Abstract
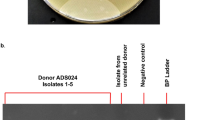
Clostridium difficile is the leading cause of antibiotic-associated nosocomial diarrhea in the developed world. When the host-associated colon microbiome is disrupted by the ingestion of antibiotics, C. difficile spores can germinate, resulting in infection. C. difficile secretes enterotoxin A (TcdA) and cytotoxin B (TcdB) that are responsible for disease pathology. Treatment options are limited as the bacterium demonstrates resistance to many antibiotics, and even with antibacterial therapies, recurrences of C. difficile are common. Actotoxumab and bezlotoxumab are human monoclonal antibodies that bind and neutralize TcdA and TcdB, respectively. In 2016, the US food and drug administration (FDA) approved bezlotoxumab for use in the prevention of C. difficile infection recurrence. To ensure the long-term expression of antibodies, gene therapy can be used. Here, adeno-associated virus (AAV)6.2FF, a novel triple mutant of AAV6, was engineered to express either actotoxumab or bezlotoxumab in mice and hamsters. Both antibodies expressed at greater than 90 μg/mL in the serum and were detected at mucosal surfaces in both models. Hundred percent of mice given AAV6.2FF-actoxumab survived a lethal dose of TcdA. This proof of concept study demonstrates that AAV-mediated expression of C. difficile toxin antibodies is a viable approach for the prevention of recurrent C. difficile infections.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015;373:287–8.
Balsells E, Shi T, Leese C, Lyell I, Burrows J, Wiuff C, et al. Global burden of Clostridium difficile infections: a systematic review and meta-analysis. J Glob Health. 2019;9:010407.
Guh AY, Mu Y, Winston LG, Johnston H, Olson D, Farley MM, et al. Trends in U.S. burden of Clostridioides difficile infection and outcomes. N Engl J Med. 2020;382:1320–30.
Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173:2039–46.
Duhalde L, Lurienne L, Wingen-Heimann SM, Guillou L, Buffet R, Bandinelli PA. The economic burden of Clostridioides difficile infection in patients with hematological malignancies in the United States: a case-control study. Infect Control Hosp Epidemiol. 2020;41:813–9.
Chopra T, Goldstein EJ. Clostridium difficile infection in long-term care facilities: a call to action for antimicrobial stewardship. Clin Infect Dis. 2015;60:S72–76.
Marshall LL, Peasah S, Stevens GA. Clostridium difficile infection in older adults: systematic review of efforts to reduce occurrence and improve outcomes. Consult Pharm. 2017;32:24–41.
De Roo AC, Regenbogen SE. Clostridium difficile Infection: an epidemiology update. Clin Colon Rectal Surg. 2020;33:49–57.
Stebel R, Vojtilová L, Husa P. Clostridium difficile infection: an update on treatment and prevention. Vnitr Lek. 2020;66:58–62.
Schäffler H, Breitrück A. Clostridium difficile—from colonization to infection. Front Microbiol. 2018;9:646.
Di Bella S, Ascenzi P, Siarakas S, Petrosillo N, di Masi A. Clostridium difficile toxins A and B: insights into pathogenic properties and extraintestinal effects. Toxins. 2016;8:134.
von Eichel-Streiber C, Boquet P, Sauerborn M, Thelestam M. Large clostridial cytotoxins-a family of glycosyltransferases modifying small GTP-binding proteins. Trends Microbiol. 1996;4:375–82.
Sun X, Savidge T, Feng H. The enterotoxicity of Clostridium difficile toxins. Toxins. 2010;2:1848–80.
Just I, Selzer J, Wilm M, von Eichel-Streiber C, Mann M, Aktories K. Glucosylation of Rho proteins by Clostridium difficile toxin B. Nature. 1995;375:500–3.
Just I, Wilm M, Selzer J, J, Rex G, von Eichel-Streiber C, Mann M, et al. The enterotoxin from Clostridium difficile (ToxA) monoglucosylates the Rho proteins. J Biol Chem. 1995;270:13932–6.
Gateau C, Couturier J, Coia J, Barbut F. How to: diagnose infection caused by Clostridium difficile. Clin Microbiol Infect. 2018;24:463–8.
Peng Z, Ling L, Stratton CW, Li C, Polage CR, Wu B, et al. Advances in the diagnosis and treatment of Clostridium difficile infections. Emerg Microbes Infect. 2018;7:15.
Curry SR, Marsh JW, Shutt KA, Muto CA, O’Leary MM, Saul MI, et al. High frequency of rifampin resistance identified in an epidemic Clostridium difficile clone from a large teaching hospital. Clin Infect Dis. 2009;48:425–9.
Dieterle MG, Rao K, Young VB. Novel therapies and preventative strategies for primary and recurrent Clostridium difficile infections. Ann N Y Acad Sci. 2019;1435:110–38.
Deshpande A, Pasupuleti V, Thota P, Pant C, Rolston DD, Hernandez AV, et al. Risk factors for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2015;36:452–60.
Rineh A, Kelso MJ, Vatansever F, Tegos GP, Hamblin MR. Clostridium difficile infection: molecular pathogenesis and novel therapeutics. Expert Rev Anti Infect Ther. 2014;12:131–50.
Bojanova DP, Bordenstein SR. Fecal transplants: what is being transferred? PLoS Biol. 2016;14:e1002503.
Daniels LM, Kufel WD. Clinical review of Clostridium difficile infection: an update on treatment and prevention. Expert Opin Pharmacother. 2018;19:1759–69.
Merrick B, Allen L, Zain NMM, Forbes B, Shawcross DL, Goldenberg SD. Regulation, risk and safety of faecal microbiota transplant. Infect Prev Pract. 2020;2:100069.
Giau VV, Lee H, An SSA, Hulme J. Recent advances in the treatment of. Infect Drug Resist. 2019;12:1597–615.
Mounsey A, Lacy Smith K, Reddy VC, Nickolich S. Clostridioides difficile Infection: update on management. Am Fam Physician. 2020;101:168–75.
Yang Z, Ramsey J, Hamza, Zhang Y, Li S, Yfantis HG, et al. Mechanisms of protection against Clostridium difficile infection by the monoclonal antitoxin antibodies actoxumab and bezlotoxumab. Infect Immunol. 2015;83:822–31.
Bézay N, Ayad A, Dubischar K, Firbas C, Hochreiter R, Kiermayr S, et al. Safety, immunogenicity and dose response of VLA84, a new vaccine candidate against Clostridium difficile, in healthy volunteers. Vaccine. 2016;34:2585–92.
de Bruyn G, Saleh J, Workman D, Pollak R, Elinoff V, Fraser NJ, et al. Defining the optimal formulation and schedule of a candidate toxoid vaccine against Clostridium difficile infection: a randomized Phase 2 clinical trial. Vaccine. 2016;34:2170–8.
CDVAX. Progress 2018. Available from: http://cdvax.org/progress/.
Babcock GJ, Broering TJ, Hernandez HJ, Mandell RB, Donahue K, Boatright N, et al. Human monoclonal antibodies directed against toxins A and B prevent Clostridium difficile-induced mortality in hamsters. Infect Immun. 2006;74:6339–47.
Steele J, Mukherjee J, Parry N, Tzipori S. Antibody against TcdB, but not TcdA, prevents development of gastrointestinal and systemic Clostridium difficile disease. J Infect Dis. 2013;207:323–30.
Corthier G, Muller MC, Wilkins TD, Lyerly D, L’Haridon R. Protection against experimental pseudomembranous colitis in gnotobiotic mice by use of monoclonal antibodies against Clostridium difficile toxin A. Infect Immunol. 1991;59:1192–5.
Markham A. Bezlotoxumab: first global approval. Drugs. 2016;76:1793–8.
Balazs AB, Chen J, Hong CM, Rao DS, Yang L, Baltimore D. Antibody-based protection against HIV infection by vectored immunoprophylaxis. Nature. 2012;481:81–84.
Zincarelli C, Soltys S, Rengo G, Rabinowitz J. Analysis of AAV serotypes 1-9 mediated gene expression and tropism in mice after systemic injection. Mol Ther. 2008;16:1073–80.
van Lieshout LP, Domm JM, Rindler TN, Frost KL, Sorensen DL, Medina SJ. A novel triple-mutant AAV6 capsid induces rapid and potent transgene expression in the muscle and respiratory tract of mice. Mol Ther Methods Clin Dev. 2018;9:323–9.
van Lieshout LP, Soule G, Sorensen D, Frost KL, He S, Tierney K, et al. Intramuscular adeno-associated virus-mediated expression of monoclonal antibodies provides 100% protection against ebola virus infection in mice. J Infect Dis. 2018;217:916–25.
Halbert C, Allen J, Miller A. Efficient mouse airway transduction following recombination between AAV vectors carrying parts of a larger gene. Nat Biotechnol. 2002;20:697–701.
van Lieshout LP, Domm JM, Wootton SK. AAV-mediated gene delivery to the lung. Methods Mol Biol. 2019;1950:361–72.
Gardner MR, Fetzer I, Kattenhorn LM, Davis-Gardner ME, Zhou AS, Alfant B, et al. Anti-drug antibody responses impair prophylaxis mediated by AAV-delivered HIV-1 broadly neutralizing antibodies. Mol Ther. 2019;27:650–60.
van den Berg FT, Makoah NA, Ali SA, Scott TA, Mapengo RE, Mutsvunguma LZ, et al. AAV-mediated expression of broadly neutralizing and vaccine-like antibodies targeting the HIV-1 envelope V2 region. Mol Ther Methods Clin Dev. 2019;14:100–12.
Best EL, Freeman J, Wilcox MH. Models for the study of Clostridium difficile infection. Gut Microbes. 2012;3:145–67.
Dekkers G, Bentlage AEH, Stegmann TC, Howie HL, Lissenberg-Thunnissen S, Zimring J, et al. Affinity of human IgG subclasses to mouse Fc gamma receptors. MAbs. 2017;9:767–73.
He X, Sun X, Wang J, Wang X, Zhang Q, Tzipori S, et al. Antibody-enhanced, Fc gamma receptor-mediated endocytosis of Clostridium difficile toxin A. Infect Immunol. 2009;77:2294–303.
Acknowledgements
We thank all those involved in the care of the animals for these studies at all institutions.
Funding
This research was funded by NSERC Discovery Grant number RGPIN-2018-04737. BAYS and ADR are both recipients of an OVC Scholarship and an Ontario Graduate Scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LPvL and SKW are inventors on a US patent for the AAV6.2FF capsid. This patent (US20190216949) is licensed to Avamab Pharma Inc., where BT and SKW are co-founders and BT serves as an executive.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guilleman, M.M., Stevens, B.A.Y., Van Lieshout, L.P. et al. AAV-mediated delivery of actoxumab and bezlotoxumab results in serum and mucosal antibody concentrations that provide protection from C. difficile toxin challenge. Gene Ther 30, 455–462 (2023). https://doi.org/10.1038/s41434-021-00236-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41434-021-00236-y
This article is cited by
-
AAV-vectored expression of monospecific or bispecific monoclonal antibodies protects mice from lethal Pseudomonas aeruginosa pneumonia
Gene Therapy (2024)
-
Antibody-based protection against respiratory syncytial virus in mice and their offspring through vectored immunoprophylaxis
Gene Therapy (2023)
-
Adeno-associated virus mediated expression of monoclonal antibody MR191 protects mice against Marburg virus and provides long-term expression in sheep
Gene Therapy (2022)