Abstract
Background
Cases of uveitis can necessitate long-term treatment resulting in recurrent follow-up appointments. Analysing the demographic distribution and patient factors influencing treatment and time spent with physicians in this population compared to other subspecialties of ophthalmology using the National Ambulatory Medical Care Survey (NAMCS) has not previously been studied.
Methods
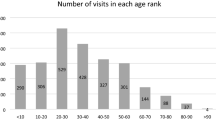
Data were extracted from the NAMCS database, a large, nationally representative survey of office-based specialists, entered between 2012–2016 and 2018. Demographics, time with physician, and payor types were compared between patients with a uveitis-related diagnosis codes versus all other ophthalmic subspecialty diagnoses.
Results
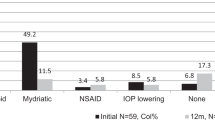
Overall, 12,870 ophthalmic patients were included of which 300 had uveitis-related diagnosis codes. Uveitis patients were more likely to be non-Caucasian (p < 0.0001 to p = 0.022), visiting the physician’s office due to flare of or treatment for a chronic medical problem (p < 0.0001 to p = 0.022). Adjusted for age, sex, race, and ethnicity, uveitis patients spent a significantly longer time (mean 27.5 min) compared to comprehensive ophthalmology patients (mean 25.5 min) with their physician (p = 0.0041). Among the uveitis patient population, African American patients (p = 0.0053), Hispanic or Latino (p = 0.034), and Medicaid (p = 0.035) patients had increased office visit times.
Conclusions
Those with uveitis spent more time with the physician than comprehensive patients. Race, ethnicity, payor type, and the major reason for the visit all significantly impacted uveitis office visit times. In order to manage their schedules, providers should be aware of the additional support and time needed by these patients during office visits.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data supporting the conclusions of this article is publicly available in the National Ambulatory Medical Care Survey repository, https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm.
References
Rothova A. Corticosteroids in uveitis. Ophthalmol Clin North Am. 2002;15:389–94.
Doycheva D, Deuter C, Grajewski R. Topical corticosteroids and non-steroidal anti-inflammatory drugs in the therapy of non-infectious uveitis. Klin Monbl Augenheilkd. 2018;235:586–91.
Ballenger LR, Ardoin SP, Driest KD. Assessing barriers to uveitis screening in patients with juvenile idiopathic arthritis through semi-structured interviews. Pediatr Qual Saf. 2018;3:e084.
Mueller CM, Ward L, O’Keefe GAD. Health literacy, medication adherence, and quality of life in patients with uveitis. Ocul Immunol Inflamm. 2022:30;1060–67.
Chu DS, Johnson SJ, Mallya UG, Davis MR, Sorg RA, Duh MS. Healthcare costs and utilization for privately insured patients treated for non-infectious uveitis in the USA. J Ophthalmic Inflamm Infect. 2013;3:64.
Scott AT, Pecen PE, Palestine AG. Ophthalmic medication price variation across the United States: anti-inflammatory medications. Ther Adv Ophthalmol. 2019;11:2515841419863638.
Briesacher BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: a review of the literature. J Gen Intern Med. 2007;22:864–71.
Cimino L, Neri P, Miserocchi E, Paroli MP, Vannozzi L, Mastropasqua L, et al. Non-infectious uveitis burden on quality of life and work impairment assessed through different psychometric questionnaires. Eur J Ophthalmol. 2022;32:2282–90.
Chauhan K, Scaife S, Rosenbaum JT. Uveitis and health disparities: results from the National Inpatient Sample. Br J Ophthalmol. 2019;103:1301–5.
Oh BL, Lee JS, Lee EY, Lee HY, Yu HG. Incidence and risk factors for blindness in uveitis: a nationwide cohort study from 2002 to 2013. Ocul Immunol Inflamm. 2021;29:1040–4.
Gilchrist VJ, Stange KC, Flocke SA, McCord G, Bourguet CC. A comparison of the National Ambulatory Medical Care Survey (NAMCS) measurement approach with direct observation of outpatient visits. Med Care. 2004;42:276–80.
Thorne JE, Skup M, Tundia N, Macaulay D, Revol C, Chao J, et al. Direct and indirect resource use, healthcare costs and work force absence in patients with non-infectious intermediate, posterior or panuveitis. Acta Ophthalmol. 2016;94:e331–9.
Shirahama S, Kaburaki T, Nakahara H, Tanaka R, Takamoto M, Fujino Y, et al. Epidemiology of uveitis (2013–2015) and changes in the patterns of uveitis (2004–2015) in the central Tokyo area: a retrospective study. BMC Ophthalmol. 2018;18:189.
González MM, Solano MM, Porco TC, Oldenburg CE, Acharya NR, Lin SC, et al. Epidemiology of uveitis in a US population-based study. J Ophthalmic Inflamm Infect. 2018;8:6.
Becker NV, Scott JW, Moniz MH, Carlton EF, Ayanian JZ. Association of chronic disease with patient financial outcomes among commercially insured adults. JAMA Intern Med. 2022;182:1044–51.
Miserocchi E, Modorati G, Mosconi P, Colucci A, Bandello F. Quality of life in patients with uveitis on chronic systemic immunosuppressive treatment. Ocul Immunol Inflamm. 2010;18:297–304.
Hribar MR, Huang AE, Goldstein IH, Reznick LG, Kuo A, Loh AR, et al. Data-driven scheduling for improving patient efficiency in ophthalmology clinics. Ophthalmology. 2019;126:347–54.
Gaffney A, Himmelstein DU, Dickman S, McCormick D, Cai C, Woolhandler S. Trends and disparities in the distribution of outpatient physicians’ annual face time with patients, 1979–2018. J Gen Intern Med. 2023;38:434–41.
Hsiang WR, Lukasiewicz A, Gentry M, Kim CY, Leslie MP, Pelker R, et al. Medicaid patients have greater difficulty scheduling health care appointments compared with private insurance patients: a meta-analysis. Inquiry. 2019;56:46958019838118.
Oliver MN, Goodwin MA, Gotler RS, Gregory PM, Stange KC. Time use in clinical encounters: are African-American patients treated differently? J Natl Med Assoc. 2001;93:380–5.
Allamby C, Scott T, Krizo J, Consing K, Mangira C, Simon EL. Do racial disparities exist at various time points during an emergency department visit for chest pain. Am J Emerg Med. 2022;58:1–4.
Tsui E, Crowell EL, Gangaputra S, Moussa K, Shantha JG, Shusko AJ, et al. Current landscape of uveitis specialists in the United States. J Acad Ophthalmol (2017). 2022;14:e187–92.
Acknowledgements
Thanks to Nicolas Gasquet (Wilmer Biostatistics Center) for helping with the statistical analysis.
Author information
Authors and Affiliations
Contributions
RM assisted with study design, compiled the data, and manuscript writing. MB assisted in study design, data analysis, and manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marshall, R.F., Berkenstock, M. Factors influencing treatment and time spent with physicians in patients with uveitis compared to other ophthalmology subspecialties in the National Ambulatory Medical Care Survey. Eye (2024). https://doi.org/10.1038/s41433-024-03071-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41433-024-03071-8