a component of standard practice postpandemic is not clear. There is evidence of a desire among policy makers for this to continue, and the reality may be a blended form of in-person and remote working. In a speech on 30 July 2020, the UK Secretary of State for Health stated, “So from now on, all consultations should be teleconsultations unless there’s a compelling clinical reason not to.”15 Governments have invested in telemedicine infrastructure that will facilitate ongoing changes to service delivery.11 Providers are also increasingly exploring telemedicine. In a survey of genetic counselors conducted by Ritchie and colleagues9 50% of those who did not yet use telehealth said they were looking to adopt this as a method for future consultations.
Whether telemedicine becomes part of the new standard method of practicing, or future waves of this or other pandemics necessitate further restrictions on face-to-face contact, it is necessary to have a clear understanding of the potential benefits and pitfalls of telegenetics. There has been no systematic review of telegenetics since 2012,4 and it did not evaluate the quality of the available evidence and suggested that further prospective, adequately powered studies were needed.
Our systematic review aims to provide an up-to-date synthesis of whether the evidence supports substituting videoconferencing for face-to-face delivery of clinical genetics services. We aim to both identify gaps in the current literature and inform future service design and research. We have focused on videoconferencing, as while telephone consultations are relatively well established in delivery of genetics services, videoconferencing is generally a novel mode of service delivery. In addition, videoconferencing offers the opportunity to maintain nonverbal communication and elements of visual examination while avoiding in-person contact, making it particularly relevant to the current COVID-19 pandemic situation.
MATERIALS AND METHODS
Data sources and search strategy
This systematic review was conducted in accordance with a predefined protocol and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [PRISMA CHECKLIST in Supplementary material]. Six databases (Medline; Web of Science; Cochrane; EMBASE; PsychInfo, and the British Nursing index) were searched on 31 May 2020. The search was repeated on 3 October 2020. Search terms were grouped into two categories: those relating to genetics services, and those relating to telemedicine or videoconferencing. Details of the search terms can be found at in Table 1. References were imported into Mendeley (www.mendeley.com) and duplicates removed. Titles and abstracts were screened, and full texts were obtained when more information was needed to make a decision about inclusion. Reference lists of all studies that proceeded to full-text screening and relevant reviews were hand searched for additional publications.
Study selection and eligibility
All full-text studies were independently reviewed by three reviewers (E.L.B., E.R.B., and A.M.) to determine if they met the inclusion criteria. Any disagreements were resolved by discussion with a fourth reviewer (I.W.). Studies were eligible for inclusion if they were published in a peer-reviewed journal in English and evaluated the use of real-time videoconferencing to deliver consultations in any area of clinical genetics. Randomized controlled trials (RCTs) and nonrandomized studies that compared videoconferencing to an alternative delivery method or utilized a before and after design were included if they evaluated one of the outcomes of interest. Reviews, letters with no primary data, and cross-sectional surveys were excluded.
The outcomes of interest were patient and/or caregiver satisfaction; provider satisfaction, patient knowledge and perceived risk; psychosocial outcomes including anxiety, depression, and perceived personal control; clinical efficacy (e.g., arriving at the correct diagnosis); behavioral outcomes (i.e., uptake of screening, testing, or treatment); and cost-effectiveness.
To ensure information gathered was relevant, particularly given the rapid rate of advance in technology, articles published before 2005 and conference abstracts published before 2015 were excluded. Studies reporting only qualitative data were not included in the main review or formally synthesized, but were noted, and key conclusions highlighted in “Discussion.”
Data extraction
Two authors (E.L.B. and I.W.) independently extracted data from each of the studies included in the review into a predesigned data abstraction form. Disagreements were resolved by discussion with a third reviewer (I.R.).
Assessment of study quality
Peer-reviewed journal articles that evaluated genetic counseling were assessed for risk of bias (eight studies). Published conference abstracts could not be assessed due to insufficient information being provided. The Cochrane Collaboration RoB 2 tool16 was used to assess RCTs. For nonrandomized studies, the Newcastle–Ottawa Scale (NOS) was used.17 On the NOS, studies that scored nine stars were judged to indicate a low risk of bias, those that scored seven or eight stars were considered medium risk, and those scoring six or less were high risk. All studies were independently assessed by two reviewers (E.L.B. and I.W.) and disagreements were resolved by discussion with a third reviewer (I.R.).
Analysis
Descriptive summary tables were constructed to display the results. Due to the small number and heterogeneity of studies meeting the inclusion criteria, it was not possible to conduct a meta-analysis.
RESULTS
Study characteristics and telegenetics setup
A total of 13 studies met the inclusion criteria—11 articles in peer-reviewed journals (2 RCTs, 8 nonrandomized studies and 1 within-subject comparison) and two conference abstracts reporting interim results of RCTs. Eight studies compared video consultations to in-person consultations, and three compared telegenetics with telephone delivery.18,19,20 Included studies were published between 2005 and 2019 and were conducted in Australia, England, the Netherlands and the United States. Full details of the studies included, their methods, and results can be found in Table 2.
Twelve of 13 studies meeting the inclusion criteria involved the delivery of genetic counseling; the majority (n = 10) focused on cancer genetic counseling for individuals with family histories of hereditary cancers (most commonly hereditary breast and ovarian cancer). Others involved patients receiving prenatal genetic counseling,21,22 and counseling regarding genetic risk for Alzheimer disease19 and familial cardiogenetic variant.22 In almost all studies the patient attended an outreach clinic and communicated with the genetics professional via video link. Only two studies22,23 reported on the delivery of counseling via videoconferencing to patients in their homes, which has now become the more typical method due to the circumstances of the COVID-19 pandemic.
The health-care professionals delivering genetic counseling varied. Most studies utilized genetics counselors (n = 10); however, some included clinical geneticists or oncologists with training in delivering genetic counseling (n = 5) alone or as an adjunct to a counselor. In some instances multiple counselors were present, with one at the satellite clinic and the clinical geneticist at the end of the video link.24
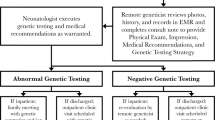
Only one study involving the delivery of services other than counseling met the inclusion criteria.25 In this small pilot study the authors assessed the accuracy of clinical examination via video link of ten patients in the neonatal intensive care unit referred to the genetics service for dysmorphic features. Patients were first examined by a bedside clinician directed by a genetics consultant who viewed the examination via live video, this was later compared to an in-person examination by the same clinical geneticist for accuracy.
Patient and provider satisfaction
Studies evaluating patient satisfaction with genetic counseling via telegenetics (n = 10) reported a high level of satisfaction with all types of counseling. Four studies controlled for participant characteristics to examine whether specific factors were associated with satisfaction. Buchanan and colleagues26 found no significant difference in satisfaction between the telegenetics and the in-person groups when controlling for age, marital status, computer anxiety, Internet use, education status, and genetic testing uptake. Conversely, Bradbury and colleagues18 found that higher education status was associated with a lower satisfaction with the telemedicine service (p = 0.02).
In studies that compared telephone and telegenetics there were also no differences in satisfaction postcounseling between methods. In the study by Voils and colleagues average satisfaction point scores were 25.2/30 for telephone and 26.9/30 for video.20 In open-ended questions, the telephone group enjoyed the convenience of the experience, while the video group liked being able to see counselor body language. In a three-armed trial18 satisfaction was slightly higher in the telephone arm after results disclosure but this was not statistically significant (p = 0.07)
One study evaluated provider satisfaction with telemedicine.23 Ten genetic counselors were assessed at baseline, after each counseling session and at the end of the study period. Overall, there was a decrease in provider satisfaction over the study period. However, conclusions are limited by the small sample size.
Psychosocial outcomes following genetic counseling
Seven studies also examined the psychological outcomes after counseling and how these were affected by delivery methods. Different tools were used across the included studies. In all seven studies there was a decrease in anxiety and depression after genetic counseling regardless of the counseling delivery method. Abrams and colleagues report a decrease in anxiety and depression postcounseling, with no significant difference between in-person and videoconferencing groups (p = 0.42 and p = 0.96 respectively).21 Solomons et al.27 used the PHQ-4 questionnaire and showed a nonsignificant trend toward reduction in depression postcounseling for the remote group (p = 0.2) and in-person group (p = 0.16). Again, there was no significant difference between groups. In the Bradbury et al.18 study comparing telephone and video there was also no statistically significant difference in the reduction in depression between groups (p = 0.07).
Four studies looked at cancer specific anxiety rather than overall anxiety and depression. Zillacus et al.24 used an Impact of Events Scale, with no difference between groups (p = 0.13). Similarly, the analysis of Otten et al.22 used the State Trait Anxiety Inventory28 and indicated that the mean change in disease specific anxiety did not differ between groups pre- and postcounseling.
Otten and colleagues22 also assessed patients’ perceived personal control (PPC). Both the in-person and telegenetics group had a statistically significant increase in PPC after counseling; however, there was no significance for between-group differences. The work by Zillacus et al.24 also examined PPC with the same questionnaire and reported an increase in PPC in both groups, with a significantly greater increase in the telegenetics group (p = 0.031).
Change in participant knowledge after genetic counseling
Six studies assessed participant genetic knowledge before and after genetic counseling, examining how well individuals could understand and retain information across different delivery platforms. Of these, three24,27,29 assessed increase in knowledge of cancer genetics for counseling delivered in-person compared to telegenetics. None reported superiority of either method. Zillacus and colleagues assessed knowledge of breast cancer genetics with a 12-item scale that had been adapted from previous research.30 Knowledge of hereditary breast and ovarian cancer was high at baseline and follow up, with a significant increase in knowledge in both groups and no statistically significant difference in knowledge gain between groups (p = 0.55). This study excluded those with low literacy levels, potentially limiting the generalizability of their results. The study by Solomons et al. also examined breast and ovarian cancer genetic knowledge pre- and postcounseling, as well as 1 month after counseling.27 This too indicated an increase in knowledge in both groups with no statistically significant difference between groups. Importantly knowledge gain was maintained at 1 month follow up.
An additional two studies compared knowledge gain for patients receiving counseling via telegenetics to telephone counseling. An RCT comparing telephone and video-based counseling20 showed a slight trend toward increased colorectal cancer knowledge gain in the video group, but there was no statistically significant difference between groups. However, in a published conference abstract reporting an interim analysis of an RCT of cancer genetic counseling18 there was statistically significant increase in knowledge gain in the video arm over the telephone arm (17.8 vs. 7.4, p <0.01).
It is important to note that these studies all focused on knowledge about cancer genetics, and mainly on hereditary breast and ovarian cancer. No studies assessed knowledge about prenatal genetic risk or pediatric genetic conditions. One conference abstract19 reports an ongoing RCT comparing telephone to video disclosure of APOE genotype to patients in the Alzheimer’s Initiative Generation Study, with knowledge as one of the prespecified outcomes. Although results relating to knowledge were not reported at this stage, the full results may contain important insights.
Cost of telegenetic counseling
Only three studies formally examined the cost of different counseling platforms; of these, two were performed in the United States and one in the Netherlands. Buchanan and colleagues26 randomized patients to videoconferencing or in-person appointments. Considering the cost of setting up and maintaining the telegenetics system, as well as the labor time to log patients into the system they calculated that telegenetics cost $106.19 per patient. The in-person group was calculated to be $244.33 when accounting for the travel time cost and time spent on counseling (their data did not account for time taken for the patient to travel to the outreach clinic for telegenetics). Voils and colleagues20 compared the cost of telegenetics to telephone delivery. Videoconferencing compared to telephone required a median 2.8-hour total journey time and the estimated mean loss of productivity was $67.29. However, this did not consider the cost of setting up the telegenetics platform. Otten and colleagues23 calculated both the time and monetary cost differences between telegenetics and in-person counseling. They estimated the time saving associated with telegenetics was 7.6% for cardiogenetic and oncogenetic counseling and 8.8% for prenatal, with related cost savings of 10.2% (€361 to €324, equivalent to $444 to $389) for cardiogenetic and 12.4% (€379 to €332, equivalent to $456 to $399) for prenatal services.22 No studies evaluated cost-effectiveness, i.e., cost per beneficial outcome.
Suitability of telegenetics for clinical diagnosis
Only one study assessed the accuracy of using telegenetics for clinical diagnosis or for delivering consultations where physical examination is required. Wenger and colleagues31 compared remote and in-person examinations of patients in neonatal intensive care referred for evaluation of dysmorphic features. Initially, a remote assessment was carried out by a consultant geneticist viewing a live video link and giving instructions to a bedside clinician (also a geneticist). The remote consultant then repeated the examination in person, and agreement between remote and in-person assessments was assessed. Remote examinations identified 81/87 features (97%) and when conditions were optimized (changing lighting and positioning) 83/87 (95%) were identified. The features not identified included cleft palate, clinodactyly, and scars. While findings were similar between remote and in-person groups both examinations were performed by a geneticist, and results may not be applicable to a scenario where other health-care professions with less experience in this style of examination act as the “bedside clinician.”
Uptake of screening, testing, or treatment
Only two studies meeting the inclusion criteria reported uptake of screening, testing, or treatment following telegenetics. Otten and colleagues22 examined whether the method of delivery of counseling affected the uptake of DNA testing. In the online group, test uptake was 95% versus 93% for in-person counseling (p = 0.73). Health-care use after completion of counseling was rare in both groups, with no significant difference (p = 0.99). Bradbury and colleagues18 report increased uptake of pretest genetic counseling (79% vs. 5%, p < 0.001) and genetic testing (56% vs. 12.5%, p < 0.001) for patients at community practices without access to genetic providers randomized to remotely delivered genetic services versus usual care. However both telephone and videoconferencing are included in the remotely delivered arm, and this preliminary report does not give breakdowns by delivery method.
Buchanan and colleagues26 noted that patients assigned in-person counseling were significantly more likely to attend appointments than those in the telegenetics group (89% vs. 79%, p = 0.03). In both groups nonattendance was associated with not being married, unemployment, lower salary, and lower education status. In an interim 6-month analysis of a three-armed RCT published as a conference abstract, Bradbury and colleagues18 noted that 79% of participants in the remote service arm versus 5% in the usual care arm had completed genetic counseling (p < 0.001). A similar pattern was noted for uptake of genetic testing with 56% of those in the remote arm and 12.5% in the usual care arm having genetic testing (p < 0.01). Of note, in this study the usual care arm did not automatically consist of an in-person consultation but involved information leaflets and advice on how to seek counseling. However, this provides a different perspective, examining telegenetics as a standalone service rather than as an alternative to an in-person consultation.
Study limitations and bias
Non-RCTs were assessed for bias using the NOS and RCTs were assessed using the Cochrane Rob 2 tool. The two abstracts were unable to be assessed, and three additional studies23,31,32 were not assessed as the study designs did not involve a comparison or control group. Full bias assessment results can be found in Tables 3 and 4.
Of the seven nonrandomized studies analyzed via the NOS the range of star scores was 3–6. No studies had low risk of bias. The main reason studies scored poorly were failures to control for patient characteristics, outcomes being assessed via self-report, and loss to follow up. Both RCTs examined using the Cochrane bias tool were found to have some risk of bias. Common sources of bias were missing outcome data and the fact that patients could not be blinded to their allocated group. Limitations common to multiple studies were small sample sizes precluding statistical testing of between-group differences.20,21,33 Other issues include not gathering a representative population, i.e., by excluding those with poorer literacy.24 Another common problem was high loss of participants to follow up. For example, in the Mette et al. study there was only a 34% completion rate for questionnaires.33
DISCUSSION
The majority of the literature comparing genetics services delivered by videoconferencing to alternative delivery methods is in the field of genetic counseling, in particular pre- and post-test counseling for those with family history of cancer. Pandemics such as coronavirus are highlighting a need to diversify medical service delivery platforms to provide additional methods to the typical face-to-face approach. However, regular reviews are required to ensure that this is a safe and effective method that is acceptable to patients. This review provides information to aid in answering this question.
Overall conclusions
Our review aimed to provide an up-to-date synthesis of the evidence for substituting videoconferencing for face-to-face delivery of clinical genetics services. We explored this question by evaluating a range of relevant outcomes of genetic services including patient satisfaction, psychosocial outcomes, knowledge gained, and impact on subsequent uptake of services.
Overall, patients receiving genetic counseling by telegenetics had immediate outcomes that were at least equivalent to those receiving counseling face to face—in terms of satisfaction, knowledge gained, and psychosocial outcomes. There is very limited evidence available concerning the effect of telegenetics on provider satisfaction, behavioral outcomes (e.g., uptake of screening, testing and treatment), and the utility of telegenetics for services requiring physical examination.
Reported patient satisfaction with telegenetics was high across a range of subspecialities and patient groups. There were no reported statistically significant differences in knowledge gain postcounseling, although it should be noted that only knowledge of cancer genetic risk was assessed, and mainly breast and ovarian cancer.24,27,29 Few studies assessed long-term knowledge gains, but Solomons and colleagues reported a maintained increase in knowledge at one month. Genetic counseling generally reduced levels of anxiety and depression, again with no statistically significant differences between delivery methods.
Comparing telephone and video consultations, all studies reported high satisfaction in both groups. There is some evidence that videoconferencing is superior to telephone genetic counseling in terms of improving knowledge of cancer genetic risk18,20 and anxiety and depression scores.18 This reduction in depression was only noted in one study, and was not statistically significant; however, this is a key patient outcome and the benefit of video software to allow nonverbal communication could be essential when dealing with sensitive subjects.
Limitations of the available evidence
There are limitations in the quality of the evidence gathered. All six nonrandomized studies comparing genetic counseling via videoconferencing to face-to-face delivery were judged to be high risk of bias, and both published randomized controlled trials were at some risk of bias. Common issues were failure to control for difference in baseline patient characteristics, and high loss to follow up.
A number of studies (four) introduced bias by assigning patients to intervention group by geographical location (patients in more remote areas were assigned to the telegenetics group). While this method was pragmatic, and utilized one of the positive impacts of telegenetics (reduced need for travel and associated costs), these groups may have different characteristics. For example, in the paper by Solomons et al. the groups were divided geographically, and the remote group was older, less likely to have a college education, and more likely to live rurally.27 These areas are also frequently underserved, and those who are receiving a service that they ordinarily would not have may feel obligated to endorse it.4
The evidence on patient satisfaction should also be interpreted with caution. First, patient satisfaction was collected through self-reporting and all individuals had agreed to be involved in a trial where a service was provided by videoconferencing. Previous research has indicated that allowing patients a choice of how to receive genetic test results gives higher satisfaction than not allowing a choice.34 This is highlighted in the Otten et al. study where only 35% of those approached chose to have online counseling, but those who did proceed with this counseling had high satisfaction.22 Another methodology issue is the potential for a ceiling effect in the data. Satisfaction was generally high across all three counseling delivery methods (telephone, videoconferencing, and face to face), and there is a risk that high scores are masking intergroup differences. Several studies were limited by small sample sizes precluding statistical analysis of between-group differences.20,21,33
Relevance to service delivery during the worldwide COVID-19 pandemic
One purpose of this review was to assess the evidence in support of providing genetics services via videoconferencing in the context of a worldwide COVID-19 pandemic. Overall the evidence produced in this review supports the use of videoconferencing as a feasible method of delivering genetic counseling that is acceptable to patients. The COVID-19 pandemic has dramatically altered the way that both the health service and other industries view service delivery. There is a general move toward increasing digital use and remote working and in a health-care context this may help to improve efficiency of the service and reduce patient requirements for time off work and managing other commitments such as child care. However, the modes of telegenetic service delivery that have been most widely studied may not be relevant to the current situation.
First, most of these studies involved the patient attending outreach clinic—i.e., still coming into contact with health-care professionals. Only two studies,22,23 used videoconferencing software in the home. No studies assessed clinical examination solely via telemedicine—in the example by Wegner and colleagues, a bedside clinician followed directions from a remote clinician to facilitate the assessment.31 This is less relevant to a situation where the aim of telegenetics is to avoid patient exposure to a health-care setting. Second, these studies are mostly evaluating telegenetics as an adjunct to existing services—expanding the reach of genetic services in underserved populations, rather than replacing the existing framework. Evidence for noninferiority of remote delivery of services in patient groups opting for telegenetics does not guarantee that an equivalent service can be provided remotely for all patients. It is not clear whether results of this evaluation would be altered if telemedicine was the sole option.
Finally, telegenetics is not an option for everyone. In Otten and colleagues’ evaluation of telegenetics delivered to patients in their homes22 65% of patients had to be excluded due to a lack of equipment. A 2020 paper by Lam and colleagues looked at telemedicine unreadiness in the United States. Looking at a database of 4,525 adults over the age of 65 they found 38% were not ready for telehealth (which equates to 13 million people in the United States). This was primarily due to inexperience with technology but other factors included physical disabilities such as problems with hearing.35 In contrast, some recent research has indicated that telemedicine can increase attendance at appointments. A study by Jeganathan and colleagues36 looked at a telemedicine service for obstetric patients rapidly set up during the COVID-19 pandemic. Comparing data from 1 March to 30 May in 2019 and 2020 they showed a significant reduction in “no shows” with the introduction of telemedicine. When implementing new service delivery methods we need to ensure it is equitable for all, including those with a disability of disadvantage such as digital poverty. If not implemented carefully and in parallel with other modes of service delivery this has the potential to widen health inequalities. The COVID-19 pandemic has already widened a number of inequalities in health, education, and income and further research is needed to examine how the move to telegenetics could affect the reach of service provision and ensure that it is introduced fairly and effectively.
Gaps in the literature and need for further research
There remain significant gaps in the literature that require further study—in particular, telegenetics in pediatrics, how increasing the proportion of services delivered via telegenetics affects patient access, and longer-term clinical and behavioral outcomes.
Only one study involving ten patients31 evaluated telegenetics for pediatric patients and for clinical examination. One similar small feasibility study was identified that did not meet inclusion criteria.37 Ten children referred to genetics services for evaluation of developmental delay were assessed in an outreach clinic, with an experienced genetic counselor taking physical measurements and images directed by a geneticist on a video link. The authors conclude that measures differed slightly but not sufficiently to affect the assessment and alter diagnosis, but one referring pediatrician later raised concerns that clinical features had been missed. Overall there is not sufficient evidence to comment on the feasibility of using telegenetics to conduct pediatric consultations, due to a lack of literature in this area. This group also provides unique challenges as children may respond differently to telegenetics than adults. Hopper and colleagues note that some of the children had to be coaxed to participate and the large camera used may have been too intrusive.37 Other challenges include consent and data governance, particularly if the video link may require images of intimate areas. These studies also raise the issue of telegenetic use in consultations that may require some form of physical examination in addition to counseling. Work by Bidmead et al.10 used a local sonographer sending images to a distant fetal medicine consultant. While individuals were accepting of this service the sonographers commented on the pressure they felt to provide emotional support, something they would not routinely have to do. This highlights unexplored issues with remote consultations, and the difficulties faced by the bedside clinician.
Strengths and limitations of our study
Our review builds on previous work4 to provide an up-to-date overview of the evidence for providing genetics services via videoconferencing. Regular reviews in the field of telehealth are required due to rapid advances in the capability of technology, and the COVID-19 pandemic has greatly increased the importance and focus on telehealth services. This review was performed in accordance with the PRISMA reporting guidelines, and all data was checked by at least two individuals. Due to the heterogeneity of the studies identified, we were not able to synthesize results by meta-analysis. One strength of our review is the inclusion of studies from multiple countries, across multiple types of genetics services. However, the generalizability of results will be limited by differences in health service delivery context between regions, and by the different patient populations accessing different types of services. Our hope is that by highlighting the areas of strength and weakness in the literature, as well as the range of service delivery models, practitioners can select the aspects of the evidence most relevant to their context.
Conclusion
Overall, there is evidence that telegenetic counseling is an acceptable alternative, and a useful adjunct to in-person appointments in terms of patient satisfaction, psychosocial outcomes, and knowledge gained. There is very limited evidence on the provision of services other than genetic counseling via videoconferencing. The majority of the literature is in the field of cancer genetic counseling, but results are similar in cardiogenetic, prenatal, and pediatric counseling (though there are few studies for these disciplines). In the subgroup of studies looking at videoconferencing versus telephone calls there was some evidence for a trend toward increased knowledge gain and greater improvement in psychosocial outcomes in the videoconferencing group; however, larger studies are needed. Significant gaps in the literature remain, and further research is needed particularly regarding pediatric genetic services, and longer-term outcomes including postcounseling uptake of screening or testing services, as well as the delivery of services other than counseling such as consultations requiring physical examination. If these models are to be implemented at a wider scale it is also important to ensure that they are done so equitably, and do not exacerbate existing health-care inequalities.
The majority of the available evidence involves models of telegenetics that require the patient to attend a remote health-care facility, often with the aid of local staff in utilizing the videoconferencing equipment, which is less relevant to the infection control requirements of the COVID-19 pandemic. Further research is needed into the feasibility and accessibility of telegenetic services provided to patients in their homes, and evaluation of service provided during the COVID-19 pandemic will likely provide vital insights.
Data availability
The data sets used and/or analyzed during the current study are available from the corresponding author on request.
References
Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth 2009 (Global Observatory for eHealth Series, Volume 2). World Health Organization. 2010.
Vrečar, I., Hristovski, D. & Peterlin, B. Telegenetics: an update on availability and use of telemedicine in clinical genetics service. J. Med. Syst. 41, 1–4 (2017).
Cohen, S. A. et al. Identification of genetic counseling service delivery models in practice: a report from the NSGC Service Delivery Model Task Force. J. Genet. Couns. 22, 411–421 (2013).
Hilgart, J. S., Hayward, J. A., Coles, B. & Iredale, R. Telegenetics: a systematic review of telemedicine in genetics services. Genet. Med. 14, 765–776 (2012).
Terry, A. B. et al. Clinical models of telehealth in genetics: a regional telegenetics landscape. J. Genet. Couns. 28, 673–691 (2019).
Zierhut, H. A., MacFarlane, I. M., Ahmed, Z. & Davies, J. Genetic counselors’ experiences and interest in telegenetics and remote counseling. J. Genet. Couns. 27, 329–338 (2018).
McCuaig, J. et al. Next-generation service delivery: a scoping review of patient outcomes associated with alternative models of genetic counseling and genetic testing for hereditary cancer. Cancers (Basel). 10, 435 (2018).
Otten, E., Birnie, E., Lucassen, A. M., Ranchor, A. V. & Van Langen, I. M. Telemedicine uptake among genetics professionals in Europe: room for expansion. Eur. J. Hum. Genet. 24, 157–163 (2016).
Ritchie, J. B. et al. Utilization of health information technology among cancer genetic counselors. Mol. Genet. Genomic Med. 8, e1315 (2020).
Bidmead, E. & Marshall, A. Covid-19 and the ‘new normal’: are remote video consultations here to stay? Br. Med. Bull. 135, 16–22 (2020).
Fisk, M., Livingstone, A. & Pit, S. W. Telehealth in the context of COVID-19: changing perspectives in Australia, the United Kingdom, and the United States. J. Med. Internet Res. 22, e19264 (2020).
Ramaswamy, A. et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J. Med. Internet Res. 22, e20786 (2020).
Vora, N. L., Hardisty, E., Coviello, E. & Stuebe, A. Telehealth to provide prenatal genetics services: Feasibility and importance revealed during global pandemic. Prenat. Diagn. 40, 1040–1041 (2020).
Pagliazzi, A. et al. Genetic counseling during COVID‐19 pandemic: Tuscany experience. Mol. Genet. Genomic Med. 8, e1433 (2020).
Hancock, M. The future of healthcare. Gov.uk. https://www.gov.uk/government/speeches/the-future-of-healthcare (2020).
Sterne, J. A. C. et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 366, l4898 (2019).
Ottawa Hospital Research Institute. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2021).
Bradbury, A. R. et al. Uptake of genetic testing and outcomes in a randomized study of remote genetic services as compared to usual care in community practices without genetic providers. J. Clin. Oncol. 36, 6506–6506 (2018).
Bradbury, A. R. Connect 4 APOE: a randomized study of phone versus videoconference delivery of APOE genotype disclosure in the Generation Study. Alzheimer’s Dement. 12, P1581 https://doi.org/10.1016/j.jalz.2019.09.020 (2019).
Voils, C. I., Venne, V. L., Weidenbacher, H., Sperber, N. & Datta, S. Comparison of telephone and televideo modes for delivery of genetic counseling: a randomized trial. J. Genet. Couns. 27, 339–348 (2018).
Abrams, D. J. & Geier, M. R. A comparison of patient satisfaction with telehealth and on-site consultations: a pilot study for prenatal genetic counseling. J. Genet. Couns. 15, 199–205 (2006).
Otten, E., Birnie, E., Ranchor, A. V. & Van Langen, I. M. Telegenetics use in presymptomatic genetic counselling: patient evaluations on satisfaction and quality of care. Eur. J. Hum. Genet. 24, 513–520 (2016).
Otten, E., Birnie, E., Ranchor, A. V. & Van Langen, I. M. Online genetic counseling from the providers’ perspective: counselors’ evaluations and a time and cost analysis. Eur. J. Hum. Genet. 24, 1255–1261 (2016).
Zilliacus, E. M. et al. Are videoconferenced consultations as effective as face-to-face consultations for hereditary breast and ovarian cancer genetic counseling? Genet. Med. 13, 933–941 (2011).
Wenger, T. L. et al. Telemedicine for genetic and neurologic evaluation in the neonatal intensive care unit. J. Perinatol. 34, 234–240 (2014).
Buchanan, A. H. et al. Randomized trial of telegenetics vs. in-person cancer genetic counseling: cost, patient satisfaction and attendance. J. Genet. Couns. 24, 961–970 (2015).
Solomons, N., Lamb, A. E., Lucas, F. L., McDonald, E. F. & Miesfeldt, S. Examination of the patient-focused impact of cancer telegenetics among a rural population: comparison with traditional in-person services. Telemed. e-Health. 24, 130–138 (2018).
Spielberger, C. D., Gorsuch, R. L., Lushene, R., Vagg, P. R., & Jacobs, G. A. Manual for the State-Trait Anxiety Inventory. (Consulting Psychologists Press, Palo Alto, CA, 1983).
Coelho, J. J., Arnold, A., Nayler, J., Tischkowitz, M. & MacKay, J. An assessment of the efficacy of cancer genetic counselling using real-time videoconferencing technology (telemedicine) compared to face-to-face consultations. Eur. J. Cancer. 41, 2257–2261 (2005).
Meiser, B. et al. Risk perceptions and knowledge of breast cancer genetics in women at increased risk of developing hereditary breast cancer. Psychol. Health. 16, 297–311 (2001).
Wenger, T. L. et al. Telemedicine for genetic and neurologic evaluation in the neonatal intensive care unit. J. Perinatol. 34, 234–240 (2014).
Bradbury, A. et al. Utilizing remote real-time videoconferencing to expand access to cancer genetic services in community practices: a multicenter feasibility study. J. Med. Internet Res. 18, e23 (2016).
Mette, L. A. et al. Reaching high-risk underserved individuals for cancer genetic counseling by video-teleconferencing. J. Community Support. Oncol. 14, 162–168 (2016).
Baumanis, L., Evans, J. P., Callanan, N. & Susswein, L. R. Telephoned BRCA1/2 genetic test results: Prevalence, practice, and patient satisfaction. J. Genet. Couns. 18, 447–463 (2009).
Lam, K., Lu, A. D., Shi, Y. & Covinsky, K. E. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern. Med. 180, 1389–1391 (2020).
Jeganathan, S. et al. Adherence and acceptability of telehealth appointments for high risk obstetrical patients during the COVID-19 pandemic. Am. J. Obstet. Gynecol. MFM. 2, 100233 (2020).
Hopper, B., Buckman, M. & Edwards, M. Evaluation of satisfaction of parents with the use of videoconferencing for a pediatric genetic consultation. Twin Res. Hum. Genet. 14, 343–346 (2011).
Acknowledgements
Many thanks to Frances Elmslie, Consultant Clinical Geneticist at St George’s University Hospital NHS Foundation Trust, for her input in paper revisions.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
E.G.B. and I.W. contributed equally to this study. E.G.B., I.R., E.S., and J.H. developed the concept. E.G.B., E.R.B., A.M., and I.W. screened titles, abstracts, and full papers. E.G.B. and I.W. extracted data and constructed tables. E.G.B. and I.W. drafted the report and all authors contributed to amending of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Brown, E.G., Watts, I., Beales, E.R. et al. Videoconferencing to deliver genetics services: a systematic review of telegenetics in light of the COVID-19 pandemic. Genet Med 23, 1438–1449 (2021). https://doi.org/10.1038/s41436-021-01149-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-021-01149-2
This article is cited by
-
Cascade genetic testing for hereditary cancer syndromes: a review of barriers and breakthroughs
Familial Cancer (2024)
-
The role of virtual consultations in cancer genetics: challenges and opportunities introduced by the COVID-19 pandemic
BJC Reports (2023)
-
Barriers to Genetic Testing Faced by Pediatric Subspecialists in Autism Spectrum Disorders
Advances in Neurodevelopmental Disorders (2023)
-
The TeleKidSeq pilot study: incorporating telehealth into clinical care of children from diverse backgrounds undergoing whole genome sequencing
Pilot and Feasibility Studies (2023)
-
A systematic review of geographical inequities for accessing clinical genomic and genetic services for non-cancer related rare disease
European Journal of Human Genetics (2022)