Abstract
Infectious diseases affecting the eye often cause unilateral or asymmetric visual loss in children and people of working age. This group of conditions includes viral, bacterial, fungal and parasitic diseases, both common and rare presentations which, in aggregate, may account for a significant portion of the global visual burden. Diagnosis is frequently challenging even in specialist centres, and many disease presentations are highly regional. In an age of globalisation, an understanding of the various modes of transmission and the geographic distribution of infections can be instructive to clinicians. The impact of eye infections on global disability is currently not sufficiently captured in global prevalence studies on visual impairment and blindness, which focus on bilateral disease in the over-50s. Moreover, in many cases it is hard to differentiate between infectious and immune-mediated diseases. Since infectious eye diseases can be preventable and frequently affect younger people, we argue that in future prevalence studies they should be considered as a separate category, including estimates of disability-adjusted life years (DALY) as a measure of overall disease burden. Numbers of ocular infections are uniquely affected by outbreaks as well as endemic transmission, and their control frequently relies on collaborative partnerships that go well beyond the remit of ophthalmology, encompassing domains as various as vaccination, antibiotic development, individual healthcare, vector control, mass drug administration, food supplementation, environmental and food hygiene, epidemiological mapping, and many more. Moreover, the anticipated impacts of global warming, conflict, food poverty, urbanisation and environmental degradation are likely to magnify their importance. While remote telemedicine can be a useful aide in the diagnosis of these conditions in resource-poor areas, enhanced global reporting networks and artificial intelligence systems may ultimately be required for disease surveillance and monitoring.
摘要
眼部传染病通常会导致儿童和工作年龄人群的单侧或不对称视力丧失。这类疾病包括病毒性、细菌性、真菌性和寄生虫性疾病, 既有常见病, 也有罕见病, 总体来说, 这些疾病占全球视觉负担的一大部分。即使是在眼科专科诊疗中心, 诊断也常具挑战性, 而且许多疾病的表现具有高度区域性。在全球化时代, 了解各种疾病的传播方式和感染的地理分布对临床医生具有指导意义。目前, 在全球视力障碍和失明发病率的研究中, 眼部感染性疾病的影响未能得到很好的体现, 可能这些研究侧重于50 岁以上人群的双眼性疾病。此外, 在许多情况下很难区分传染性疾病和免疫性疾病的区别。由于传染性眼病可预防, 且常影响年轻人, 我们认为在未来的流行病学研究中, 应将其视为一个独立的类别, 包括将预估残疾调整寿命年数 (DALY) 作为衡量总体疾病负担的标准。眼部感染的例数受到疾病爆发和地方性传播的独特影响, 其控制往往依赖于相关的领域, 这远远超出眼科范围, 包括疫苗接种、抗生素发展、个人医保、病媒控制、大规模药物管控、食品供应, 环境和食品卫生、流行病学地图等多个领域。此外, 全球变暖、冲突、粮食匮乏、城市化和环境退化等预期影响可能会增加其重要性。虽然远程医疗可以在资源匮乏地区在这些疾病的诊断方面提供有效辅助, 但疾病监测最终可能需要强化的全球报告网络和人工智能系统来完成。
Similar content being viewed by others
Introduction
The eye is susceptible to infections caused by a bewildering spectrum of organisms, from prions [1] to arthropods [2] (Table 1). Pathology may be restricted to the ocular tissues, or manifest in the eye as part of a systemic infectious disease, with impact ranging from minor nuisance to sight impairment or death [3]. While any structure along the visual pathways may be the focus of an infection, these disease presentations principally fall into one of three distinct anatomical categories: external eye, intraocular structures including the optic nerve, and ocular adnexae, although all three may be involved simultaneously. Many of these infections occur universally, whereas others occur only within certain geographic parameters such as the tropical belt, and seldom surface in temperate countries. A few, like cysticercosis and soil-transmitted helminthiases, are categorised as neglected tropical diseases [4].
As global warming progresses, however, geographic boundaries may shift [5]. In addition, widespread international travel and migration makes geographic boundaries porous, with the result that clinical presentations more commonly associated with tropical climes can present and must be recognised worldwide [6]. Infectious diseases that can manifest in the eye such as tuberculosis (TB) and measles tend to occur disproportionately among persons from developing countries with incomplete healthcare coverage and among migrants from these countries [7]. Moreover, emerging infectious diseases (EID) including arthropod-borne viral (arboviral) infections (e.g., Zika virus) and diseases of presumed zoonotic origin (e.g., Ebolavirus) have given rise to unexpected ocular pathologies [8,9,10]. While recognition thereof can be life-saving or life-changing, a failure to understand its implications can lead to inappropriate immunosuppression, with devastating consequences. It therefore behoves ophthalmologists everywhere to have a working knowledge of the vast spectrum of infectious diseases that can affect the eye.
Correct diagnosis is the critical first step in directing patients towards appropriate healthcare services for sight- or life-preserving treatment, reducing transmission, or even reporting an outbreak [11]. Once an infectious entity is suspected, a specific history guided by clinical and epidemiological risk factors should be elicited to determine possible relevant routes of potential exposure, and appropriate investigations requested to aid consultation and further care. Specialist investigations and multidisciplinary management may be necessary but are often not possible in low-and middle-income countries, which bear the brunt of global visual impairment [12]. Whereas ophthalmologists in rich countries benefit from a plethora of aids to diagnose infectious disease, such as DNA analysis of ocular samples and CT-PET scans to identify avid lymph nodes, medical staff in resource-poor settings may be guided only by clinical acumen and epidemiological knowledge [13]. The challenges are substantial, and although they are being addressed through innovative public health initiatives, much work remains to be done at a grassroots level [14].
From an epidemiological perspective, infectious diseases trail far behind the main global causes of avoidable moderate-to-severe distance visual impairment (MSVI) and avoidable blindness, estimated in a large meta-analysis to affect 553 million and 43 million people, respectively in 2020 [15]. Due to lack of sufficient data, the meta-analysis is based on population-based surveys of eye disease in people aged 50 and above, and the definition of sight impairment stipulates a visual acuity threshold for the better-seeing eye, thus neglecting the burden of conditions affecting only one eye [16]. Important infectious entities causing bilateral visual impairment remain trachoma and onchocerciasis, yet both are in sharp decline and anticipated to be under control by 2030 [12]. Moreover, both diseases are located in geographical pockets of high risk, in contrast to infectious eye diseases with a more global distribution, such as herpes and syphilis. While this underscores a shift in visual burden towards non-communicable diseases, the true global visual burden of infectious diseases is most likely underestimated for several possible reasons. Most significantly, infectious eye conditions are often unilateral, and are therefore not captured in prevalence studies using commonly adopted definitions of sight impairment. Monocular visual impairment is now officially recognised as a disability by WHO [17], and is much more common than bilateral visual impairment [18]. Moreover, in contrast to sight-threatening conditions acquired in maturity, many infectious eye diseases are likely to be evenly distributed across all age groups, and epidemiological or population-based studies focusing on the over-50s may underestimate both their statistical significance and economic impact. For example, studies from low vision services in Latin America indicate toxoplasmosis as one of the leading causes of childhood blindness, yet this valid source of information is not currently incorporated into global estimates. Since toxoplasmosis is common and globally distributed, its toll on vision may be significantly underestimated (especially in terms of years of vision loss), possibly even vying with trachoma and onchocerciasis as a leading infectious cause of sight impairment and blindness worldwide. Determining the true global visual burden of ocular toxoplasmosis will be a sizeable challenge.
There are several other reasons for this suggested attribution bias as the following examples demonstrate. In many parts of the world where ocular infections are common, ophthalmic services in aggregate are often underdeveloped or absent altogether, and diagnoses may easily be missed or simply unreported [13]. Ocular infections can cause secondary pathologies, such as cataract, glaucoma, or retinal detachment, to which sight loss might be attributed without recognition of the underlying cause [19]. Common medications used to treat ocular infections, such as ethambutol and linezolid, may themselves cause visual loss [20]. Para- or post-infectious syndromes may not be identified and assumed to be auto-immune non-infectious presentations. The role of immune-mediated pathology following infections is complex and incompletely understood [21]. The global visual burden of EIDs such as dengue fever, Ebolavirus disease and coronavirus disease remains poorly understood [8, 22, 23]. Estimating the global visual burden of infectious disease is, therefore, likely to be an extremely complex undertaking.
Although data are currently sparse, it is likely that if one were to combine in one category all unilateral and bilateral visual loss due to infectious causes of keratitis [24], optic neuritis [25], uveitis [26] and orbital cellulitis [27], infectious disease would feature more prominently as a cause of the global visual burden. Progress has been achieved across multiple domains in reducing the burden of trachoma, cytomegalovirus retinitis, and onchocerciasis [13], suggesting that sight impairment from other infectious causes should be similarly preventable by collaboration between various disciplines. In this respect, infectious causes of eye disease stand out from other sight-threatening conditions, and in future prevalence studies, it would therefore be useful to consider them in aggregate.
Viral ophthalmic diseases
Many viruses cause ophthalmic disease, including adenovirus, influenza A, SARS-CoV-2, herpesviruses, HIV, measles, arthropod-borne viruses (arboviruses), zoonotic viruses, and others [23, 28]. The herpesviruses and adenoviruses possess double-stranded DNA, whereas the bulk of the remainder of viruses affecting the eye (flaviviruses, influenza, measles, filoviruses, and others) are enveloped single-stranded RNA viruses [29]. Certain RNA viruses, suggested to be inherently more mutation-prone, have been implicated in EIDs and may prove to be causative pathogens of future pandemics [8, 23, 30].
While adenovirus, influenza, and coronavirus infections typically pass without lingering effects, they occasionally have sight-threatening sequelae such as corneal scarring [31], acute posterior multifocal placoid pigment epitheliopathy [32], and retinal vascular occlusion [33], respectively. These complications may be rare, but as infections with these viruses are common, their visual burden around the world may be significant. While vaccination might be expected to mitigate visual loss from these and other viruses, vaccines themselves can precipitate ocular complications leading to visual loss [34].
The herpesviruses cause a range of pathologies, from self-limiting dendritic corneal ulcers to bilateral acute retinal necrosis (ARN), leading to visual impairment, and even complete blindness globally [35,36,37,38]. This group includes varicella zoster and herpes simplex type 1, the most common causative agents of ARN in adults, and herpes simplex type 2, an important cause of ARN in children following neonatal exposure [39]. These are common pathogens with a worldwide distribution, serological exposure increasing with age [40]. It has been calculated that, in 2016, 230,000 people around the world suffered uniocular visual impairment because of newly diagnosed HSV keratitis [35]. Infection with these viruses can lead to disseminated multisystem disease with florid ocular involvement, in some cases leading to death, especially in the context of immunodeficiency, immunosuppression, or immunosenescence [41]. While there may be a role for recombinant vaccines in preventing ocular complications and visual loss from varicella zoster infections [42], there have been numerous case reports of ARN and other manifestations of herpetic infection following vaccination [22]. Vaccines are under development for HSV-2 infection which is thought to increase the risk of acquiring HIV [43].
In the same family, cytomegalovirus (CMV) has emerged as a common cause of hypertensive anterior uveitis [44], and also causes a characteristic retinitis in immunodeficient individuals, leading to a substantial visual burden especially in poor countries [37]. These infections are treatable with a combination of anti-viral drugs, corticosteroids, and anti-glaucoma medications. Screening and treatment programmes by HIV physicians have been effective in some areas [45]. In addition, congenital CMV infection is associated with ophthalmological disorders including retinochoroiditis and visual impairment in a proportion of cases [46]. While the possible role of Epstein-Barr virus in causing retinal disease is controversial, as it can often be detected in non-infectious uveitis, it is strongly associated with nasopharyngeal cancer and lymphomas that can invade ocular tissues [47, 48]. Similarly, human herpesvirus-8 is associated with Kaposi sarcoma, which occasionally involves the conjunctiva and/or the eyelid [49].
Although HIV causes retinopathy and anterior uveitis in its own right [50], the bulk of ocular damage in HIV disease is from opportunistic infections such as cytomegalovirus, varicella zoster, Cryptococcus neoformans, Pneumocystis jirovecii, human herpesvirus 8, microsporidia, Toxoplasma gondii, and others, as well as infection-induced neoplasia [37, 51,52,53,54]. In addition, visual loss may occur as a result of immune recovery inflammatory syndromes following treatment of HIV with modern combination anti-retroviral therapy, including immune recovery uveitis [55] and paradoxical worsening of TB [56]. Visual loss may also occur because of drug-induced uveitis, most commonly with cidofovir or rifabutin [57]. While recent diagnostic and therapeutic developments have allowed many people with HIV to enjoy an apparently normal life expectancy, health inequalities dictate that in several parts of the world, coverage is still incomplete. Consequently, ophthalmic complications of HIV disease persist, producing visual impairment in an unknown proportion of the approximately 40 million people living with HIV worldwide, probably more so in poor countries without screening programmes for CMV retinitis [13]. As the new brands of anti-retroviral medications become more available across the globe, we can expect this proportion to fall.
Another retrovirus, human T lymphotropic virus type 1 is one of the most common causes of retinal vasculitis and vitritis in endemic areas such as Japan, frequently leading to visual loss [58].
Worldwide, the measles virus has been one of the most common causes of blindness in childhood in at-risk populations [59]. This occurs because infection can cause a precipitous loss of vitamin A to which children with already low reserves are especially vulnerable [60]. The acute vitamin A deficiency leads to a progressive spectrum of ocular pathology, termed xerophthalmia, from night blindness and severe ocular surface dryness (xerosis) to corneal ulceration, keratomalacia, and corneal scarring, along with permanent retinal structural changes. Cell-mediated immunity also is compromised, making the cornea susceptible to secondary infection and necrosis. In addition to exacerbating hypovitaminosis A, the measles virus can directly cause keratitis, retinitis and optic neuritis. The mainstay of prevention in malnourished populations is measles vaccination, together with vitamin A supplementation given at the time of vaccination, as well as in fortified food. While vitamin A deficiency worldwide has been decreasing worldwide [61], the impact of food poverty due to conflict and global warming may be significant this century. In addition, measles vaccination rates have been hit by misinformation campaigns, with unclear consequences for future measles epidemics [62].
Despite the development of an effective vaccine against the rubella virus over half a century ago, congenital rubella syndrome persists as a disease with devastating ocular consequences [63] in a few countries where vaccine uptake remains low [64]. Pregnant women infected with rubella in the first trimester are most at risk of transmitting the virus to the foetus, resulting in congenital ocular manifestations such as cataract, microphthalmos and pigmentary retinopathy [65]. More recently, an association has emerged between rubella and Fuchs uveitis syndrome, evidenced by the finding of an excess of rubella antibodies compared to serum levels, as well as the rubella genome, in the aqueous humour of eyes with clinically defined Fuchs uveitis syndrome [66]. A decrease in this syndrome has been reported in the United States following the introduction of the rubella vaccination programme in 1969 [67].
Dengue is the most common arbovirus worldwide, infecting up to 400 million people every year following the bite of Aedes spp. mosquitoes [68], mainly in urban centres in the tropical belt. These vectors proliferate during wet seasons, driving dengue epidemics. The number of cases of dengue has been increasing year after year, principally due to global warming favouring the expansion of the habitat of its mosquito vectors [69]. Typically, primary infection with one of the four viral serotypes is mild. A second infection with a different serotype, however, can produce a more severe clinical picture including haemorrhage and death, which has been attributed to antibody-dependent enhancement [70]. This mechanism is a potential obstacle to the development of a dengue vaccine. A small proportion of infected persons will have some degree of ocular involvement, from a self-limiting multifocal retinitis and vitritis to a posterior pole ischaemic retinal vasculitis and foveolitis, with outcomes ranging from a transient disturbance to permanent central blindness [71, 72]. In one outbreak of dengue serotype 1, the prevalence of maculopathy was reported to be 10% [73]. The risk factors leading to ocular complications are unknown [74], but it seems plausible that severe ocular involvement may be more likely following secondary infection. As the development of an effective vaccine has so far proven elusive [75], efforts at containing dengue have focused on limiting the ability of the mosquito vector to transmit the virus, for example by infecting mosquitoes with a ubiquitous endosymbiotic bacterium, Wolbachia spp. [76].
Another of the viruses transmitted by Aedes mosquitoes, the chikungunya virus has a similar environmental suitability map to dengue [77] but differs from dengue in that it has an additional sylvatic life cycle involving non-human primates. Chikungunya infection is typically self-limiting but can be associated with ocular findings causing visual loss, such as intraocular inflammation, multifocal retinitis and optic neuritis [78]. Far less common than dengue, the closely related Zika virus is also transmitted by Aedes spp., and its sight-threatening complications include uveitis and congenital malformations of the eye [79]. Zika virus infection causes anterior uveitis in acquired disease, and macular lesions in congenital disease. In contrast, West Nile virus is transmitted to humans from infected birds by Culex spp. mosquitoes. Infection produces a characteristically linear chorioretinitis [80]. In each case, the expansion of the mosquito vector habitat will determine the geographic spread of the infection, while climatic events such as precipitous rainfall and flooding may be a significant factor in driving future vector-borne epidemics [81].
Outbreaks of Rift Valley fever typically occur in Africa and the Middle East during periods of high rainfall leading to a massive increase in the proliferation of Aedes and Culex vectors, which then transmit the virus from livestock to man in high numbers [82]. In a small proportion of cases (estimated at around 1 to 2%), infection with RVF virus causes a characteristic macular retinitis, which is frequently bilateral and can lead to central blindness [83].
Recent outbreaks of presumed zoonotic viruses that predominantly spread directly from person to person, such as Ebolavirus (thought to be initially transmitted to humans by fruit bats) [9] and SARS-CoV-2 (zoonotic origins disputed) [10], have also been associated with ocular morbidity. In the case of Ebola, the filovirus can survive in the eye for several months after infection (similar to Marburg), eliciting a spectrum of signs from mild chorioretinal scarring to severe panuveitis in a high percentage of survivors, many of whom had secondary complications such as cataract, glaucoma and retinal detachment [84, 85].
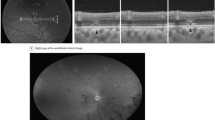
Infection with SARS-CoV-2, on the other hand, may precipitate a hypercoagulable state indirectly resulting in retinal arterial and venous occlusions, as well capillary ischaemia possibly linked to paracentral acute middle maculopathy and acute macular neuroretinopathy [33]. Vaccination is now a key strategy to limit the morbidity of these viruses, although vaccines themselves have been reported to be associated with ocular pathologies similar to those found following SARS-CoV-2 infection [33, 86]. Proving causality, however, remains challenging.
Numerous other viruses have been reported to cause ocular pathology and visual loss, such as Coxsackie virus [87], a putative cause of unilateral acute idiopathic maculopathy. The role of viral illness in presumed post-infectious ophthalmological entities such as multiple evanescent white dot syndrome remains incompletely understood [88, 89]. While many patients recover vision spontaneously following post-infectious syndromes, a minority of patients lose vision permanently.
Bacteria and fungi
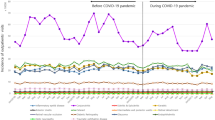
The global visual burden of trachoma, caused by repeated conjunctival infections with serological variants of the obligate intracellular bacterium Chlamydia trachomatis has been well documented [90, 91]. The Musca sorbens fly, which feeds on human mucosal secretions and preferentially lays its eggs in human faeces, is thought to act as a mechanical vector for the bacterium in endemic areas, especially in areas where sanitation is poor and open defecation is practiced [92]. Repeated infections (around 150 to 200) cause progressive tarsal conjunctival scarring, leading to entropion and trichiasis, which in turn scars the corneas leading to sight loss, typically in middle age. According to WHO, trachoma is currently responsible for the blindness or visual impairment of about 1.9 million people in 42 countries, and about 1.4% of all blindness worldwide at an annual cost of 2.9 to 5.3 billion US dollars. The visual burden, shouldered mostly in sub-Saharan Africa, had been decreasing every year [93] until the worldwide SARS-CoV-2 pandemic of 2020 when progress was briefly disrupted. Key to this progress is the SAFE strategy, a treatment and prevention programme adopted by WHO in 1993. The strategy prioritises Surgical procedures, including epilation and posterior lamellar tarsal rotation for trichiasis and cicatricial entropion, respectively [94], mostly carried out by trained nurses, Antibiotic treatment (e.g., oral azithromycin), awareness of hygiene measures such as Face washing, and Environmental improvements including closed latrines and clean water sources [95]. While it has not been possible to eliminate the disease as a public health problem thus far, the WHO Alliance for the Global Elimination of Trachoma by 2020 now aspires to eliminate it by 2030 [12, 96]. If this is achieved, it will represent the culmination of a vast combined effort by various international, governmental and non-governmental partners to carry out epidemiological surveillance, evaluate projects and mobilise resources, and could provide a template for limiting preventable visual impairment due to other less common infectious causes, for example by promoting reporting of relevant data on infectious eye disease to WHO.
Several sight-threatening ocular pathologies, including infectious keratitis, orbital cellulitis and endophthalmitis are caused by a wide variety of different pathogens, including bacteria, fungi, protists and viruses; co-infection is also possible. Many of the causative pathogens are universal, whereas others exhibit considerable variation in geographic distribution [97]. In the tropics, these conditions may be caused by organisms unfamiliar to ophthalmologists in temperate countries. As an example, Burkholderia pseudomallei, a Gram-negative bacillus acquired through direct contact with contaminated soil and water, is a known cause of infectious keratitis, endophthalmitis and orbital cellulitis in Thailand [98], yet its geographical distribution outside southeast Asia and northern Australia remains poorly understood [99].
Infectious keratitis, commonly called corneal ulceration, is one of the leading global causes of unilateral blindness; it has been described as a ‘silent epidemic’ [100]. The visual burden of infectious keratitis in resource-poor settings greatly exceeds that in rich countries, prompting a proposal to designate this condition as a neglected tropical disease [101]. Common pathogenic causes worldwide include coagulase-negative staphylococci, Streptococcus pneumoniae, Pseudomonas aeruginosa, Staphylococcus spp., herpes simplex and zoster, Fusarium spp., Aspergillus spp., Microsporidia, Candida spp. and Acanthamoeba spp., and rarer causes include non-tubercular mycobacteria and Nocardia spp., as well as a plethora of other organisms [24]. Risk factors include hypoxia-inducing contact lens wear, while agricultural and other ocular trauma is a more common predisposing factor in resource-poor countries. In a proportion of cases, it is bilateral, notably in neonatal conjunctivitis where the causative pathogen may be Neisseria gonorrhoeae, which can lead to blindness rapidly and may be resistant to antibiotics [102]. More broadly, the prevalence of multidrug-resistant bacterial keratitis may be increasing [103]. The true burden of infectious keratitis is unknown, in part because epidemiological studies lack the data to disaggregate it from other non-infectious causes of non-trachomatous corneal opacity, estimated to cause 3.2% of global blindness [104]. In areas where bacterial, fungal and other pathogenic causes of infectious keratitis are common, it can be difficult to distinguish these clinically. There is no substitute for microbiological diagnosis, including Gram staining, culture and DNA analysis of tissue samples in identifying the causative pathogen to guide treatment [105]. Wherever this facility is lacking, however, empirical treatments with topical antibiotics and anti-fungals are sometimes the only option to treat infectious keratitis, leading to uncertain outcomes. The emergence of multidrug resistance, as well as the harm done by traditional medicines [106], contribute further to the toll of infectious visual loss. The role of antiseptics such as povidone-iodine in treating infectious keratitis has been evaluated, showing promise against Gram-positive organisms [107].
Orbital cellulitis remains a significant cause of visual morbidity as well as mortality worldwide, more frequently affecting children [108]. It commonly results from the spread of infection from the sinuses and periorbital skin, as well as haematogenous spread from distant sites. Infection may be polymicrobial, although streptococcal and staphylococcal species predominate. Aggressive treatment is typically required to prevent complications such as visual loss, including immediate empirical treatment with intravenous antibiotics and early surgery to drain sinuses and abscesses. This level of care is frequently unavailable in resource-poor settings. Vaccination against Haemophilus influenzae type B is one measure judged to have reduced rates of orbital cellulitis in children [27]. In poor countries, however, many children remain unvaccinated [109] and at risk of visual loss.
Invasive fungal causes of rhinosinusitis, often caused by Mucor and Aspergillus species, are a feature of immunodeficiency, uncontrolled diabetes mellitus and corticosteroid treatment, and saw a resurgence during the 2020 SARS-CoV-2 pandemic attributed to treatment of serious respiratory complications with corticosteroids, notably in South Asia [110].
Infectious endophthalmitis remains a serious possible complication of all penetrating eye injuries and intraocular procedures [111], but it may also arise spontaneously, rarely in otherwise completely asymptomatic individuals, as well as those with serious systemic infections, following haematogenous spread of bacterial, fungal and other pathogens [112]. As a matter of convention, viral and parasitic causes of endogenous infection are usually considered separately as uveitic entities [113]. The list of organisms reported to cause endophthalmitis is long, but commensal coagulase-negative Staphylococcus spp. were found to predominate (39.4%) in one large series of culture-positive isolates from a single institution in North America, followed by Streptococcus viridans (12.1%) and Staphylococcus aureus (11.1%) [114]. Gram-negative organisms and fungi accounted for 10.3% and 4.6% of isolates, respectively. More indolent causes of endophthalmitis, typically with a delayed presentation, include Cutibacterium acnes [115]. Regional differences in the percentages of different causative pathogens exist, as exemplified by endogenous Klebsiella pneumoniae endophthalmitis secondary to pyogenic liver abscess, often reported to be more prevalent in east Asian countries but which is emerging in several countries around the world [116]. In rich countries, postoperative endophthalmitis is well recognised as a serious complication, and is typically managed as a medical emergency with intravitreal and systemic antibiotics and vitrectomy, with mixed results reflecting the virulence of the causative organism and the timing of presentation. In many resource-poor settings, however, the circumstances surrounding presentations of endophthalmitis may be very different, often leading to poor visual outcomes and impacting on patients’ economic potential [117]. As cataract surgical rates increase around the world, and with the emergence of intravitreal therapies, the incidence of endophthalmitis can be expected to rise concomitantly.
Endogenous fungal endophthalmitis is associated with distinct medical risk factors, including diabetes mellitus, immunosuppression, dialysis and intravenous drug use [118]. Lemon juice used to dissolve opiates and stimulants has long been identified as a source of Candida spp. in cases of endophthalmitis among intravenous drug users [119].
Mycobacterial diseases, chief among which is tuberculosis, impose a significant burden on vision worldwide, especially in endemic areas but also in some countries with low endemicity [120]. Approximately 10.6 million people around the world fell ill with TB in 2021 [121], yet significant gaps in our knowledge concerning the global visual burden of ocular TB remain. In part, this is because ocular TB is itself often a challenging concept for ophthalmologists and TB physicians alike [122]. The diagnosis can be straightforward, for example when a choroidal granuloma is found in a patient from an endemic area, and a chest X-ray showing characteristic changes together with a positive immunological test corroborate the ocular findings. At the other end of the scale are clinical presentations that suggest but do not establish beyond doubt a diagnosis of ocular TB, such as occlusive retinal vasculitis, ampiginous, serpiginous-like and multifocal choroiditis, as well as chronic granulomatous uveitis [123]. To complicate matters, radiological and immunological tests (e.g., tuberculin skin test or interferon-gamma release assay, which do not distinguish between active and latent TB) may be negative even in culture-confirmed TB [124]. The Collaborative Ocular Tuberculosis Study group has recently devised a consensus-based decision-making tool enabling users to confidently recommend starting ATT [125]. Once treatment is started, the clinical picture may initially deteriorate due to increasing inflammation, a phenomenon known as paradoxical worsening [126]. The emergence of multidrug-resistant strains of TB further complicates progress, although new drug regimens have recently been found to be non-inferior to standard treatments [127]. The global prevalence of visual impairment secondary to ocular TB, therefore, is a complex question likely to tax even the most assiduous epidemiological researcher.
While it is much less common than TB, leprosy (Mycobacterium leprae) also can cause visual impairment, mostly due to neurotrophic keratitis and lagophthalmos secondary to cranial nerve inflammation or bacillary invasion, but also due to direct bacillary invasion of intraocular structures [128]. Following systemic treatment for multibacillary (lepromatous) leprosy, it is possible for bacilli to persist inside the eye, eliciting a severe inflammatory response leading to visual impairment and blindness [129]. A biopsy of iris granulomas (leproma) in patients with chronic uveitis treated for leprosy may occasionally demonstrate viable mycobacteria, indicating a need for further treatment rather than immunosuppressive therapy alone [130]. It is unclear whether these organisms can survive in the eye because of treatment failure, suppressed cell-mediated immunity [131] or possibly anterior chamber-associated immune deviation.
Non-tubercular mycobacteria (e.g., Mycobacterium abscessus) have been implicated in severe ocular infections, such as necrotising sclerokeratitis resulting in enucleation [132]. Diagnosis may be delayed, even with tissue biopsies sent for histopathological analysis, as the bacilli can be mistaken for Corynebacteria or Nocardia spp. on microscopy.
Spirochaetes represent another group of bacteria of great ophthalmological importance, including syphilis, leptospirosis and Lyme disease all of which can have a significant impact on the eyes [133]. Less well known are the tick-borne relapsing fevers, endemic in many tropical and temperate regions and also able to cause ocular inflammation [134].
In the past two decades, there has been a resurgence of syphilis in other high-income countries, linked in part to the success of both treatment and pre-exposure prophylaxis against HIV [135]. This can be associated with a reduction in the use of condoms during high-risk sexual activity, resulting in an increase in other sexually transmitted infections [136]. Ocular syphilis, caused by infection with Treponema pallidum, can manifest in various forms, including chronic granulomatous or non-granulomatous anterior uveitis, retinitis, optic neuritis and a characteristic placoid chorioretinitis from a few weeks to several months after primary infection [137, 138]. It is assumed that following infection, treponemes can invade the ocular tissues, including the retina which is part of the central nervous system, and ocular syphilis is therefore considered to be a manifestation of neurosyphilis. Signs of secondary syphilis, such as palmar and plantar rashes, may be present, although ocular syphilis may feature at any stage of the disease. The ocular signs may be subtle and can be missed [139], often leading to counterproductive treatment with systemic corticosteroids. In congenital cases, Hutchison’s triad consisting of interstitial keratitis, malformed teeth and eighth nerve deafness may be present. Serological testing is an essential aspect of diagnosis. False positive treponemal serology tests are possible in cases of endemic treponemal infections such as yaws, bejel and pinta, whereas non-specific serological tests may be positive in certain non-syphilitic conditions [140]. Once positive, treponemal serology does not revert, whereas non-specific assays can be used to monitor treatment success, defined as a fourfold decrease in titre (e.g., from 1:1024 to 1:256). Ocular syphilis must be managed in collaboration with colleagues in sexual medicine, following neurosyphilis treatment protocols [137, 138]. While some visual recovery is possible following treatment, visual impairment can be permanent if the diagnosis is delayed, yet the global visual burden remains unknown.
In recent decades, infections with Leptospira spp., one of the world’s most common zoonoses [141], have emerged as a major cause of ocular inflammation and visual impairment, predominantly in tropical zones [142]. It may occur months or even years after primary infection following contact with contaminated water during an epidemic, often presenting with non-granulomatous hypopyon uveitis, although a multitude of ophthalmic signs such as retinal vasculitis and vitritis are recognised associations [143]. Visual prognosis is usually good, but secondary complications such as cataract are common [144]. Although leptospirosis is common worldwide, it is rarely considered - let alone tested for - in the Global North, except perhaps in moderately high prevalence areas like Hawaii. Outbreaks are related to sanitation and are therefore difficult to prevent in many parts of the resource-poor world [145].
Tick-borne borrelioses include Lyme disease and tick-borne relapsing fevers [140], both of which cause inflammatory eye diseases [146]. Lyme disease is prevalent in areas where humans encounter deer infected with B. burgdorferi in the United States and B. afzelii or B. garinii in Europe. Lyme disease is a well-recognised cause of intermediate, posterior and panuveitis, including retinal vasculitis, serous retinal detachment and papilloedema, with late manifestations including peripheral ulcerative keratitis. Tick-borne relapsing fevers are caused by locally endemic Borrelia spp. in central Asia, East Africa, the Mediterranean and the Americas. They are rarely considered as causes of uveitis outside these endemic areas, and their burden is unknown.
The tick-borne diseases also include rickettsioses such as the spotted fever group [147]. Mediterranean spotted fever (also known as boutonneuse), caused by Rickettsia conorii and transmitted by canine ticks, is prevalent in the Mediterranean basin, the Middle East, central and southern Asia, and sub-Saharan Africa. It can present with focal and multifocal inner retinitis, neuroretinitis and uveitis [148]. Typically, a black eschar is present on the skin indicating a tick bite, and there may be a history of a headache, fever and skin rash. It is one of the most commonly imported rickettsioses by returning international travellers [149].
Cat scratch disease, caused by Bartonella henselae, is transmitted directly to humans by cats through biting and scratching, as well as by tick and flea vectors [150], at least between cats. It is a well-known cause of multifocal retinal infiltrates, retinal artery occlusion and neuroretinitis, potentially leading to visual loss [151, 152]. The disease is thought to have a worldwide distribution, although its effects on visual loss in the tropics remain unknown.
Another common zoonosis in the tropical belt, Malta fever is caused by Brucella melitensis transmitted by unpasteurised dairy products and may be complicated by focal chorioretinitis and optic nerve swelling [153, 154]. Choroidal granulomas may be present, mimicking tuberculosis. In one series of 1551 patients, ocular involvement, most commonly posterior uveitis, was found in 0.7% of patients with acute brucellosis and in 7.9% of patients with chronic brucellosis, in some cases leading to blindness [155]. Prevention depends on quality control of dairy products and vaccination of livestock in endemic countries [156].
Post-streptococcal syndrome uveitis is an immune-mediated response following a group A β-haemolytic streptococcus pharyngeal infection, which may include bilateral sight threatening non-granulomatous panuveitis, mostly affecting children and teenagers in economically challenged communities [157]. Elevated anti-streptolysin O titres confirm a recent invasive streptococcal infection in these patients [158].
Community-acquired fungal infections rarely can spread to the eye, causing severe visual loss, even in immunocompetent individuals. Culprits include coccidioidomycosis [159] and paracoccidioidomycosis [160], inhaled as spores often in an agricultural setting in hyperendemic areas. In contrast, presumed ocular histoplasmosis is thought to be an immunological reaction following exposure to histoplasma in endemic areas [161], and is a significant cause of visual morbidity. Disseminated histoplasmosis and talaromycosis are more likely to features of profound immunodeficiency [162], while sporotrichosis endophthalmitis can occur because of traumatic inoculation [163].
Parasites and arthropods
Parasitic infections have a particularly strong association with the tropics, reflecting habitats and climates that favour parasite and vector survival as well as social and environmental conditions that permit human infection. The eye can host both protozoan organisms, which include amoebae, and helminthic parasites, and rarely it can become severely damaged by invasion by arthropods [2]. Some, but not all parasites that affect the eyes are important zoonoses [164].
Two protists, namely Acanthamoeba spp. and Toxoplasma gondii, cause widespread ophthalmic pathology. Acanthamoeba spp. are one of a group of ubiquitous free-living amoebae that occasionally cause fatal encephalitis in humans and are well known as a cause of painful infectious keratitis and scleritis associated with exposure to contaminated water and contaminated contact lens equipment [165, 166]. Acanthamoebal sclerokeratitis may be refractory to treatment and persist for several years, and trophozoites may occasionally invade the eye, leading to severe inflammation and blindness. The incidence is said to be increasing due to the global epidemic of myopia, which has resulted in increased contact lens use [167].
Toxoplasma gondii is one of the most common parasites in the world to infect humans and is a major cause of retinochoroiditis and visual loss [168]. It is a well-recognised cause of congenital blindness following primary maternal infection and transplacental spread [169]. It may be acquired in life following exposure to sporulated oocysts in cat faeces or contaminated soil and water, or to tissue cysts through ingestion of undercooked meat, blood transfusion and organ transplantation. Transmission is more common in warm, humid climates germane to the sporulation and prolonged survival of oocysts in the soil. Additional risk factors include the presence of oocysts in drinking water [170], and social factors such as acceptability of eating raw meat [171]. Primary infection may lead to a florid retinochoroiditis and vitritis, especially in immunodeficient and immunosenescent individuals [172], although severe systemic manifestations are possible even in immunocompetent travellers [173]. Typically, the inflammation subsides leaving behind retinal scars which become increasingly pigmented over time. Cysts are present adjacent to the scar, and recurrence of inflammation due to tachyzoite proliferation is not uncommon. In some instances, especially in the setting of immunodeficiency, toxoplasma retinochoroiditis can run an aggressive, protracted course leading to severe visual impairment. Disease acquired during pregnancy poses a serious risk to the unborn child and requires management by the obstetrician to prevent vertical transmission [174].
Post-kala azar ocular leishmaniasis is a protozoal parasitic ocular condition that is not widely known among Western ophthalmologists, but which may affect travellers returning from countries where endemic or sporadic visceral leishmaniasis occurs in the population [175]. Visceral leishmaniasis (kala azar) is caused by two species of Leishmania, L. donovani in east Africa and south Asia and L. infantum in South and Central America, the Middle East and the Mediterranean basin [176]. It is spread by the bite of a sandfly and where the domestic dog can act as reservoir host [177]. The parasite migrates to the spleen and bone marrow, causing hepatosplenomegaly and bone marrow suppression. Treatment directed at reducing the visceral parasitic load frequently causes the Leishmania amastigotes to migrate back towards peripheral tissues, including the eyes, where the subsequent intense chronic inflammation causes severe tissue damage and visual loss [178]. The conjunctivae and orbits may become swollen due to infiltration with amastigotes. Post-kala azar ocular leishmaniasis is to be distinguished from primary leishmania lesions on the eyelids causing chronic localised swelling and lymphadenopathy (analogous to Romaña’s sign in Chagas disease), which can also be a feature of cutaneous and mucocutaneous forms of leishmaniasis. Treatment of visceral leishmaniasis can be very lengthy and complex, and eradication may not be achieved [179]. Importantly, therefore, these patients should not be treated with secondary immunosuppressive therapeutic agents, such as biologic anti-TNF drugs, but with repeated cycles of anti-parasitic drugs.
Helminthic parasites include roundworms (nematodes), tapeworms (cestodes) and flukes (trematodes). While some helminth infections pose significant regional public health problems, most are individually rare, yet collectively, these constitute a global challenge to vision.
Onchocerciasis is stated to be the second most common infectious cause of visual impairment after trachoma, affecting approximately three-quarters of a million people [180]. The pathogenic cause is a filarial nematode worm, Onchocerca volvulus, transmitted by the bite of species of blackfly near fast-flowing rivers in hyperendemic areas, most of which are in western and central Africa with smaller foci in South America and Yemen. The adult worms form nodules (onchocercomas) over bony prominences, where the female worm produces around a thousand microfilarie each day. These infiltrate the skin, eliciting inflammation that provokes intense itching. Eventually, the microfilariae infiltrate the ocular tissues, causing a spectrum of disease that includes sclerokeratitis and endophthalmitis leading to atrophic degeneration of the uveal tissues and retina, optic nerve atrophy and secondary cataract [181], although there may be regional variation in the patterns seen. Like trachoma, onchocerciasis is decreasing as a global cause of visual loss because of public health measures including vector control and mass drug administration of ivermectin, freely donated by the manufacturer [182]. The severe itching is relieved for approximately one year by annual administration of ivermectin, which greatly facilitates uptake of the mass drug administration, in turn reducing the incidence of blindness very favourably.
A particular challenge with treatment arises in areas where onchocerciasis is co-endemic with infection with Loa loa, another filarial worm transmitted by the deerfly in equatorial forests. Ivermectin can precipitate a fatal encephalopathy in people with high microfilarial loads of L. loa, whereas diethyl carbamazine, used to treat Loaiasis, can trigger the Mazzotti reaction, a life and sight threatening allergic response, in people infected with O. volvulus [183]. To mitigate this, the ‘test-and-not-treat’ strategy has been adopted, whereby L. loa microfilarial loads are quantified, and if found to be high, treatment with ivermectin deferred [184]. In such cases, albendazole has been used to decrease the L. loa microfilaraemia [185], while doxycycline is thought to be effective against O. volvulus by targeting its endogenous symbiont, Wohlbachia spp. [186]. Loa loa, the African eye worm, is known for its frequently dramatic appearance in the subconjunctival space, but it does not commonly cause visual loss except in rare cases when it invades the intraocular space [187].
Ocular toxocariasis is another nematode infection, caused by accidental ingestion of the eggs of Toxocara spp. shed in the faeces of cats (T. cati) and dogs (T. canis), and it can be acquired worldwide [188]. The larvae hatch in the intestine, penetrate the intestinal wall and migrate haematogenously to the eye, termed ocular larva migrans, almost always in the absence of systemic disease [189]. Ocular toxocariasis is typically a unilateral condition, tending to present as a posterior pole granuloma, as a peripheral granuloma with fibrous bands to the posterior retina, or as a chronic endophthalmitis, frequently resulting in severe visual loss [190].
The clinical finding of a motile retinal worm on fundoscopy, in association with optic disc swelling and macular exudates, was originally attributed to ocular toxocariasis [191]. Originally described as diffuse unilateral subacute neuroretinitis, it is now understood occasionally to affect both eyes [192] and is perhaps more accurately termed diffuse subacute neuroretinitis (DSN) [193]. In the early stages, there may be mild central visual loss, and disc swelling, macular exudates and clusters of small white retinal lesions may be visible on fundoscopy. These lesions may progress to profound visual loss with optic atrophy and widespread degeneration of the retinal pigment epithelium. Following the observation that this condition also could be caused by an intestinal racoon nematode, Baylisascaris procyonis [194], many additional nematodes have been implicated, including soil-transmitted helminths, Strongyloides spp., food- or waterborne zoonotic helminths, arthropod-borne filarial worms and non-human hookworms [195].
Soil-transmitted helminth infections (Ascaris lumbricoides, hookworms Ancylostoma duodenale and Necator americanus, and Trichuris trichiuria) are all passed through human faeces, and are common throughout the tropics, especially in agricultural areas where open defecation is practiced, and shoes are not always worn [196]. Mass drug administration with anti-helminthic drugs is used to limit their morbidity in some countries. Infection with Strongyloides stercoralis, also transmitted through soil in endemic areas, often can be latent until the immune system is suppressed (or senescent), after which it can disseminate throughout the body with occasionally fatal effects [197]. These nematodes have in common the ability to penetrate human skin and migrate through subcutaneous tissues and blood vessels, entering the right heart circulation and eventually finding their way to the ocular tissues. Similarly, canine hookworm eggs (Ancylostoma spp.) are passed through dog faeces, from which they develop into larvae capable of penetrating human skin, for instance on beaches frequented by both dogs and humans. Infection is normally limited to (highly pruritic) cutaneous larva migrans on exposed body parts, but aberrant migration to the eye is also possible.
Food- and waterborne zoonotic helminthic eye infections can be transmitted through copepods [198], tiny crustaceans found virtually ubiquitously in bodies of water. Gnathostomiasis, another nematode cause of DSN [199] found mostly in southeast Asia, is one such example. Gnathostoma spp. eggs are passed through the faeces of definitive animal hosts into bodies of water, whereupon the eggs embryonate and form larvae which are ingested by copepods as the first intermediate host. These in turn are consumed by second intermediate hosts such as frogs, fish, snakes and ducks. Humans become infected by eating the undercooked meat of these animals, or possibly by drinking contaminated water, or even by applying the flesh of infected animals as a poultice for the eye [200]. Besides causing DSN, Gnathostoma spp. can prove highly destructive to the eye, invading orbital tissues [201] and the intraocular compartment [202] alike. It is probably a matter of chance whether a helminth capable of migrating through tissue ends up in the retina, the anterior chamber or the orbit.
In contrast, the rat lungworm, Angiostrongylus cantonensis, is not transmitted through copepods but through eating undercooked land snails [203]. The snails become infected by consuming eggs present in rat faeces [204]. Outbreaks of angiostrongyliasis have been known to occur at restaurants where snails are considered a delicacy. Considered endemic in some parts of eastern Asia, A. cantonensis is known to have spread widely [205]. Larvae from these nematodes can invade all ocular tissues, as well as the central nervous system and the optic nerve [203, 206].
Diffuse neuroretinitis has also been attributed to filarial nematode worms transmitted by mosquitoes, such as Brugia malayi [207], which is endemic in tropical coastal regions in south Asia. Humans are definitive hosts for these and other filarial parasites around the tropical belt, such Wuchereria bancrofti, which has been known to present as panuveitis [208].
Vector-borne transmission is possible even in temperate climates, such as southern Europe. Dirofilaria spp. (including the dog heartworm) are endemic in many parts of the world, including the Mediterranean, the primary hosts being wild and domestic canids and felids [209]. Humans can become infected following the bite of a mosquito vector, resulting in pulmonary or subcutaneous dirofilariasis. Ectopic infections in the orbital and ocular tissues are possible with some dirofilarial species and may cause severe visual loss.
Trichinella spp. is a nematode parasite with a worldwide distribution, commonly infecting domestic and wild pigs, as well as other wild animals [210]. The larvae encyst in striated muscle and are liberated by gastric juices in humans eating undercooked pork, especially in temperate climes. The female adult worms can burrow into the intestinal mucosa, passing larvae directly into the tissues and circulation to disseminate widely, including to the orbit, where they can cause chronic peri-orbital oedema and damage to intraocular structures [211]. While measures to raise food standards, such as freezing meat, have greatly reduced the incidence of trichinellosis in rich countries, the consumption of wild game perpetuates the risk of human infection.
The domestic pig is the intermediate host for Taenia solium, one of the better-known tapeworm infections to affect the eyes [212]. Consumption of measly pork containing encysted larvae (cysticerci) results in human tapeworm infection. The adult tapeworm attaches itself to the mucosal wall of the small intestine, shedding ova. The eggs may be ingested via faeco-oral autoinfection, or via contaminated food, following which the larvae penetrate the gut wall and migrate to any site in the body to form cysticerci. Most commonly, ophthalmic manifestations are orbital, although cysts may also appear in the vitreous cavity, the subretinal space and the anterior chamber. Ova shed by the dog tapeworm, Echinococcus granulosus, which causes hydatid disease, may occasionally be inadvertently ingested by humans. Rarely, cysts may seed the visual pathways and ocular structures causing severe sight impairment [213].
Sparganosis is another example of copepod transmission, in this case caused by the larvae of intestinal tapeworms, Spirometra spp. [214], present in domesticated and wild animals. The eggs are shed in the faeces of infected animals, and embryonate in water, releasing ciliated larvae which are ingested by copepods and undergo further stages of development. The copepods are consumed by fish and amphibians, providing a route for the Spirometra larvae to enter the human food chain. These larvae can cross the intestinal wall and migrate to ocular or orbital tissues, eliciting severe inflammation and eventual visual loss [215].
While trematodes have been reported to cause DSN [216] the most common ocular manifestation of a systemic trematode infection is probably presumed trematode-induced granulomas or granulomatous anterior uveitis, which has been reported in various tropical and subtropical countries where swimming in fresh water containing the snail host of various flukes risks infection, including Schistosoma spp. [217]. and Procerovum varium [218]. The trematode larvae (cercariae) penetrate the skin and are carried in the circulation to distal sites throughout the body, where they mature and lay eggs. Migration to the vessels surrounding the eye may result in ectopic ova, producing a granuloma in the anterior chamber or the ciliary body. In sheep-rearing countries, flukes such as Fasciola hepatica may rarely reach the eye ectopically [219], possibly following consumption of watercress contaminated with larval cysts.
Rare arthropod infections causing visual loss include internal ophthalmomyiasis, caused by the larvae of a variety of flies around the world, such as the sheep bot fly Oestrus ovis [220]. Once settled on the conjunctival surface, these larvae can burrow into the eye, forming characteristically long and wide subretinal tracks, and sometimes they appear in the vitreous cavity. Another rare arthropod eye infection, known as pentastomiasis, can occur following ingestion of undercooked snake meat infected with Armillifer armillatus [221], or by accidental ingestion of a canid nasopharyngeal parasite, Linguatula serrata, known as tongue worm [222]. These large organisms can cause severe destruction of the ocular tissues, leading to monocular blindness.
Summary
While no review on infectious ophthalmic disease can be comprehensive, it is a useful exercise to consider the spectrum of organisms that can infect the human eye, and the impact this group of diseases has on ocular morbidity and sight impairment. Together, these conditions cast a formidable shadow on global efforts to prevent unnecessary visual loss. Some of the major sight-threatening infections, such as herpesviruses infections, infectious keratitis and orbital cellulitis, as well as lesser-known entities like diffuse subacute neuroretinitis are often unilateral, whereas other common infections such as ocular tuberculosis and acquired toxoplasmosis are frequently asymmetric. The recognition of monocular visual impairment as a form of disability should drive more prevalence studies to evaluate the morbidity of these conditions.
As efforts to contain and suppress the major blinding infectious diseases, such as trachoma and onchocerciasis, continue to bear fruit, our attention naturally turns to other preventable eye diseases of global importance, such as cytomegalovirus retinitis, infectious keratitis and other helminthic eye infections. These, too, impose a disproportionate burden in developing societies. To capture the true burden of this unique group of diseases, it is proposed that future prevalence studies consider them in aggregate under one category. For a more comprehensive assessment, this categorisation could include the secondary sight threatening effects of infection and treatment, as well as post-infectious ocular conditions. This approach would help to direct resources, it is hoped, not just to cataract and refractive services, but also to other avoidable causes of blindness like ocular infections and inflammation which still need serious attention in many parts of the world [13, 223].
Success in halting the spread of trachoma and onchocerciasis has proven beyond doubt that collaborative multidisciplinary approaches can turn the tide against complex infectious diseases. Key interventions, of course, include vaccination, which is available for numerous viruses [224], bacteria [225] and even parasites [226]. The unprecedented success of messenger RNA vaccines in combating the SARS-CoV-2 pandemic gives much room for hope [227]. Public health initiatives to mitigate the impact of neglected tropical diseases will also reduce their visual burden, including mass drug administration [228], improvements in environmental hygiene [229], vector control [230] and improved access to healthcare [231].
The advent of telemedicine is now well-established, and many ophthalmologists count themselves among the converted, galvanised perhaps by the SARS-CoV-2 pandemic [232]. The highly visual specialty of ophthalmology, abetted by highly informative imaging, lends itself well to remote medicine, and it is envisaged to expand further as technology spreads. The widespread availability of mobile phones, enabling photography of external and, to a lesser extent, internal ocular structures [233], as well as relatively low-cost handheld retinal cameras [234], augurs well for the future of teleophthalmology. It has unmatched potential for the delivery of care in resource-poor settings, though significant challenges, including cost, electricity supply and acceptance, remain [235]. While the role of handheld fundus cameras in screening of diabetic retinopathy appears to be well established, their value in diagnosis of significantly more complex infectious eye disease presentations is as yet unclear.
We stand before a new era, as attested by apparent climate emergencies across the globe [236]. Extreme weather, degradation of the natural world, overpopulation, human incursion into animal habitats, conflict, international travel and food poverty conspire to stimulate the proliferation of vector-borne, zoonotic and other infectious diseases, while stymying human efforts to contain them, with untold consequences [231, 237]. What this portends for the future of human health and health systems remains a subject of intense debate, but it seems likely that infectious diseases, including those that threaten vision, will take centre stage [238]. Community-based surveillance programmes to detect and respond to outbreaks are already operational [239], and their scope is set to expand. In addition, WHO has recently launched a global network to detect infectious disease threats, harnessing the power of pathogen genomics across the globe [240]. At the same time, One Health Networks have emerged, seeking to address health inequality at a global level through multisectoral, transdisciplinary and community-orientated collaboration [241]. There is no question that ophthalmologists too will have a part to play, for example in reporting and managing presentations compatible with Emerging Infectious Diseases [11]. Global reporting networks may ultimately help to lift the veil on the true global burden of infectious eye disease.
Ultimately, sophisticated artificial intelligence (AI) systems may be required to process the intricate interplay between incoming information on diagnosis and epidemiological mapping of infectious eye disease on one hand and the mobilisation of resources and collaborative public health initiatives on the other, simultaneously factoring in ever-increasing environmental threats to healthcare [242]. Already established in various domains of ophthalmic healthcare [243], AI appears set to open the doors to a new era of information gathering and synthesis, transforming ophthalmology in hitherto unimagined ways.
References
Orrù CD, Soldau K, Cordano C, Llibre-Guerra J, Green AJ, Sanchez H, et al. Prion seeds distribute throughout the eyes of sporadic Creutzfeldt-Jakob disease patients. mBio. 2018;9:https://doi.org/10.1128/mbio.02095-18.
Panadero-Fontán R, Otranto D. Arthropods affecting the human eye. Vet Parasitol. 2015;208:84–93.
Lynn WA, Lightman S. The eye in systemic infection. Lancet. 2004;364:1439–50.
Hotez PJ, Aksoy S, Brindley PJ, Kamhawi S. What constitutes a neglected tropical disease? PLoS Negl Trop Dis. 2020;14:e0008001.
Rohr JR, Cohen JM. Understanding how temperature shifts could impact infectious disease. PLOS Biol. 2020;18:e3000938.
Vignier N, Bouchaud O. Travel, migration and emerging infectious diseases. EJIFCC 2018;29:175–9.
Taha H, Durham J, Reid S. Communicable diseases prevalence among refugees and asylum seekers: systematic review and meta-analysis. Infect Dis Rep. 2023;15:188–203.
Khairallah M, Kahloun R. Ocular manifestations of emerging infectious diseases. Curr Opin Ophthalmol. 2013;24:574.
Marí Saéz A, Weiss S, Nowak K, Lapeyre V, Zimmermann F, Düx A, et al. Investigating the zoonotic origin of the West African Ebola epidemic. EMBO Mol Med. 2015;7:17–23.
Alwine JC, Casadevall A, Enquist LW, Goodrum FD, Imperiale MJ. A critical analysis of the evidence for the SARS-CoV-2 origin hypotheses. J Virol. 2023;97:e00365–23.
Rose-Nussbaumer J, Doan T. Role of ophthalmology in emerging infectious diseases. JAMA Ophthalmol. 2022;140:935.
Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health 2021;9:e489–551.
Sommer A, Taylor HR, Ravilla TD, West S, Lietman TM, Keenan JD, et al. Challenges of ophthalmic care in the developing world. JAMA Ophthalmol. 2014;132:640–4.
Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman MH. Poverty and access to health care in developing countries. Ann NY Acad Sci. 2008;1136:161–71.
GBD 2019 Blindness and Vision Impairment Collaborators, Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e130–43.
Steinmetz JD, Bourne RRA, Briant PS, Flaxman SR, Taylor HRB, Jonas JB, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–60.
World Health Organisation. International statistical classification of diseases and related health problems [Internet]. 2016. Available from: https://icd.who.int/browse10/2016/en#/H53-H54. Accessed 26 Jul 2023.
McKibbin M, Farragher TM, Shickle D. Monocular and binocular visual impairment in the UK Biobank study: prevalence, associations and diagnoses. BMJ Open Ophthalmol. 2018;3:e000076.
Suttorp-Schulten MS, Rothova A. The possible impact of uveitis in blindness: a literature survey. Br J Ophthalmol. 1996;80:844–8.
Grzybowski A, Zülsdorff M, Wilhelm H, Tonagel F. Toxic optic neuropathies: an updated review. Acta Ophthalmol. 2015;93:402–10.
Cunningham ET, Forrester JV, Rao NA, Zierhut M. Post-infectious uveitis. Ocul Immunol Inflamm. 2016;24:603–6.
Scalabrin S, Becco A, Vitale A, Nuzzi R. Ocular effects caused by viral infections and corresponding vaccines: an overview of varicella zoster virus, measles virus, influenza viruses, hepatitis B virus, and SARS-CoV-2. Front Med [Internet]. 2022;9. Available from: https://www.frontiersin.org/articles/10.3389/fmed.2022.999251. Accessed 15 Jul 2023.
Venkatesh A, Patel R, Goyal S, Rajaratnam T, Sharma A, Hossain P. Ocular manifestations of emerging viral diseases. Eye. 2021;35:1117–39.
Cabrera-Aguas M, Khoo P, Watson SL. Infectious keratitis: a review. Clin Exp Ophthalmol. 2022;50:543–62.
Kahloun R, Abroug N, Ksiaa I, Mahmoud A, Zeghidi H, Zaouali S, et al. Infectious optic neuropathies: a clinical update. Eye Brain. 2015;7:59–81.
E.Cunningham ET, Zierhut M. Vision loss in uveitis. Ocul Immunol Inflamm. 2021;29:1037–9.
Pelletier J, Koyfman A, Long B. High risk and low prevalence diseases: orbital cellulitis. Am J Emerg Med. 2023;68:1–9.
Lee CS, Lee AY, Akileswaran L, Stroman D, Najafi-Tagol K, Kleiboeker S, et al. Determinants of outcomes of adenoviral keratoconjunctivitis. Ophthalmology. 2018;125:1344–53.
Koonin EV, Krupovic M, Agol VI. The Baltimore classification of viruses 50 years later: how does it stand in the light of virus evolution? Microbiol Mol Biol Rev. 2021;85:https://doi.org/10.1128/mmbr.00053-21.
Smit DP, Mathew DK, Khairallah M, Yeh S, Cunningham ET. A review of human ocular Rna virus infections excluding coronavirus, human T-cell lymphotropic virus, and arboviruses. Ocul Immunol Inflamm. 2023;1–7.
Rajaiya J, Saha A, Ismail AM, Zhou X, Su T, Chodosh J. Adenovirus and the cornea: more than meets the eye. Viruses. 2021;13:293.
Brydak-Godowska J, Turczyńska M, Przybyś M, Brydak LB, Kęcik D. Ocular complications in influenza virus infection. Ocul Immunol Inflamm. 2019;27:545–50.
Yeo S, Kim H, Lee J, Yi J, Chung YR. Retinal vascular occlusions in COVID-19 infection and vaccination: a literature review. Graefes Arch Clin Exp Ophthalmol. 2023;261:1793–808.
Benage M, Fraunfelder FW, Vaccine-Associated. Uveitis. Mo Med. 2016;113:48–52.
McCormick I, James C, Welton NJ, Mayaud P, Turner KME, Gottlieb SL, et al. Incidence of herpes simplex virus keratitis and other ocular disease: global review and estimates. Ophthalmic Epidemiol. 2022;29:353–62.
Cochrane TF, Silvestri G, McDowell C, Foot B, McAvoy CE. Acute retinal necrosis in the United Kingdom: results of a prospective surveillance study. Eye. 2012;26:370–8.
Ford N, Shubber Z, Saranchuk P, Pathai S, Durier N, O’Brien DP, et al. Burden of HIV-related cytomegalovirus retinitis in resource-limited settings: a systematic review. Clin Infect Dis. 2013;57:1351–61.
Zhu L, Zhu H. Ocular herpes: the pathophysiology, management and treatment of herpetic eye diseases. Virol Sin. 2014;29:327–42.
Grose C. Acute retinal necrosis caused by herpes simplex virus type 2 in children: reactivation of an undiagnosed latent neonatal herpes infection. Semin Pediatr Neurol. 2012;19:115–8.
Fowler K, Mucha J, Neumann M, Lewandowski W, Kaczanowska M, Grys M, et al. A systematic literature review of the global seroprevalence of cytomegalovirus: possible implications for treatment, screening, and vaccine development. BMC Public Health. 2022;22:1659.
Oh SJ, Lee JK, Shin OS. Aging and the immune system: the impact of immunosenescence on viral infection, immunity and vaccine immunogenicity. Immune Netw. 2019;19:e37.
Tsatsos M, Athanasiadis I, Myrou A, M Saleh G, Ziakas N. Herpes zoster ophthalmicus: a devastating disease coming back with vengeance or finding its nemesis? J Ophthalmic Vis Res. 2022;17:123–9.
Stone J, Looker KJ, Silhol R, Turner KME, Hayes R, Coetzee J, et al. The population impact of herpes simplex virus type 2 (HSV-2) vaccination on the incidence of HSV-2, HIV and genital ulcer disease in South Africa: a mathematical modelling study. eBioMedicine [Internet]. 2023;90. Available from: https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(23)00095-6/fulltext. Accessed 15 Jul 2023.
Chan NSW, Chee SP, Caspers L, Bodaghi B. Clinical features of CMV-associated anterior uveitis. Ocul Immunol Inflamm. 2018;26:107–15.
London NJ, Tun N, Kyaw MK, Smithuis F, Heiden D. Mortality and a CMV retinitis strategy for resource-poor settings. Invest Ophthalmol Vis Sci. 2010;51:2913.
Gabrani C, Mitsikas D, Giannakou K, Lamnisos D. Congenital cytomegalovirus infection and ophthalmological disorders: a systematic review. J Pediatr Ophthalmol Strabismus. 2023;60:86–94.
Cunningham ET, Zierhut M. Epstein-Barr virus and the eye. Ocul Immunol Inflamm. 2020;28:533–7.
Donzel M, Bonjour M, Combes JD, Broussais F, Sesques P, Traverse-Glehen A, et al. Lymphomas associated with Epstein-Barr virus infection in 2020: results from a large, unselected case series in France. eClinicalMedicine [Internet]. 2022;54. Available from: https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(22)00404-7/fulltext. Accessed 12 Aug 2023.
Donovan C, Patel H, Shetty S, Bierman L, Lustbader JM, Oboh-Weilke AM. Aggressive conjunctival Kaposi sarcoma as the initial manifestation of acquired immunodeficiency syndrome. Am J Ophthalmol Case Rep. 2020;19:100832.
Smit DP, Meyer D. HIV-induced uveitis: would you recognize it if it looked straight at you? AIDS. 2017;31:1777.
Banker AS, Chauhan R, Banker DA. HIV and opportunistic eye diseases. Expert Rev Ophthalmol. 2009;4:173–85.
Feroze KB, Wang J Ocular Manifestations of HIV. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. Available from: http://www.ncbi.nlm.nih.gov/books/NBK441926/. Accessed 8 Jul 2023.
Laovirojjanakul W, Thanathanee O. Opportunistic ocular infections in the setting of HIV. Curr Opin Ophthalmol. 2018;29:558–65.
Peters RPH, Kestelyn PG, Zierhut M, Kempen JH. The changing global epidemic of HIV and ocular disease. Ocul Immunol Inflamm. 2020;28:1007–14.
Kempen JH, Min YI, Freeman WR, Holland GN, Friedberg DN, Dieterich DT, et al. Risk of immune recovery uveitis in patients with AIDS and cytomegalovirus retinitis. Ophthalmology. 2006;113:684–94.
Rathinam SR, Lalitha P. Paradoxical worsening of ocular tuberculosis in HIV patients after antiretroviral therapy. Eye. 2007;21:667–8.
Yang M, Kamoi K, Zong Y, Zhang J, Ohno-Matsui K. Human immunodeficiency virus and uveitis. Viruses. 2023;15:444.
Kamoi K, Watanabe T, Uchimaru K, Okayama A, Kato S, Kawamata T, et al. Updates on HTLV-1 uveitis. Viruses. 2022;14:794.
Sherwin JC, Reacher MH, Dean WH, Ngondi J. Epidemiology of vitamin A deficiency and xerophthalmia in at-risk populations. Trans R Soc Trop Med Hyg. 2012;106:205–14.
Gilbert C, Bowman R, Malik AN. The epidemiology of blindness in children: changing priorities. Community Eye Health. 2017;30:74–7.
Stevens GA, Bennett JE, Hennocq Q, Lu Y, De-Regil LM, Rogers L, et al. Trends and mortality effects of vitamin A deficiency in children in 138 low-income and middle-income countries between 1991 and 2013: a pooled analysis of population-based surveys. Lancet Glob Health. 2015;3:e528–36.
Pandey A, Galvani AP. Exacerbation of measles mortality by vaccine hesitancy worldwide. Lancet Glob Health. 2023;11:e478–9.
Duszak RS. Congenital rubella syndrome—major review. Optom - J Am Optom Assoc. 2009;80:36–43.
Zimmerman LA, Knapp JK, Antoni S, Grant GB, Reef SE. Progress toward rubella and congenital rubella syndrome control and elimination—worldwide, 2012–2020. Morb Mortal Wkly Rep. 2022;71:196–201.
Vijayalakshmi P, Kakkar G, Samprathi A, Banushree R. Ocular manifestations of congenital rubella syndrome in a developing country. Indian J Ophthalmol. 2002;50:307.
Quentin CD, Reiber H. Fuchs heterochromic cyclitis: rubella virus antibodies and genome in aqueous humor. Am J Ophthalmol. 2004;138:46–54.
Birnbaum AD, Tessler HH, Schultz KL, Farber MD, Gao W, Lin P, et al. Epidemiologic relationship between fuchs heterochromic iridocyclitis and the United States rubella vaccination program. Am J Ophthalmol. 2007;144:424–428.e2.
Brady OJ, Hay SI. The global expansion of dengue: how aedes aegypti mosquitoes enabled the first pandemic arbovirus. Annu Rev Entomol. 2020;65:191–208.
Mondal N. The resurgence of dengue epidemic and global warming in India. Lancet. 2023;401:727–8.
Katzelnick LC, Gresh L, Halloran ME, Mercado JC, Kuan G, Gordon A, et al. Antibody-dependent enhancement of severe dengue disease in humans. Science. 2017;358:929–32.
Tabbara K. Dengue retinochoroiditis. Ann Saudi Med. 2012;32:530–3.
Ng AW, Teoh SC. Dengue eye disease. Surv Ophthalmol. 2015;60:106–14.
Su DHW, Bacsal K, Chee SP, Flores JVP, Lim WK, Cheng BCL, et al. Prevalence of dengue maculopathy in patients hospitalized for dengue fever. Ophthalmology. 2007;114:1743–1747.e4.
Wagle AM, Hegde SR, Sanjay S, Au Eong KG. Ophthalmic manifestations in seropositive dengue fever patients during epidemics caused by predominantly different dengue serotypes. Adv Ophthalmol Pract Res. 2022;2:100049.
Wilder-Smith A. Dengue vaccine development: status and future. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2020;63:40–4.
Edenborough KM, Flores HA, Simmons CP, Fraser JE. Using Wolbachia to eliminate dengue: will the virus fight back? J Virol. 2021;10;95:https://doi.org/10.1128/jvi.02203-20.
Bartholomeeusen K, Daniel M, LaBeaud DA, Gasque P, Peeling RW, Stephenson KE, et al. Chikungunya fever. Nat Rev Dis Prim. 2023;9:1–21.
da Silva LCM, da Silva Platner F, da Silva Fonseca L, Rossato VF, de Andrade DCP, de Sousa Valente J, et al. Ocular manifestations of chikungunya infection: a systematic review. Pathogens. 2022;11:412.
de Andrade GC, Ventura CV, Mello Filho PA, de A, Maia M, Vianello S, et al. Arboviruses and the eye. Int J Retin Vitr. 2017;3:4.
Rousseau A, Haigh O, Ksiaa I, Khairallah M, Labetoulle M. Ocular manifestations of west nile virus. Vaccines. 2020;8:641.
Palmer PI, Wainwright CM, Dong B, Maidment RI, Wheeler KG, Gedney N, et al. Drivers and impacts of Eastern African rainfall variability. Nat Rev Earth Environ. 2023;4:254–70.
Wright D, Kortekaas J, Bowden TA, Warimwe GM. Rift valley fever: biology and epidemiology. J Gen Virol. 2019;100:1187–99.
Al-Hazmi A, Al-Rajhi AA, Abboud EB, Ayoola EA, Al-Hazmi M, Saadi R, et al. Ocular complications of Rift valley fever outbreak in Saudi Arabia. Ophthalmology. 2005;112:313–8.
Shantha JG, Crozier I, Varkey JB, Kraft CS, Marshall Lyon G, et al. Long-term management of panuveitis and iris heterochromia in an Ebola survivor. Ophthalmology. 2016;123:2626–2628.e2.
Sneller MC, Reilly C, Badio M, Bishop RJ, Eghrari AO, Moses SJ, et al. A longitudinal study of Ebola sequelae in Liberia. N Engl J Med. 2019;380:924–34.
Testi I, Brandão-de-Resende C, Agrawal R, Pavesio C, Steeples L, Balasubramaniam B, et al. Ocular inflammatory events following COVID-19 vaccination: a multinational case series. J Ophthalmic Inflamm Infect. 2022;12:4.
Beck AP, Jampol LM, Glasser DA, Pollack JS. Is coxsackievirus the cause of unilateral acute idiopathic maculopathy? Arch Ophthalmol. 2004;122:121–3.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for multiple evanescent white dot syndrome. Am J Ophthalmol. 228:198–204. 2021
Papasavvas I, Mantovani A, Tugal-Tutkun I, Herbort CP. Multiple evanescent white dot syndrome (MEWDS): update on practical appraisal, diagnosis and clinicopathology; a review and an alternative comprehensive perspective. J Ophthalmic Inflamm Infect. 2021;11:45.
Burton MJ, Mabey DCW. The global burden of trachoma: a review. PLoS Negl Trop Dis. 2009;3:e460.
Hu VH, Harding-Esch EM, Burton MJ, Bailey RL, Kadimpeul J, Mabey DCW. Epidemiology and control of trachoma: systematic review. Trop Med Int Health. 2010;15:673–91.
Solomon AW, Burton MJ, Gower EW, Harding-Esch EM, Oldenburg CE, Taylor HR, et al. Trachoma. Nat Rev Dis Prim. 2022;8:1–20.
He J, Chen A, Zou M, Young CA, Jin L, Zheng D, et al. Time trends and heterogeneity in the disease burden of trachoma, 1990–2019: a global analysis. Br J Ophthalmol. 2023;107:337–41.
Habtamu E, Wondie T, Aweke S, Tadesse Z, Zerihun M, Zewudie Z, et al. Posterior lamellar versus bilamellar tarsal rotation surgery for trachomatous trichiasis in Ethiopia: a randomised controlled trial. Lancet Glob Health. 2016;4:e175–84.
Emerson PM, Burton M, Solomon AW, Bailey R, Mabey D. The SAFE strategy for trachoma control: Using operational research for policy, planning and implementation. Bull World Health Organ. 2006;84:613–9.
Renneker KK, Abdala M, Addy J, Al-Khatib T, Amer K, Badiane MD, et al. Global progress toward the elimination of active trachoma: an analysis of 38 countries. Lancet Glob Health. 2022;10:e491–500.
Murray KA, Preston N, Allen T, Zambrana-Torrelio C, Hosseini PR, Daszak P. Global biogeography of human infectious diseases. Proc Natl Acad Sci. 2015;112:12746–51.
Yaisawang S, Asawaphureekorn S, Chetchotisakd P, Wongratanacheewin S, Pakdee P. Ocular involvement in melioidosis: a 23-year retrospective review. J Ophthalmic Inflamm Infect. 2018;8:5.
Limmathurotsakul D, Golding N, Dance DAB, Messina JP, Pigott DM, Moyes CL, et al. Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis. Nat Microbiol. 2016;1:1–5.
Whitcher JP, Srinivasan M. Corneal ulceration in the developing world—a silent epidemic. Br J Ophthalmol. 1997;81:622–3.
Ung L, Acharya NR, Agarwal T, Alfonso EC, Bagga B, Bispo PJ, et al. Infectious corneal ulceration: a proposal for neglected tropical disease status. Bull World Health Organ. 2019;97:854–6.
Mallika P, Asok T, Faisal H, Aziz S, Tan A, Intan G.Neonatal conjunctivitis—a review.Malays Fam Physician J. 2008;3:77–81.
Sahoo S, Alluri H, Mitra S, Priyadarshini S, Sahu SK, Mohanty A, et al. Multidrug-resistant keratitis: challenging yet manageable. Br J Ophthalmol. 2023;107:769–73.
Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–34.
Ting DSJ, Gopal BP, Deshmukh R, Seitzman GD, Said DG, Dua HS. Diagnostic armamentarium of infectious keratitis: a comprehensive review. Ocul Surf. 2022;23:27–39.
Mselle J. Visual impact of using traditional medicine on the injured eye in Africa. Acta Trop. 1998;70:185–92.
Pedrotti E, Bonacci E, Kilian R, Pagnacco C, Fasolo A, Anastasi M, et al. The role of topical povidone-iodine in the management of infectious keratitis: a pilot study. J Clin Med. 2022;11:848.
Tsirouki T, Dastiridou AI, Ibánez flores N, Cerpa JC, Moschos MM, Brazitikos P, et al. Orbital cellulitis. Surv Ophthalmol. 2018;63:534–53.
Gilsdorf JR. Hib vaccines: their impact on Haemophilus influenzae Type b disease. J Infect Dis. 2021;224:S321–30.
Sharma S, Grover M, Bhargava S, Samdani S, Kataria T. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol. 2021;135:442–7.
Fabiani C, Agarwal M, Dogra M, Tosi GM, Davis JL. Exogenous endophthalmitis. Ocul Immunol Inflamm. 2022;0:1–10.
Xie CA, Singh J, Tyagi M, Androudi S, Dave VP, Arora A, et al. Endogenous endophthalmitis—a major review. Ocul Immunol Inflamm. 2022;0:1–24.
Durand ML. Bacterial and fungal endophthalmitis. Clin Microbiol Rev. 2017;30:597–613.
Gentile RC, Shukla S, Shah M, Ritterband DC, Engelbert M, Davis A, et al. Microbiological spectrum and antibiotic sensitivity in endophthalmitis: a 25-year review. Ophthalmology. 2014;121:1634–42.
Fowler BJ, Miller D, Yan X, Yannuzzi NA, Flynn Jr HW. Postoperative endophthalmitis caused by cutibacterium (formerly propionibacterium) acnes: case series and review. Case Rep. Ophthalmol. 2021;12:1–10.
Serban D, Popa Cherecheanu A, Dascalu AM, Socea B, Vancea G, Stana D, et al. Hypervirulent Klebsiella pneumoniae endogenous endophthalmitis—a global emerging disease. Life. 2021;11:676.
Specht CS, Laver NV. Epidemiology and clinical significance of ocular infection. In: Laver NV, Specht CS, editors. The infected eye: clinical practice and pathological principles [Internet]. Cham: Springer International Publishing; 2016. p. 1–11. https://doi.org/10.1007/978-3-319-42840-6_1. Accessed 19 Jul 2023.
Haseeb AA, Elhusseiny AM, Siddiqui MZ, Ahmad KT, Sallam AB. Fungal endophthalmitis: a comprehensive review. J Fungi. 2021;7:996.
Shankland GS, Richardson MD, Dutton GN. Source of infection in candida endophthalmitis in drug addicts. Br Med J Clin Res Ed. 1986;292:1106–7.
Gunasekeran DV, Gupta B, Cardoso J, Pavesio CE, Agrawal R. Visual morbidity and ocular complications in presumed intraocular tuberculosis: an analysis of 354 cases from a non-endemic population. Ocul Immunol Inflamm. 2018;26:865–9.
Bagcchi S. WHO’s global tuberculosis report 2022. Lancet Microbe. 2023;4:e20.
Kon OM, Beare N, Connell D, Damato E, Gorsuch T, Hagan G, et al. BTS clinical statement for the diagnosis and management of ocular tuberculosis. BMJ Open Respir Res. 2022;9:e001225.
Petrushkin H, Sethi C, Potter J, Martin L, Russell G, White V, et al. Developing a pathway for the diagnosis and management of ocular tuberculosis. The pan-LOndon Ocular tuberculosis Pathway—LOOP. Eye. 2020;34:805–8.
Dewan PK, Grinsdale J, Kawamura LM. Low sensitivity of a whole-blood interferon-γ release assay for detection of active tuberculosis. Clin Infect Dis. 2007;44:69–73.
Agrawal R, Ludi Z, Betzler BK, Testi I, Mahajan S, Rousellot A, et al. The Collaborative Ocular Tuberculosis Study (COTS) calculator—a consensus-based decision tool for initiating antitubercular therapy in ocular tuberculosis. Eye. 2023;37:1416–23.
Ganesh SK, Abraham S, Sudharshan S. Paradoxical reactions in ocular tuberculosis. J Ophthalmic Inflamm Infect. 2019;9:19.
Nyang’wa BT, Berry C, Kazounis E, Motta I, Parpieva N, Tigay Z, et al. A 24-week, all-oral regimen for rifampin-resistant tuberculosis. N Engl J Med. 2022;387:2331–43.
Grzybowski A, Nita M, Virmond M. Ocular leprosy. Clin Dermatol. 2015;33:79–89.
Rathinam SR, Parikh JG, Rao NA. Ocular erythema nodosum leprosum: an immunohistochemical study. Indian J Ophthalmol. 2020;68:2028–30.
Soni D, Sharma B, Karkhur S. Anterior chamber angle granuloma: a rare ocular manifestation of histoid lepromatous leprosy. Indian J Ophthalmol. 2020;68:2031.
Talhari C, Talhari S, Penna GO. Clinical aspects of leprosy. Clin Dermatol. 2015;33:26–37.
Clare G, Mitchell S. Iris root abscess and necrotizing sclerokeratitis caused by mycobacterium abscessus and presenting as hemorrhagic anterior uveitis. Cornea. 2008;27:255.
Kalogeropoulos D, Asproudis I, Stefaniotou M, Moschos M, Gartzonika C, Bassukas I, et al. Spirochetal uveitis: Spectrum of clinical manifestations, diagnostic and therapeutic approach, final outcome and epidemiological data. Int Ophthalmol. 2021;41:4111–26.
Jakab Á, Kahlig P, Kuenzli E, Neumayr A. Tick borne relapsing fever - a systematic review and analysis of the literature. PLoS Negl Trop Dis. 2022;16:e0010212.
Mendez-Lopez A, Stuckler D, Marcus U, Hickson F, Noori T, Whittaker RN, et al. Social and behavioural determinants of syphilis: modelling based on repeated cross-sectional surveys from 2010 and 2017 among 278,256 men who have sex with men in 31 European countries. Lancet Reg Health – Eur [Internet]. 2022;22. Available from: https://www.thelancet.com/journals/lanepe/article/PIIS2666-7762(22)00179-X/fulltext. Accessed 21 Jul 2023.
Holt M, Newman CE, Lancaster K, Smith AK, Hughes S, Truong HHM. HIV pre-exposure prophylaxis and the ‘problems’ of reduced condom use and sexually transmitted infections in Australia: a critical analysis from an evidence-making intervention perspective. Socio Health Illn. 2019;41:1535–48.
Furtado JM, Simões M, Vasconcelos-Santos D, Oliver GF, Tyagi M, Nascimento H, et al. Ocular syphilis. Surv Ophthalmol. 2022;67:440–62.
Woolston SL, Dhanireddy S, Marrazzo J. Ocular syphilis: a clinical review. Curr Infect Dis Rep. 2016;18:36.
Chen C, Wang S, Li X. Acute syphilitic posterior placoid chorioretinitis misdiagnosed as systemic lupus erythematosus associated uveitis. Ocul Immunol Inflamm. 2020;28:1116–24.
Henao-Martínez AF, Johnson SC. Diagnostic tests for syphilis. Neurol Clin Pr. 2014;4:114–22.
Shukla D, Rathinam SR, Cunningham ETJ. Leptospiral uveitis in the developing world. Int Ophthalmol Clin. 2010;50:113.
Rathinam SR, Namperumalsamy P. Global variation and pattern changes in epidemiology of uveitis. Indian J Ophthalmol. 2007;55:173.
Rathinam SR. Ocular manifestations of leptospirosis. J Postgrad Med. 2005;51:189.
Arrieta-Bechara CE, Carrascal-Maldonado AY. Ocular leptospirosis: a review of current state of art of a neglected disease. Rom J Ophthalmol. 2022;66:282–8.
Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, et al. Leptospirosis: a zoonotic disease of global importance. Lancet Infect Dis. 2003;3:757–71.
Raja H, Starr MR, Bakri SJ. Ocular manifestations of tick-borne diseases. Surv Ophthalmol. 2016;61:726–44.
Zhang YY, Sun YQ, Chen JJ, Teng AY, Wang T, Li H, et al. Mapping the global distribution of spotted fever group rickettsiae: a systematic review with modelling analysis. Lancet Digit Health. 2023;5:e5–15.
Kahloun R, Gargouri S, Abroug N, Sellami D, Ben Yahia S, Feki J, et al. Visual loss associated with rickettsial disease. Ocul Immunol Inflamm. 2014;22:373–8.
Ericsson CD, Jensenius M, Fournier PE, Raoult D. Rickettsioses and the international traveler. Clin Infect Dis. 2004;39:1493–9.
Biancardi AL, Curi ALL. Cat-scratch disease. Ocul Immunol Inflamm. 2014;22:148–54.
Johnson A. Ocular complications of cat scratch disease. Br J Ophthalmol. 2020;104:1640–6.
Hu V, Dong B, MacFarlane A. Visual loss after cat scratch. J R Soc Med. 2005;98:28–9.
Ma C, Li H, Lu S, Li X, Wang S, Wang W. Ocular lesions in brucella infection: a review of the literature. Infect Drug Resist. 2022;15:7601–17.
Bazzazi N, Yavarikia A, Keramat F. Ocular involvement of brucellosis. Middle East Afr J Ophthalmol. 2013;20:95–7.
Rolando I, Olarte L, Vilchez G, Lluncor M, Otero L, Paris M, et al. Ocular manifestations associated with brucellosis: a 26-year experience in Peru. Clin Infect Dis. 2008;46:1338–45.
Goodwin ZI, Pascual DW. Brucellosis vaccines for livestock. Vet Immunol Immunopathol. 2016;181:51–8.
Tinley C, Zyl LV, Grötte R. Poststreptococcal syndrome uveitis in South African children. Br J Ophthalmol. 2012;96:87–9.
Hahn RG, Knox LM, Forman TA. Evaluation of poststreptococcal illness. Am Fam Physician. 2005;71:1949–54.
Vasconcelos-Santos DV, Lim JI, Rao NA. Chronic coccidioidomycosis endophthalmitis without concomitant systemic involvement: a clinicopathological case report. Ophthalmology. 2010;117:1839–42.
Oke I, Loporchio DF, Siegel NH, Subramanian ML, LaMattina KC. Chorioretinal paracoccidioidomycosis treated with intravitreal voriconazole and therapeutic vitrectomy. Am J Ophthalmol Case Rep. 2021;23:101187.
Prasad AG, Van Gelder RN. Presumed ocular histoplasmosis syndrome. Curr Opin Ophthalmol. 2005;16:364–8.
Widaty S, Santoso ID, Ricky D, Yunihastuti E, Rihatmadja R, Wahyuningsih R. Talaromycosis clinically and histopathologically mimicking histoplasmosis in an immunocompromised patient. Dermatol Online J [Internet]. 2020,26. https://escholarship.org/uc/item/9r49g227. Accessed 21 Jul 2023.
Ramírez-Soto MC, Tirado-Sánchez A, Bonifaz A. Ocular sporotrichosis. J Fungi. 2021;7:951.
Otranto D, Eberhard ML. Zoonotic helminths affecting the human eye. Parasit Vectors. 2011;4:41.
Wilhelmus KR, Jones DB, Matoba AY, Hamill MB, Pflugfelder SC, Weikert MP. Bilateral acanthamoeba keratitis. Am J Ophthalmol. 2008;145:193–197.e1.
Varacalli G, Di Zazzo A, Mori T, Dohlman TH, Spelta S, Coassin M, et al. Challenges in acanthamoeba keratitis: a review. J Clin Med. 2021;10:942.
Rayamajhee B, Willcox MD, Henriquez FL, Petsoglou C, Carnt N. Acanthamoeba keratitis: an increasingly common infectious disease of the cornea. Lancet Microbe. 2021;2:e345–6.
Saadatnia G, Golkar M. A review on human toxoplasmosis. Scand J Infect Dis. 2012;44:805–14.
Jones JL, Lopez A, Wilson M, Schulkin J, Gibbs R. Congenital toxoplasmosis: a review. Obstet Gynecol Surv. 2001;56:296.
Krueger WS, Hilborn ED, Converse RR, Wade TJ. Drinking water source and human Toxoplasma gondii infection in the United States: a cross-sectional analysis of NHANES data. BMC Public Health. 2014;14:711.
Messier V, Lévesque B, Proulx JF, Rochette L, Libman MD, Ward BJ, et al. Seroprevalence of Toxoplasma gondii Among Nunavik Inuit (Canada). Zoonoses Public Health. 2009;56:188–97.
Johnson MW, Greven CM, Jaffe GJ, Sudhalkar H, Vine AK. Atypical, severe toxoplasmic retinochoroiditis in elderly patients. Ophthalmology. 1997;104:48–57.
Leroy J, Houzé S, Dardé ML, Yéra H, Rossi B, Delhaes L, et al. Severe toxoplasmosis imported from tropical Africa in immunocompetent patients: a case series. Travel Med Infect Dis. 2020;35:101509.
Ahmed M, Sood A, Gupta J. Toxoplasmosis in pregnancy. Eur J Obstet Gynecol Reprod Biol. 2020;255:44–50.
El Hassan AM, Khalil EAG, El Sheikh EA, Zijlstra EE, Osman A, Ibrahim ME. Post kala-azar ocular leishmaniasis. Trans R Soc Trop Med Hyg. 1998;92:177–9.
Burza S, Croft SL, Boelaert M. Leishmaniasis. Lancet. 2018;392:951–70.
Ready PD. Epidemiology of visceral leishmaniasis. Clin Epidemiol. 2014;6:147–54.
Khalil E, Musa A, Musa B, Elfaki M, Zijlstra E, Elhassan A. Blindness following visceral leishmaniasis: a neglected post-kala-azar complication. Trop Doct. 2011;41:139–40.
Moore EM, Lockwood DN. Treatment of visceral leishmaniasis. J Glob Infect Dis. 2010;2:151–8.
Frallonardo L, Di Gennaro F, Panico GG, Novara R, Pallara E, Cotugno S, et al. Onchocerciasis: current knowledge and future goals. Front Trop Dis [Internet]. 2022, Vol. 3. Available from: https://www.frontiersin.org/articles/10.3389/fitd.2022.986884. Accessed 13 Aug 2023.
Newland HS, White AT, Greene BM, Murphy RP, Taylor HR. Ocular manifestations of onchocerciasis in a rain forest area of West Africa. Br J Ophthalmol. 1991;75:163–9.
Hotez P. Mass drug administration and integrated control for the world’s high-prevalence neglected tropical diseases. Clin Pharm Ther. 2009;85:659–64.
Campillo JT, Boussinesq M, Bertout S, Faillie JL, Chesnais CB. Serious adverse reactions associated with ivermectin: a systematic pharmacovigilance study in sub-Saharan Africa and in the rest of the world. PLoS Negl Trop Dis. 2021;15:e0009354.
Kamgno J, Pion SD, Chesnais CB, Bakalar MH, D’Ambrosio MV, Mackenzie CD, et al. A test-and-not-treat strategy for onchocerciasis in Loa loa–endemic areas. N. Engl J Med. 2017;377:2044–52.
Klion AD, Massougbodji A, Horton J, Ekoué S, Lanmasso T, Ahouissou NL, et al. Albendazole in human loiasis: results of a double-blind, placebo-controlled trial. J Infect Dis. 1993;168:202–6.
Turner JD, Tendongfor N, Esum M, Johnston KL, Langley RS, Ford L, et al. Macrofilaricidal activity after doxycycline only treatment of Onchocerca volvulus in an area of Loa loa co-endemicity: a randomized controlled trial. PLoS Negl Trop Dis. 2010;4:e660.
Das D, Ramachandra V, Islam S, Bhattacharjee H, Biswas J, Koul A, et al. Update on pathology of ocular parasitic disease. Indian J Ophthalmol. 2016;64:794–802.
Woodhall D, Starr MC, Montgomery SP, Jones JL, Lum F, Read RW, et al. Ocular toxocariasis: epidemiologic, anatomic, and therapeutic variations based on a survey of ophthalmic subspecialists. Ophthalmology. 2012;119:1211–7.
Hare AQ, Franco-Paredes C. Ocular Larva migrans: a severe manifestation of an unseen epidemic. Curr Trop Med Rep. 2014;1:69–73.
Ahn SJ, Ryoo NK, Woo SJ. Ocular toxocariasis: clinical features, diagnosis, treatment, and prevention. Asia Pac Allergy. 2014;4:134–41.
Gass JD, Scelfo R. Diffuse unilateral subacute neuroretinitis. J R Soc Med. 1978;71:95–111.
de Souza EC, Abujamra S, Nakashima Y, Gass JDM. Diffuse bilateral subacute neuroretinitis: first patient with documented nematodes in both eyes. Arch Ophthalmol. 1999;117:1349–51.
Garcia CAdeA, Sabrosa NA, Gomes AB, Segundo PdeS, Garcia Filho CAdeA, Sabrosa AS. Diffuse unilateral subacute neuroretinitis—DUSN. Int Ophthalmol Clin. 2008;48:119.
Goldberg MA, Kazacos KR, Boyce WM, Ai E, Katz B. Diffuse unilateral subacute neuroretinitis: morphometric, serologic, and epidemiologic support for baylisascaris as a causative agent. Ophthalmology. 1993;100:1695–701.
Sabrosa N, Zajdenweber M. Nematode infections of the eye: toxocariasis, onchocerciasis, diffuse unilateral subacute neuroretinitis, and cysticercosis. Ophthalmol Clin N. Am. 2002;15:351–6.
Jourdan PM, Lamberton PHL, Fenwick A, Addiss DG. Soil-transmitted helminth infections. Lancet. 2018;391:252–65.
Luvira V, Siripoon T, Phiboonbanakit D, Somsri K, Watthanakulpanich D, Dekumyoy P. Strongyloides stercoralis: a neglected but fatal parasite. Trop Med Infect Dis. 2022;7:310.
Bass D, Rueckert S, Stern R, Cleary AC, Taylor JD, Ward GM, et al. Parasites, pathogens, and other symbionts of copepods. Trends Parasitol. 2021;37:875–89.
Pillai GS, Kumar A, Radhakrishnan N, Maniyelil J, Shafi T, Dinesh KR, et al. Intraocular gnathostomiasis: report of a case and review of literature. Am J Trop Med Hyg. 2012;86:620–3.
Wiwanitkit V. Ocular sparganosis. Orbit. 2014;33:474–474.
Preechawat P, Wongwatthana P, Poonyathalang A, Chusattayanond A. Orbital apex syndrome from gnathostomiasis. J Neuro-Ophthalmol J North Am Neuro-Ophthalmol Soc. 2006;26:184–6.
Rawat P, Gautam M, Jain NC, Jain R. Intraocular gnathostomiasis: a rare case report from Central India. Indian J Ophthalmol. 2016;64:235–7.
Feng Y, Nawa Y, Sawanyavisuth K, Lv Z, Wu ZD. Comprehensive review of ocular angiostrongyliasis with special reference to optic Neuritis. Korean J Parasitol. 2013;51:613–9.
Lv S, Zhang Y, Liu HX, Hu L, Yang K, Steinmann P, et al. Invasive snails and an emerging infectious disease: results from the first national survey on Angiostrongylus cantonensis in China. PLoS Negl Trop Dis. 2009;3:e368.
Martín-Carrillo N, Feliu C, Abreu-Acosta N, Izquierdo-Rodriguez E, Dorta-Guerra R, Miquel J, et al. A peculiar distribution of the emerging nematode Angiostrongylus cantonensis in the Canary Islands (Spain): Recent Introduction Or Isolation Effect? Animals. 2021;11:1267.
Murugan SB. Commentary: angiostrongylus cantonensis in anterior chamber. Indian J Ophthalmol. 2019;67:161–2.
Myint K, Sahay R, Mon S, Saravanan VR, Narendran V, Dhillon B. Worm in the eye”: the rationale for treatment of DUSN in south India. Br J Ophthalmol. 2006;90:1125–7.
Ganesh SK, Babu K, Krishnakumar S, Biswas J. Ocular filariasis due to Wuchereria bancrofti presenting as panuveitis: a case report. Ocul Immunol Inflamm. 2003;11:145–8.
Kalogeropoulos CD, Stefaniotou MI, Gorgoli KE, Papadopoulou CV, Pappa CN, Paschidis CA. Ocular dirofilariasis: a case series of 8 patients. Middle East Afr J Ophthalmol. 2014;21:312–6.
Kaewpitoon N, Kaewpitoon SJ, Pengsaa P. Food-borne parasitic zoonosis: distribution of trichinosis in Thailand. World J Gastroenterol WJG. 2008;14:3471–5.
Kocięcki J, Czaplicka E, Kocięcka W. Ocular system involvement in the course of human trichinellosis. Pathological and diagnostic aspects. Acta Parasitol. 2014;59:493–501.
Dhiman R, Devi S, Duraipandi K, Chandra P, Vanathi M, Tandon R, et al. Cysticercosis of the eye. Int J Ophthalmol. 2017;10:1319–24.
Konar KD, Pillay S. A case and literature review of intraocular echinococcus causing bilateral visual loss in a HIV-infected patient. SAGE Open Med Case Rep. 2022;10:2050313X221113699.
Liu Q, Li MW, Wang ZD, Zhao GH, Zhu XQ. Human sparganosis, a neglected food borne zoonosis. Lancet Infect Dis. 2015;15:1226–35.
Ye H, Du Y, Liu G, Luo X, Yang H. Clinical features of 8 cases of orbital sparganosis in southern China. Can J Ophthalmol. 2012;47:453–7.
McDonald HR, Kazacos KR, Schatz H, Johnson RN. Two cases of intraocular infection with Alaria mesocercaria (Trematoda). Am J Ophthalmol. 1994;117:447–55.
El Nokrashy A, Abou Samra W, Sobeih D, Lamin A, Hashish A, Tarshouby S, et al. Treatment of presumed trematode-induced granulomatous anterior uveitis among children in rural areas of Egypt. Eye. 2019;33:1525–33.
Rathinam SR, Usha KR, Rao NA. Presumed trematode-induced granulomatous anterior uveitis: a newly recognized cause of intraocular inflammation in children from south India. Am J Ophthalmol. 2002;133:773–9.
Dalimi A, Jabarvand M. Fasciola hepatica in the human eye. Trans R Soc Trop Med Hyg. 2005;99:798–800.
Pupić-Bakrač A, Pupić-Bakrač J, Škara Kolega M, Beck R. Human ophthalmomyiasis caused by Oestrus ovis-first report from Croatia and review on cases from Mediterranean countries. Parasitol Res. 2020;119:783–93.
Sulyok M, Rózsa L, Bodó I, Tappe D, Hardi R. Ocular pentastomiasis in the Democratic Republic of the Congo. PLoS Negl Trop Dis. 2014;8:e3041.
Koehsler M, Walochnik J, Georgopoulos M, Pruente C, Boeckeler W, Auer H, et al. Linguatula serrata tongue worm in human eye, Austria. Emerg Infect Dis. 2011;17:870–2.
London NJS, Rathinam SR, Cunningham ET. The epidemiology of uveitis in developing countries. Int Ophthalmol Clin. 2010;50:1.
Brisse M, Vrba SM, Kirk N, Liang Y, Ly H. Emerging concepts and technologies in vaccine development. Front Immunol [Internet] 2020;11. Available from: https://www.frontiersin.org/articles/10.3389/fimmu.2020.583077. Accessed 30 Jul 2023.
Micoli F, Bagnoli F, Rappuoli R, Serruto D. The role of vaccines in combatting antimicrobial resistance. Nat Rev Microbiol. 2021;19:287–302.
Willyard C. The slow roll-out of the world’s first malaria vaccine. Nature. 2022;612:S48–9.
Jain S, Venkataraman A, Wechsler ME, Peppas NA. Messenger RNA-based vaccines: past, present, and future directions in the context of the COVID-19 pandemic. Adv Drug Deliv Rev. 2021;179:114000.
Webster JP, Molyneux DH, Hotez PJ, Fenwick A. The contribution of mass drug administration to global health: past, present and future. Philos Trans R Soc B Biol Sci. 2014;369:20130434.
Boisson S, Wohlgemuth L, Yajima A, Peralta G, Obiageli N, Matendechero S, et al. Building on a decade of progress in water, sanitation and hygiene to control, eliminate and eradicate neglected tropical diseases. Trans R Soc Trop Med Hyg. 2021;115:185–7.
Wilson AL, Courtenay O, Kelly-Hope LA, Scott TW, Takken W, Torr SJ, et al. The importance of vector control for the control and elimination of vector-borne diseases. PLoS Negl Trop Dis. 2020;14:e0007831.
Baker RE, Mahmud AS, Miller IF, Rajeev M, Rasambainarivo F, Rice BL, et al. Infectious disease in an era of global change. Nat Rev Microbiol. 2022;20:193–205.
Meshkin RS, Armstrong GW, Hall NE, Rossin EJ, Hymowitz MB, Lorch AC. Effectiveness of a telemedicine program for triage and diagnosis of emergent ophthalmic conditions. Eye. 2023;37:325–31.
Iqbal U. Smartphone fundus photography: a narrative review. Int J Retin Vitr. 2021;7:44.
Tran K, Mendel TA, Holbrook KL, Yates PA. Construction of an inexpensive, hand-held fundus camera through modification of a consumer “Point-and-Shoot” camera. Investig Ophthalmol Vis Sci. 2012;53:7600–7.
Dolar-Szczasny J, Barańska A, Rejdak R. Evaluating the efficacy of teleophthalmology in delivering ophthalmic care to underserved populations: a literature review. J Clin Med. 2023;12:3161.
Howard, MacNeill C, Hughes AJ, Alqodmani F, Charlesworth L, Almeida K, et al. Learning to treat the climate emergency together: social tipping interventions by the health community. Lancet Planet Health. 2023;7:e251–64.
Judson SD, Rabinowitz PM. Zoonoses and global epidemics. Curr Opin Infect Dis. 2021;34:385–92.
Mora C, McKenzie T, Gaw IM, Dean JM, von Hammerstein H, Knudson TA, et al. Over half of known human pathogenic diseases can be aggravated by global warming. Nat Clim Change. 2022;12:869–75.
McGowan CR, Takahashi E, Romig L, Bertram K, Kadir A, Cummings R, et al. Community-based surveillance of infectious diseases: a systematic review of drivers of success. BMJ Glob Health. 2022;7:e009934.
Harris E. WHO introduces worldwide pathogen surveillance network. JAMA. 2023;329:2012.
Mwatondo A, Rahman-Shepherd A, Hollmann L, Chiossi S, Maina J, Kurup KK, et al. A global analysis of One Health Networks and the proliferation of One Health collaborations. Lancet. 2023;401:605–16.
Wong F, de la Fuente-Nunez C, Collins JJ. Leveraging artificial intelligence in the fight against infectious diseases. Science. 2023;381:164–70.
Han JH. Artificial intelligence in eye disease: recent developments, applications, and surveys. Diagnostics. 2022;12:1927.
Funding
JHK received funding from Sight for Souls (Bellevue, Washington, USA) and the Massachusetts Eye and Ear Global Surgery Programme (Boston, Massachusetts, USA).
Author information
Authors and Affiliations
Contributions
GC wrote this report. JHK and CP edited and contributed to the report.
Corresponding author
Ethics declarations
Competing interests
John H. Kempen: Betaliq (Equity Owner); Tarsier Pharma (Equity Owner). The remaining authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Clare, G., Kempen, J.H. & Pavésio, C. Infectious eye disease in the 21st century—an overview. Eye (2024). https://doi.org/10.1038/s41433-024-02966-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41433-024-02966-w