Abstract
Purpose
Cerebrotendinous xanthomatosis (CTX) is a treatable hereditary disorder caused by the deficiency of sterol 27-hydroxylase, which is encoded by the CYP27A1 gene. Different newborn screening biomarkers for CTX have been described, including 7α,12α-dihydroxy-4-cholesten-3-one (7α12αC4), 5β-cholestane-3α,7α,12α,25-tetrol glucuronide (GlcA-tetrol), the ratio of GlcA-tetrol to tauro-chenodeoxycholic acid (t-CDCA) (GlcA-tetrol/t-CDCA), and the ratio of tauro-trihydroxycholestanoic acid (t-THCA) to GlcA-tetrol (t-THCA/GlcA-tetrol). We set out to evaluate these screening methods in a research study using over 32,000 newborn dried blood spots (DBS).
Methods
Metabolites were extracted from DBS with methanol containing internal standard, which was then quantified by ultraperformance liquid chromatography tandem mass spectrometry (UPLC-MS/MS).
Results
The measurement of 7α12αC4 was complicated by isobaric interferences and was discontinued. A total of 32,737 newborns were screened based on the GlcA-tetrol concentration in DBS. GlcA-tetrol/t-CDCA and t-THCA/GlcA-tetrol ratios were also calculated. Newborns displaying both elevated GlcA-tetrol and GlcA-tetrol/t-CDCA ratio were considered to be screen positives. The t-THCA/GlcA-tetrol ratio was used to further distinguish CTX screen positives from Zellweger Spectrum Disorder (ZSD) screen positives. Only one newborn displayed both elevated GlcA-tetrol concentration in DBS and a typical CTX biochemical profile. This newborn was interpreted as a CTX-affected patient as CYP27A1 gene sequencing identified two known pathogenic variants.
Conclusion
The results indicate that both GlcA-tetrol and the GlcA-tetrol/t-CDCA ratio are excellent CTX biomarkers suitable for newborn screening. By characterizing the relationship of GlcA-tetrol, t-CDCA, and t-THCA as secondary markers, 100% assay specificity can be achieved.
Similar content being viewed by others
INTRODUCTION
Cerebrotendinous xanthomatosis (CTX; OMIM 213700) is a rare autosomal recessive disorder associated with the deficiency of sterol 27-hydroxylase, which is encoded by the CYP27A1 gene.1 Sterol 27-hydroxylase is involved in the biosynthesis of the primary bile acids, cholic acid (CA) and chenodeoxycholic acid (CDCA), from cholesterol.1 Biallelic pathogenic CYP27A1 variants result in deficiency of the primary bile acids, CA and CDCA, and the accumulation of bile acid pathway intermediates and derived metabolites, such as cholestanol and bile alcohols. This causes a progressive, mainly neurological phenotype. Symptoms during infancy and childhood can include neonatal cholestasis, liver failure, intractable diarrhea, bilateral cataracts, and developmental delay.2,3 CTX in adults is characterized by the development of tendon xanthomas and progressive neuropsychiatric symptoms, including pyramidal and cerebellar signs, peripheral neuropathy, and dementia from the second or third decade onward. The development of symptoms can be halted or prevented by supplementation with CDCA, which downregulates both bile acid and cholesterol synthesis through a negative feedback mechanism, thereby preventing the accumulation of cholesterol and cholestanol.4 The prognosis of CTX is good when therapy is started early, but is less favorable when initiated at a later age.5 Unfortunately, due to the slow progressive nature of CTX, there is often a long diagnostic delay, which negatively affects the treatment outcome of patients as irreversible neurological damage has already occurred. Based on allele frequencies of proven pathogenic variants, CTX is believed to be underdiagnosed.6 Since an early start of therapy can prevent the neurological phenotype completely, and patients are expected to remain symptom-free if treatment is started immediately after neonatal diagnosis, CTX is considered to be an excellent candidate disease for newborn screening programs.3,5,7,8
Disease associated metabolites (and metabolite ratios) have been successfully used to test newborn dried blood spots (DBS) for CTX.9,10 DeBarber et al. demonstrated that 7α,12α-dihydroxy-4-cholesten-3-one (7α12αC4), a bile acid synthesis intermediate known to be elevated in CTX, could be successfully used to identify newborns that developed CTX later in life (CTX newborns).9 Quantification of 7α12αC4 was performed with a derivatization step to improve liquid chromatography tandem mass spectrometry (LC-MS/MS) method sensitivity, or more recently, without derivatization but using a more sensitive LC-MS/MS instrument.7,9 The second CTX newborn screening method was described by Vaz et al. and is based on measuring the amount of a bile alcohol, 5β-cholestane-3α,7α,12α,25-tetrol glucuronide (GlcA-tetrol), as well as the ratio of GlcA-tetrol to tauro-chenodeoxycholic acid (t-CDCA) in DBS using flow-injection MS/MS.10 It was also recommended to measure the tauro-trihydroxycholestanoic acid (t-THCA) level and calculate the t-THCA/GlcA-tetrol ratio as a secondary disease indicator to distinguish CTX patients from patients with cholestasis and Zellweger Spectrum Disorder (ZSD).10,11
In this study, we evaluated both the practical analytical aspects and the newborn screening potential for these metabolites and metabolite ratios in a research study using DBS from >32,000 de-identified newborns.
MATERIALS AND METHODS
DBS samples
This study using DBS from de-identified newborns was approved by the Washington State Institutional Review Board. DBS were shared by the Washington State Department of Health (WA DOH) after being stored for 30–60 days of life at room temperature (DBS stored <30 days cannot be shared for research according to the policy of the WA DOH). De-identified DBS from 1 CTX newborn, 8 symptomatic CTX patients and 1 ZSD patient were acquired from the Oregon Health and Science University and the Amsterdam UMC, location AMC (Amsterdam, The Netherlands). Results from these patients and random newborns are summarized in Table S1. K2EDTA whole blood was collected from a consenting healthy adult. Negative control DBS were prepared by spotting the K2EDTA whole blood on Whatmann 903 protein saver cards (Standard Operating Protocol, Supplementary Information). Positive control DBS (GlcA-tetrol-spiked DBS) were prepared by diluting GlcA-tetrol stock solution in methanol 100-fold to K2EDTA whole blood and spotting the spiked blood on Whatmann 903 protein saver cards (Standard Operating Protocol, Supplementary Information).
Methods
The detailed protocol for the assay is provided in the Supplementary Information. In short, metabolites (GlcA-tetrol, t-CDCA, and t-THCA) were extracted from a 3-mm DBS punch with methanol containing the internal standard (d6-GlcA-tetrol, Retrophin Inc.). After a 4-hour extraction, the sample was centrifuged, and the supernatant was analyzed by ultraperformance liquid chromatography tandem mass spectrometry (UPLC-MS/MS), where the analytes and the internal standard were detected by multiple reaction monitoring (MRM) in negative electrospray ionization mode. Chromatographic peaks were integrated automatically using the TargetLynx software (Waters Corp.) and were inspected manually.
The concentration of GlcA-tetrol in blood (nM) was calculated by multiplying the ion ratio of the analyte to the internal standard by the nmole of the internal standard added to the assay, then dividing by the volume of blood (L), assuming each 3-mm DBS punch contained 3.2 μL blood. The GlcA-tetrol/t-CDCA biomarker ratio was calculated by dividing the MRM integral area of the GlcA-tetrol peak by that of the t-CDCA peak. The t-THCA/GlcA-tetrol biomarker ratio was calculated by dividing the MRM integral area of the t-THCA peak by that of the GlcA-tetrol peak.
Next-generation sequencing of the CYP27A1 gene was conducted on a second 3-mm DBS punch from newborns that were considered to be at risk of CTX at Molecular Vision Laboratory (Hillsboro, OR).
RESULTS
Analysis of 7α12αC4 concentration in DBS
A new derivatization method using O-ethylhydroxylamine was developed to improve the MS/MS response of 7α12αC4 (details provided in the Supplementary Information), since the original method developed by DeBarber et al. utilized a commercial kit that is too costly for large-scale screening. 7α12αC4 was derivatized via oxime bond formation, which led to a threefold increase in the detector response compared with the underivatized 7α12αC4. Although the original derivatization method was two times more sensitive, derivatization with O-ethylhydroxylamine afforded sufficient signal on our platform.
The 7α12αC4 concentration in DBS from 8 CTX patients, 1 CTX newborn, 1 ZSD patient, and 2033 random newborns is shown in Fig. S1 and Table S1. During the study, however, it became apparent that the quantification of O-ethylhydroxylamine derivatized 7α12αC4 in newborn DBS suffered from interference of isobaric species eluting closely to the target compound. The abundance of these blood-derived isobars varied greatly between newborns, though they did not pose a major issue when analyzing patient DBS. Therefore, accurate quantification of the derivatized 7α12αC4 was impossible without considerably lengthening the analysis to fully separate the interfering substance(s) from the analyte. We decided to discontinue the quantification of 7α12αC4 and to focus on the quantification of GlcA-tetrol and the determination of the GlcA-tetrol/t-CDCA ratio.
Analysis of GlcA-tetrol concentration and GlcA-tetrol/t-CDCA ratio in DBS
GlcA-tetrol, t-CDCA, and t-THCA were simultaneously extracted from the DBS and analyzed without derivatization by UPLC-MS/MS using negative electrospray ionization mode. The sample injection-to-injection time was 2.5 minutes, allowing more than 400 samples to be analyzed per day per instrument. Fig. S2 shows the UPLC-MS/MS chromatogram of GlcA-tetrol, t-CDCA, and t-THCA in a CTX newborn, a single normal newborn, and a ZSD patient. GlcA-tetrol was highly elevated in the CTX newborn, whereas it was undetectable in the normal newborn. The ZSD patient showed a moderate GlcA-tetrol peak that was 4.5-fold smaller than that in the CTX newborn. t-CDCA was reduced by five to sevenfold in the CTX newborn and the ZSD patient compared with the normal newborn. t-THCA was highly elevated in the ZSD patient and undetectable in the CTX newborn and the normal newborn. Biomarker levels and biomarker ratios measured in the CTX and ZSD patients as well as the 32,737 newborns are summarized in Table S1.
Quantification of GlcA-tetrol was carried out using d6-GlcA-tetrol as the internal standard. The linearity of the analyte assay response and the analyte recovery were assessed using a series of GlcA-tetrol-spiked DBS ranging from 0 nM to 2000 nM. As shown in Fig. S3, the assay displayed good linearity (R2 > 0.99), with an overall recovery of 71% based on the slope of the calibration curve. The limit of detection for the GlcA-tetrol assay was estimated to be 38 nM, which was calculated as described (details provided in Supplementary Information).12 The assay also displayed good intra- and interassay imprecision (<10%), which was evaluated using adult DBS spiked with 2000 nM GlcA-tetrol, with ten replicates measured on five nonconsecutive days (Table S2). We did not investigate the stability of GlcA-tetrol in DBS, as previous studies demonstrated that GlcA-tetrol is stable for at least 3 weeks in DBS stored at room temperature.7,10 This stability study is adequate for our studies since the DBS were stored for up to 1–2 months at room temperature prior to analysis. No external calibration was used in our routine analysis; the GlcA-tetrol concentration in DBS was calculated using the internal standard. Positive control and negative control (adult) DBS, with/without 2000 nM GlcA-tetrol spike, were included in our daily analysis to ensure the consistency of the assay (Standard Operating Protocol, Supplementary Information).
Fig. S4 displays the GlcA-tetrol/t-CDCA ratio in 8 CTX patients (median: 15.51, range: 2.20–63.64), 1 CTX newborn (1.18), 1 ZSD patient (0.38), and 2000 random newborns (median: 0.01, range: 0–0.26). The GlcA-tetrol/t-CDCA ratio in random newborns did not vary substantially and was close to zero because GlcA-tetrol was barely detectable in most newborns, while t-CDCA was abundant. On the contrary, the GlcA-tetrol/t-CDCA ratio varied over a large range in CTX patients and CTX newborns because t-CDCA, the denominator of the ratio, was reduced to values close to zero. Compared with the 2000 random newborns, the GlcA-tetrol/t-CDCA ratio was elevated significantly in the CTX patients and the CTX newborn, while only elevated moderately in the ZSD patient (Fig. S4).
GlcA-tetrol as the primary screening marker for CTX
First, we used the GlcA-tetrol concentration as the primary screening filter. The screening cutoff was set at 500 nM based on the data on the GlcA-tetrol concentration in DBS from 3 CTX newborns reported by DeBarber et al. (638.9–1176 nM).7 Newborns with GlcA-tetrol concentration above the cutoff were considered at risk of CTX. A total of 32,737 newborns were screened, 6 of whom (0.018%) had elevated GlcA-tetrol above the 500 nM cutoff (Table 1). Results from these six newborns are summarized in Table 2.
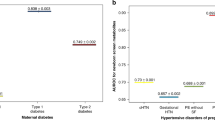
To further improve the specificity of the screening, GlcA-tetrol/t-CDCA and t-THCA/GlcA-tetrol ratios were implemented as secondary screening markers. The proposed screening algorithm for CTX is shown in Fig. 1a. Only newborns displaying both elevated GlcA-tetrol concentration and GlcA-tetrol/t-CDCA ratio were considered as screen positives (Fig. 1a). Since an elevated t-THCA/GlcA-tetrol ratio was indicative of ZSD, this metabolite ratio was used to distinguish CTX screen positives from ZSD screen positives (Fig. 1a).10 The cutoff for the GlcA-tetrol/t-CDCA ratio was set at 0.3, based on the results reported in this study (1 CTX newborn, 1.18, Table S1) and published earlier (5 CTX newborns, 0.33–138).7,10 The cutoff for the t-THCA/GlcA-tetrol ratio was set at 4, based on results reported in this study (1 ZSD patient, 11.8, Table S1) and published earlier (3 ZSD patients, 10.5 to 38).10
Following this algorithm, only 2 of the 6 newborns with elevated GlcA-tetrol had GlcA-tetrol/t-CDCA ratio above 0.3 (subject 3 and 5, Table 2). The rest were not considered to be potential CTX patients after applying the GlcA-tetrol/t-CDCA ratio as the secondary filter. In addition, the t-CDCA peaks in subjects 1, 2, and 4 (Table 2) were higher than 99.9% of the newborns screened in the study, suggesting cholestasis.7,13 Subject 5 (Table 2) had both moderately elevated GlcA-tetrol (599.6 nM) and GlcA-tetrol/t-CDCA ratio (0.46) but highly elevated t-THCA/GlcA-tetrol ratio (9.88), suggesting ZSD. No discernible t-THCA peak was found in subjects 2 and 3, whereas t-THCA was slightly elevated in subjects 1, 4, and 6 (Table 2). Thus, only subject 3 in Table 2 fits the biochemical profile of CTX and was considered to be CTX screen positive.
This single newborn (subject 3, Table 2) that was suggested to be CTX-affected based on the absolute abundance of GlcA-tetrol as well as GlcA-tetrol/t-CDCA and t-THCA/GlcA-tetrol ratios was submitted to genotyping using a reserved 3-mm punch from the same DBS used for the UPLC-MS/MS analysis. DNA sequencing of the CYP27A1 gene revealed two known pathogenic variants: NM_000784.3(CYP27A1):c.1214G>A (p.Arg405Gln) and NM_000784.3(CYP27A1):c.1415G>C (p.Gly472Ala).6 Therefore, subject 3 in Table 2 was interpreted as a CTX patient.
GlcA-tetrol/t-CDCA ratio as the primary screening marker for CTX
Alternatively, the GlcA-tetrol/t-CDCA ratio could also be used as the primary screening marker for CTX. The screening cutoff was set at 0.3 (see previous section). Newborns with a GlcA-tetrol/t-CDCA ratio above 0.3 were considered at risk of CTX. Among the 32,737 newborns, 10 (0.031%) displayed a GlcA-tetrol/t-CDCA ratio above the cutoff. Results from these ten newborns are summarized in Table 3.
GlcA-tetrol concentration (cutoff: 500 nM) as well as the t-THCA/GlcA-tetrol ratio (cutoff: 4) were both implemented as secondary markers to improve the specificity of the screening. The cutoff establishment was elaborated in the previous section. The screening algorithm is shown in Fig. 1b. Following this screening algorithm, subject 1 in Table 3 (same as subject 3, Table 2) was identified as CTX screen positive and subject 3 in Table 3 (same as subject 5, Table 2) was identified as ZSD screen positive. The remainder were considered as screen negatives. Therefore, this screening algorithm (Fig. 1b) identified the same CTX and ZSD screen positives as the previous algorithm (Fig. 1a), indicating that the GlcA-tetrol/t-CDCA ratio is also a good first-tier marker for newborn screening of CTX.
Assessment of the screening sensitivity
To evaluate the sensitivity of the screening, the GlcA-tetrol/t-CDCA ratio from the top 1,000 newborns ranked according to elevated GlcA-tetrol concentration was plotted (Fig. 2a). Figure 2b displays the GlcA-tetrol concentration from the top 1,000 newborns ranked according to the GlcA-tetrol/t-CDCA ratio. In both cases, two newborns are found to be well separated from the remaining 998 newborns. These two are the CTX patient and the potential ZSD patient identified as described above according to the two screening algorithms (Fig. 1). Based on this clear separation, we did not carry out CYP27A1 sequencing on additional newborns.
The top 1,000 newborns with the highest (a) GlcA-tetrol concentration; and (b) GlcA-tetrol/t-CDCA ratio. The horizontal dashed lines indicate the GlcA-tetrol/t-CDCA ratio cutoff at 0.3. The vertical dashed lines indicate the GlcA-tetrol cutoff at 500 nM. Newborns that fall into the upper-right quadrant are considered screen positives. The screen positive indicated by a diamond (◊) is the ZSD screen positive (subject 5 in Table 2, subject 3 in Table 3). The screen positive indicated by a square (□) is the CTX screen positive (subject 3 in Table 2, subject 1 in Table 3).
DISCUSSION
7α12αC4 was not considered to be useful as a primary marker for CTX in this study due to the endogenous interferences using our derivatization approach and the requirement for a short analysis time per newborn. However, it should be noted that the isobar problem can be resolved by using an enhanced gradient to fully separate the derivatized 7α12αC4 from the isobars or by quantifying the marker without derivatization using a less sensitive but more specific MRM channel as described by DeBarber et al.7 This requires a longer sample turnaround time and/or a more sophisticated mass spectrometer. Nevertheless, measurement of 7α12αC4 can still be used in the future as a secondary biomarker. In our study, we had only one reserved DBS punch after the first-tier UPLC-MS/MS analysis, and we opted to use it for genotyping analysis.
The GlcA-tetrol/t-CDCA ratio and GlcA-tetrol from the CTX newborn were significantly elevated compared with random newborns, but they were less elevated than levels measured in older, untreated CTX patients (Fig. S4 and Table S1). Similar trends were seen in previous reports.7,10 Although little is known about the correlation between blood glucuronide–conjugated bile alcohol concentration and age, it is well established that glucuronidation capacity is low in neonates because of the low activity of UDP-glucuronosyltransferase, which increases with age.14 This likely leads to lower glucuronide-conjugated bile alcohol levels in neonates, which explains the lower GlcA-tetrol concentration seen in CTX newborns compared with older CTX patients. In addition, it was reported that in neonates the serum t-CDCA concentration is higher than that in children and adolescents.15 Together, this would explain the lower GlcA-tetrol/t-CDCA ratios observed in CTX newborns compared with older CTX patients, as the GlcA-tetrol/t-CDCA ratios in CTX newborns are calculated by dividing the lower GlcA-tetrol level by the higher t-CDCA level. As all newborns have lower blood concentrations of GlcA-tetrol in combination with lower GlcA-tetrol/t-CDCA ratios, we do not expect a negative effect on the discriminative power of the CTX newborn screening method described here.
GlcA-tetrol was found to be an excellent marker for CTX, as only 6 of 32,737 newborns (0.018%) had a GlcA-tetrol level above the 500 nM screening cutoff. The screen positive rate was further reduced when GlcA-tetrol/t-CDCA and t-THCA/GlcA-tetrol ratios were taken into consideration. Since t-CDCA and t-THCA are extracted together with GlcA-tetrol, there is no need for an additional DBS punch nor a separate analysis. Only 1 of 32,737 newborns was considered to be CTX screen positive after applying the GlcA-tetrol/t-CDCA and t-THCA/GlcA-tetrol ratios as secondary screening markers. CYP27A1 gene sequencing of the newborn of interest revealed two pathogenic variants, showing 100% assay specificity.
One concern with the 500 nM GlcA-tetrol screening cutoff is that it is based on published data from only three CTX newborns, and it is difficult to rule out the possibility of false negatives in the future. However, even if the cutoffs for GlcA-tetrol and the GlcA-tetrol/t-CDCA ratio are lowered from 500 nM to 300 nM and from 0.3 to 0.2, respectively, only 2 newborns would result (subjects 3 and 5 in Table 2 or subject 1 and 3 in Table 3). One of these two newborns is the confirmed CTX patient and the other is the suspected ZSD patient, whom can be identified by using the t-THCA/GlcA-tetrol ratio. This gives us confidence that even in extreme cases where the screening cutoffs for GlcA-tetrol and GlcA-tetrol/t-CDCA need to be lowered significantly, the false positive rate is not expected to increase substantially. Data from future prospective pilot studies and CTX-affected newborns identified will help to better define the affected range and confirm the optimal cutoff for GlcA-tetrol concentration and the GlcA-tetrol/t-CDCA ratio.
Alternatively, using the GlcA-tetrol/t-CDCA ratio as the first-tier screening marker is also feasible based on our results. The screen positive rate using GlcA-tetrol/t-CDCA ratio as the primary marker is 0.031% and is acceptable for a newborn screening test compared with other active newborn screening programs.16,17,18 By implementing GlcA-tetrol and t-THCA/GlcA-tetrol as secondary markers, the screen positive rate can be further reduced, as shown in this study. Vaz et al. originally proposed to screen CTX by measuring the GlcA-tetrol/t-CDCA ratio using flow-injection MS/MS without using an internal standard.10 The benefit of this approach is that most screening laboratories are only equipped with flow-injection MS/MS, not LC-MS/MS. Most flow-injection MS/MS based screening tests (i.e., amino acid, acyl-carnitine, and succinylacetone analysis), however, are carried out in positive electrospray ionization mode in contrast to the negative mode required for our CTX screening assay. This necessitates a separate analysis for CTX. Furthermore, endogenous isobars with GlcA-tetrol and t-CDCA can skew the result of flow-injection MS/MS analysis, which is the case for the quantification of C26:0-lysophosphatidylcholine for X-linked adrenoleukodystrhophy.19 It remains to be established how this will affect the results for CTX screening, and the flow-injection MS/MS method needs to be tested in a larger newborn population. Even if flow-injection MS/MS is used as the first-tier NBS test, a secondary LC-MS/MS analysis with suitable internal standards is expected to be required to quantify GlcA-tetrol, t-CDCA, and t-THCA.
One advantage of quantifying the absolute concentration of GlcA-tetrol using a chemically identical but isotopic differentiated internal standard is that the screening cutoff is expected to be comparable across multiple platforms and between laboratories. Researchers who are interested in setting up the assay can contact A. DeBarber (debarber@ohsu.edu) for the reagents (GlcA-tetrol and d6-GlcA-tetrol). It should also be noted that in this study, the GlcA-tetrol/t-CDCA ratio was calculated by dividing the integral peak area of GlcA-tetrol by that of t-CDCA. Since GlcA-tetrol and t-CDCA did not coelute on the UPLC column (Fig. S2), they are expected to suffer from different extents of matrix effects (ion suppression). For flow-injection MS/MS analysis, this issue is less relevant as analytes all pass into the mass spectrometer together, though it can suffer from interference from isobars. Therefore, the measured GlcA-tetrol/t-CDCA ratio (and affected range) may differ between LC-MS/MS methods and flow-injection MS/MS methods. Although not used in the current study, deuterated t-CDCA is commercially available from Toronto Research Chemicals (catalog number T008133), and some assay improvement may result if the GlcA-tetrol/t-CDCA ratio is calculated by dividing the measured GlcA-tetrol/d6-GlcA-tetrol ratio by the measured t-CDCA/deuterated t-CDCA ratio.
Conclusion
The research study presented here demonstrates that newborn screening for CTX is feasible with an exceptionally low false positive rate. We propose that CTX be screened based on either the GlcA-tetrol concentration or the GlcA-tetrol/t-CDCA ratio in DBS. A comprehensive profiling of GlcA-tetrol, t-CDCA, and t-THCA is required as a secondary filter to improve the specificity of the screening. Among the 32,737 random newborns screened, only 1 had a biochemical abnormality—as defined in this study—that was indicative of CTX. DNA sequencing of the CYP27A1 gene revealed two previously reported pathogenic variants, and together with the biochemical data, strongly suggests that this newborn will develop CTX disease. Our study demonstrated that newborn screening for CTX is feasible in a real-world scenario.
References
Verrips A, Hoefsloot LH, Steenbergen GC, et al. Clinical and molecular genetic characteristics of patients with cerebrotendinous xanthomatosis. Brain. 2000;123:908–919.
Gong J-Y, Setchell KD, Zhao J, et al. Severe neonatal cholestasis in cerebrotendinous xanthomatosis: genetics, immunostaining, mass spectrometry. J Pediatr Gastroenterol Nutr. 2017;65:561–568.
Salen G, Steiner RD. Epidemiology, diagnosis, and treatment of cerebrotendinous xanthomatosis (CTX). J Inherit Metab Dis. 2017;40:771–781.
Pierre G, Setchell K, Blyth J, et al. Prospective treatment of cerebrotendinous xanthomatosis with cholic acid therapy. J Inherit Metab Dis. 2008;31:241–245.
Yahalom G, Tsabari R, Molshatzki N, et al. Neurological outcome in cerebrotendinous xanthomatosis treated with chenodeoxycholic acid: early versus late diagnosis. Clin Neuropharmacol. 2013;36:78–83.
Appadurai V, DeBarber A, Chiang PW, et al. Apparent underdiagnosis of cerebrotendinous xanthomatosis revealed by analysis of ~60,000 human exomes. Mol Genet Metab. 2015;116:298–304.
DeBarber AE, Kalfon L, Fedida A, et al. Newborn screening for cerebrotendinous xanthomatosis is the solution for early identification and treatment. J Lipid Res. 2018;59:2214–2222.
Berginer VM, Gross B, Morad K, et al. Chronic diarrhea and juvenile cataracts: think cerebrotendinous xanthomatosis and treat. Pediatrics. 2009;123:143–147.
DeBarber AE, Luo J, Star-Weinstock M, et al. A blood test for cerebrotendinous xanthomatosis with potential for disease detection in newborns. J Lipid Res. 2014;55:146–154.
Vaz FM, Bootsma AH, Kulik W, et al. A newborn screening method for cerebrotendinous xanthomatosis using bile alcohol glucuronides and metabolite ratios. J Lipid Res. 2017;58:1002–1007.
Gustafsson J, Sisfontes L, Björkhem I. Diagnosis of Zellweger syndrome by analysis of bile acids and plasmalogens in stored dried blood collected at neonatal screening. J Pediatr. 1987;111:264–267.
Armbruster DA, Pry T. Limit of blank, limit of detection and limit of quantitation. Clin Biochem Rev. 2008;29 Suppl 1:S49.
Mills KA, Mushtaq I, Johnson AW, et al. A method for the quantitation of conjugated bile acids in dried blood spots using electrospray ionization-mass spectrometry. Pediatr Res. 1998;43:361–368.
Neumann E, Mehboob H, Ramirez J, et al. Age-dependent hepatic UDP-glucuronosyltransferase gene expression and activity in children. Front Pharmacol. 2016;7:437.
Jahnel J, Zohrer E, Scharnagl H, et al. Reference ranges of serum bile acids in children and adolescents. Clin Chem Lab Med. 2015;53:1807–1813.
Hopkins PV, Klug T, Vermette L, et al. Incidence of 4 lysosomal storage disorders from 4 years of newborn screening. JAMA Pediatr. 2018;172:696–697.
Burton BK, Charrow J, Hoganson GE, et al. Newborn screening for lysosomal storage disorders in Illinois: the initial 15-month experience. J Pediatr. 2017;190:130–135.
Lee S, Clinard K, Young SP, et al. Evaluation of X-Linked adrenoleukodystrophy newborn screening in North Carolina. JAMA Netw Open. 2020;3:e1920356.
Turgeon CT, Moser AB, Morkrid L, et al. Streamlined determination of lysophosphatidylcholines in dried blood spots for newborn screening of X-linked adrenoleukodystrophy. Mol Genet Metab. 2015;114:46–50.
Acknowledgements
We are grateful to Retrophin, Inc. for providing the internal standard d6-GlcA-tetrol. This work was supported by a grant from the National Institutes of Health (R01 DK067859).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
F.M.V.ʼs filed patents include EP3593143, CN110612448, CA3055659, AU2018231379. M.H.G. is a cofounder of GelbChem, LLC, and a consultant for PerkinElmer Corp. M.H.Gʼs awarded and filed patents include US20140249054A1, US20160298166A1, US8802833B2, EP2191006B1, and EP2385950B1. The other authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hong, X., Daiker, J., Sadilek, M. et al. Toward newborn screening of cerebrotendinous xanthomatosis: results of a biomarker research study using 32,000 newborn dried blood spots. Genet Med 22, 1606–1612 (2020). https://doi.org/10.1038/s41436-020-0846-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-0846-x
Keywords
This article is cited by
-
Living with Cerebrotendinous Xanthomatosis: Patient, Caregiver, and Expert Perspectives
Advances in Therapy (2024)
-
Allelic prevalence and geographic distribution of cerebrotendinous xanthomatosis
Orphanet Journal of Rare Diseases (2023)
-
33-jähriger Patient mit progredienter Leukenzephalopathie, frühkindlichem Katarakt und rezidivierenden Diarrhöen
DGNeurologie (2023)
-
Expert opinion on diagnosing, treating and managing patients with cerebrotendinous xanthomatosis (CTX): a modified Delphi study
Orphanet Journal of Rare Diseases (2021)