Abstract
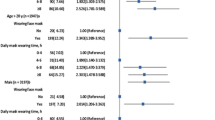
Mask-Associated Dry Eye (MADE) has emerged as a consequence of widespread face mask usage during the Covid-19 pandemic. This review critically assesses the available evidence. A comprehensive search on PUBMED and EMBASE was conducted to identify studies on MADE, which were then categorized based on their design. A total of 26 studies were critically appraised, with the majority exhibiting poor study design quality. Investigating the impact of mask use on ocular surface irritation faced challenges due to global mask mandates, pandemic-related behavioural changes, and a lack of validated methods to measure the response to mask wear. Among the 15 studies, 12 reported a statistically significant reduction in TBUT associated with mask wear; however, the median decrease of 1.3 s was considered clinically insignificant. Results from Schirmer’s test in 8 studies varied, with 5 studies reporting a decrease, contradicting the hypothesis of misdirected airflow. Out of 7 studies on corneal and conjunctival staining, 6 indicated a worsening associated with mask wear. Five studies investigating OSDI scores reported an increase following mask wear, but 3 studies repeated the survey too soon. Limited evidence suggests that masks may cause mild ocular surface irritation, but the quality and certainty of this evidence remain low. Methodological limitations were prevalent across the majority of studies, and the observed changes were minimal. Therefore, it is unlikely that significant ocular surface pathology will develop in the majority of mask wearers. Currently, there is insufficient data to support the establishment of a new syndrome.
摘要
口罩相关干眼症 (MADE) 是新冠肺炎大流行期间广泛使用口罩的后果。本综述批判性地评估了现有证据。
通过对PUBMED和EMBASE数据库的全面检索来确定对MADE的研究, 并根据其设计对其进行分类。
本研究共评估了26项研究, 其中大多数研究设计质量较差。由于全球佩戴口罩的要求、与疫情相关的行为改变以及缺乏有效方法测量佩戴口罩反应, 调查口罩使用对眼表刺激的影响面临挑战。在15项研究中, 12项报告显示与佩戴口罩相关的TBUT在统计学上减少; 然而, 中位数减少1.3秒在临床上是微不足道的。Schirmer在8项研究中试验的结果各不相同, 其中5项研究报告的结果与气流误导的假设相矛盾。在7项角膜和结膜染色的研究中, 6项显示了与佩戴口罩相关眼病的恶化。五项调查疫情后OSDI评分的研究报告称, 佩戴口罩后OSDI评分有所上升, 但有三项研究过早地重复了这项调查。
有限的证据表明, 口罩可能会引起轻微的眼表刺激, 但这一证据的质量和确定性仍然很低。在大多数研究中普遍存在方法学的局限性, 且观察到的变化微乎其微。因此, 大多数戴口罩的人不太可能出现明显的眼表病变。目前, 还没有足够的数据来支持一种新的综合征的命名。
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
White D. MADE: a new coronavirus-associated eye disease. Blog. 2020 [cited 2023 March]. Available from: www.healio.com/news/ophthalmology.
Moshirfar M, West WB, Marx DP. Face mask-associated ocular irritation and dryness. Ophthalmol Ther. 2020;9:397–400. https://doi.org/10.1007/s40123-020-00282-6.
Allsopp J, Basu MK, Browne RM, Burge PS, Matthews JB. Survey of the use of personal protective equipment and prevalence of work related symptoms among dental staff. Occup Environ Med. 1997;54:125–34. https://oem.bmj.com/lookup/doi/10.1136/oem.54.2.125.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. http://www.bmj.com/content/372/bmj.n71.abstract.
ROBINS-E Development Group (Higgins J, Morgan R, Rooney A, Taylor K, Thayer K, Silva R, et al. Risk Of Bias In Non-randomized Studies - of Exposure (ROBINS-E). Risk Of Bias In Non-randomized Studies - of Exposure (ROBINS-E). 2022. https://www.riskofbias.info/welcome/robins-e-tool.
Patel S, Blades K. The dry eye: a practical approach. 2003;1:1–88.
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo C-K, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017;15:276–83.
Jordan A, Baum J. Basic tear flow. Does it exist. Ophthalmology. 1980;87:920–30.
Serin D, Karsloğlu S, Kyan A, Alagöz G. A simple approach to the repeatability of the Schirmer test without anesthesia: eyes open or closed? Cornea. 2007;26:903–6.
Wright JC, Meger GE. A review of the Schirmer test for tear production. Arch Ophthalmol (Chic, Ill 1960). 1962;67:564–5.
Farrell J, Grierson DJ, Patel S, Sturrock RD. A classification for dry eyes following comparison of tear thinning time with Schirmer tear test. Acta Ophthalmol. 1992;70:357–60. https://doi.org/10.1111/j.1755-3768.1992.tb08579.x.
Lee JH, Hyun PM. The reproducibility of the Schirmer test. Korean J Ophthalmol. 1988;2:5–8. https://doi.org/10.3341/kjo.1988.2.1.5.
Marta A, Marques JH, Almeida D, José D, Sousa P, Barbosa I. Impact of COVID-19 pandemic on the ocular surface. World J Clin Cases. 2022;10:9619–27.
Schargus M, Zimzik EM, Fuhrmann L, Geerling G. Influence of short-term face mask wear on semiautomatically measured tear film parameters in dry eye patients and healthy volunteers. Graefe’s Arch Clin Exp Ophthalmol = Albr von Graefes Arch fur Klin und Exp Ophthalmol. 2023;261:1045–54.
D’Souza S, Vaidya T, Nair AP, Shetty R, Kumar NR, Bisht A, et al. Altered Ocular Surface Health Status and Tear Film Immune Profile Due to Prolonged Daily Mask Wear in Health Care Workers. Biomedicines. 2022;10:1160.
Shalaby HS, Eldesouky MEE. Effect of facemasks on the tear film during the COVID-19 pandemic. Eur J Ophthalmol. 2022;33:145–51. https://doi.org/10.1177/11206721221110010.
Aksoy M, Simsek M. Evaluation of ocular surface and dry eye symptoms in face mask users. Eye Contact Lens. 2021;47:555–8. https://journals.lww.com/claojournal/Fulltext/2021/10000/Evaluation_of_Ocular_Surface_and_Dry_Eye_Symptoms.5.aspx.
Mastropasqua L, Lanzini M, Brescia L, D’Aloisio R, Nubile M, Ciancaglini M, et al. Face mask-related ocular surface modifications during COVID-19 pandemic: a clinical, in vivo confocal microscopy, and immune-cytology study. Transl Vis Sci Technol. 2021;10:22 https://doi.org/10.1167/tvst.10.3.22.
Tatti F, Mangoni L, Pirodda S, Demarinis G, Iovino C, Siotto Pintor E, et al. Ocular surface changes associated with face masks in healthcare personnel during COVID-19 pandemic. Life. 2022;12:1431.
Bostanci Ceran B, Ozates S, Arifoglu HB, Tasindi E. Does facial mask use make our eyes dry? Change in tear meniscus measurements and conventional dry eye tests during facial mask use. Eur EYE Res. 2022;2:25–9. https://doi.org/10.14744/eer.2022.24633.
Nair S, Kaur M, Sah R, Titiyal JS. Impact of taping the upper mask edge on ocular surface stability and dry eye symptoms. Am J Ophthalmol. 2022;238:128–33.
Azzam SH, Nama A, Badarni H, Asael H, Dahoud WA, Mimouni M, et al. Assessment of dry eye disease in N95 versus surgical face mask wearers during COVID-19. Indian J Ophthalmol. 2022;70:995–9.
Esen Baris M, Guven Yilmaz S, Palamar M. Impact of prolonged face mask wearing on tear break-up time and dry eye symptoms in health care professionals. Int Ophthalmol. 2022;42:2141–4. https://doi.org/10.1007/s10792-022-02213-9.
Scalinci SZ, Pacella E, Battagliola ET. Prolonged face mask use might worsen dry eye symptoms. Indian J Ophthalmol. 2021;69:1508–1510. https://journals.lww.com/ijo/Fulltext/2021/06000/Prolonged_face_mask_use_might_worsen_dry_eye.32.aspx.
Jahanbani-Ardakani H, Hosseini M, Almasi S, Khalili MR. Letter to the Editor: Face mask–associated dry eye in health care professionals amid the COVID-19 pandemic. Optom Vis Sci. 2021;98:995–996. https://journals.lww.com/optvissci/Fulltext/2021/08000/Letter_to_the_Editor__Face_Mask_associated_Dry_Eye.18.aspx.
Krolo I, Blazeka M, Merdzo I, Vrtar I, Sabol I, Petric-Vickovic I. Mask-associated dry eye during COVID-19 pandemic-how face masks contribute to dry eye disease symptoms. Med Arch. 2021;75:144–8.
Giannaccare G, Vaccaro S, Mancini A, Scorcia V. Dry eye in the COVID-19 era: how the measures for controlling pandemic might harm ocular surface. Graefe’s Arch Clin Exp Ophthalmol. 2020;258:2567–8. https://doi.org/10.1007/s00417-020-04808-3.
Miller KL, Walt JG, Mink DR, Satram-Hoang S, Wilson SE, Perry HD, et al. Minimal clinically important difference for the ocular surface disease index. Arch Ophthalmol. 2010;128:94–101. https://doi.org/10.1001/archophthalmol.2009.356.
Motwani R, Janti SS, Ganji V, Mali KR, Yadav K, Patnaik N, et al. Face mask in COVID-19 and its association with dry eye disease: a cross-sectional study. Cureus. 2022;14:e32937.
Alsulami RA, Alotaibi R, Alsulami G, Alharbi R, Alamoudi R, Badeeb NO, et al. Effects of face-mask use on dry eye disease evaluated using self-reported ocular surface disease index scores: a cross-sectional study on nurses in Saudi Arabia. Cureus. 2022;14:e33071.
Itokawa T, Okajima Y, Iwashita H, Koji K, Suzuki T, Hori Y. Association between mask-associated dry eye (MADE) and corneal sensations. Sci Rep. 2023;13:1625.
Kapelushnik N, Benyosef S, Skaat A, Abdelkader A, Landau Prat D, Blum-Meirovitch S, et al. The effect of face masks during COVID-19 pandemic on ocular surface temperature––a clinical thermographic analysis. Diagnostics. 2022;12:1431.
Alanazi MA, El-Hiti GA, Al-Tamimi R, Bawazir AM, Almutleb ES, Fagehi R, et al. Assessment of the effect of wearing a surgical face mask on tear film in normal eye subjects. Meduri A, editor. J Ophthalmol. 2022;2022:2484997. https://doi.org/10.1155/2022/2484997.
Fan Q, Liang M, Kong W, Zhang W, Wang H, Chu J, et al. Wearing face masks and possibility for dry eye during the COVID-19 pandemic. Sci Rep. 2022;12:6214 https://doi.org/10.1038/s41598-022-07724-0. Available from
Harrison W, Pence N, Kovacich S. Anterior segment complications secondary to continuous positive airway pressure machine treatment in patients with obstructive sleep apnea. Optom - J Am Optom Assoc. 2007;78:352–5. https://www.sciencedirect.com/science/article/pii/S1529183907001169.
Chen X, Gallar J, Pozo MA, Baeza M, Belmonte C. CO2 stimulation of the cornea: a comparison between human sensation and nerve activity in polymodal nociceptive afferents of the cat. Eur J Neurosci. 1995;7:1154–63.
Prescott CR. Increased screen time and dry eye: another complication of COVID-19. Eye Contact Lens. 2021;47:433. https://journals.lww.com/claojournal/Fulltext/2021/08000/Increased_Screen_Time_and_Dry_Eye__Another.1.aspx.
Tangmonkongvoragul C, Chokesuwattanaskul S, Khankaeo C, Punyasevee R, Nakkara L, Moolsan S, et al. Prevalence of symptomatic dry eye disease with associated risk factors among medical students at Chiang Mai University due to increased screen time and stress during COVID-19 pandemic. PLoS One. 2022;17:e0265733 https://doi.org/10.1371/journal.pone.0265733.
Napoli PE, Nioi MFM. The “Quarantine Dry Eye”: The lockdown for Coronavirus disease 2019 and its implications for ocular surface health. Risk Manag Heal Policy. 2021;14:1629–36.
Neti N, Prabhasawat P, Chirapapaisan C, Ngowyutagon P. Provocation of dry eye disease symptoms during COVID-19 lockdown. Sci Rep. 2021;11:24434 https://doi.org/10.1038/s41598-021-03887-4.
Liao X, Wong ACC, Wong JOY, Jia R, Chen W, Wong HYM, et al. Investigating the Impact of COVID-19 Infection on Dry Eye Parameters. Diagnostics. 2023 ;13:1524.
Silkiss RZ, Paap MK, Ugradar S. Increased incidence of chalazion associated with face mask wear during the COVID-19 pandemic. Am J Ophthalmol Case Rep. United States; 2021; 22. 101032.
Patel SN, Mahmoudzadeh R, Salabati M, Soares RR, Hinkle J, Hsu J, et al. Bacterial dispersion associated with various patient face mask designs during simulated intravitreal injections. Am J Ophthalmol. 2021;223:178–83.
Acknowledgements
The authors would like to thank Mr Scott Hau for his expert opinion on in vivo confocal microscopy and immune cytology techniques.
Funding
Professor Bhuphendra Patel is supported in part by an Unrestricted Grant from Research to Prevent Blindness, Inc., New York, NY, to the Department of Ophthalmology & Visual Sciences, University of Utah. Mr Eoin O’ Sullivan has received honoraria from Roche and UCB. These are not associated with this work. No other sources of funding.
Author information
Authors and Affiliations
Contributions
RM was responsible for the conceptualisation of the study. EOS and BP contributed to the design of the study. MT was responsible for the data collection, analysis, quality assessment, writing and drafting. RM, EOS and BP were responsible for the ongoing editing, review, analysis and approval of the final manuscript of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Synopsis
This paper reviewed 26 studies on Mask-Associated Dry Eye (MADE) and concluded that although there is some evidence suggesting that masks may cause mild ocular surface irritation, the overall quality and certainty of this evidence is low.
Supplementary information
Rights and permissions
About this article
Cite this article
Teo, M.A.L., Sullivan, E.O., Patel, B.C.K. et al. Real or MADE-up: Investigating Mask-Associated Dry Eye (MADE) as an emerging syndrome. Eye 38, 1091–1096 (2024). https://doi.org/10.1038/s41433-023-02847-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02847-8