Abstract
Amblyopia is an important public health concern. While home-based screening may present an effective solution, this has not been rigorously assessed in a systematic review. A systematic review was performed using Ovid MEDLINE, PubMed, The Cochrane Library, Embase, Web of Science Core Collection, and Clinicaltrials.gov. All studies reporting the diagnostic accuracy of home-based screening tools for amblyopia among children were included. Studies involving orthoptist or ophthalmologist-led screening and adult subjects were excluded. The main outcome measure was the diagnostic accuracy expressed as sensitivity and specificity. Among 3670 studies identified, 28 were eligible for inclusion in our systematic review. The age range of patients were less than 1 month to 16 years old. 7 studies used internet-based tools, 16 used smartphone/tablet applications, 3 used digital cameras, and 3 used home-based questionnaires and visual acuity tools. All studies included a reference standard except one, which was a longitudinal study. 21 studies had full ophthalmological examination whilst 6 studies had validated visual acuity measurement tools as gold standards. Of the 27 studies which compared against a reference test, only 25 studies reported sensitivity and specificity values. Using the QUADAS-2 tool, 50% of studies were deemed to have applicability concern due to patient selection from tertiary centres and unclear methods for recruitment. There is a need to improve the quality of diagnostic accuracy studies, standardise thresholds for detecting amblyopia, and ensure consistent reporting of results. Further research is needed to evaluate the suitability of these tools for amblyopia screening.
摘要
弱视是一个重要的公共健康问题。虽然基于家庭的筛查可能是一个有效的解决方案, 但这还没有在系统性回顾中得到严格的评估。我们使用Ovid MEDLINE、Pubmed、The Cochrane Library、Embase、Web of Science Core Collection和Clinicaltrials.gov进行了系统综述。并纳入所有研究儿童弱视评估以家庭为基础的筛查方法诊断准确性的文章。涉及视力矫正医师或眼科医生主导的筛查和以成人受试者为对象的研究被排除在外。主要结果指标是敏感性和特异性表示的诊断准确性。在确定的3670项研究中, 有28项纳入系统回顾。患者的年龄范围在1个月至16岁之间。其中7项研究使用基于互联网的评估工具, 16项研究使用智能手机/平板电脑应用程序, 3项研究使用数码相机, 3项研究使用基于家庭的调查问卷和视力工具。除了一项纵向研究以外, 所有的研究均包含参考标准。21项研究进行了全面的眼科检查, 而6项研究将有效的视力测量工具作为黄金标准。在与参考测试进行比较的27项研究中, 只有25项研究报告了敏感度和特异性值。经QUADAS-2工具评估, 50%的研究被认为有适用性问题, 原因是病人来自三级中心和招募方法不明确。需要提高诊断准确性研究的质量, 对检测弱视的阈值进行标准化, 并确保结果报告的一致性。未来需要进一步的研究评估这些方法是否适合用于弱视筛查。
Similar content being viewed by others
Introduction
Amblyopia, or ‘lazy eye’, is associated with a lack of visual stimulation in the early years of life, resulting in cortical visual impairment [1]. This could be due to amblyogenic risk factors including uncorrected refractive error, astigmatism, media opacities, ptosis or other congenital pathologies that cause stimulus deprivation, and abnormal binocular interaction from strabismus [2,3,4]. This condition represents a significant public health concern, with population prevalence estimated between 2–5% [5,6,7].
Even though amblyopia is initially largely asymptomatic, untreated amblyopia resulting in vision loss could lead to problems at school, bullying, reduced quality of life, lifelong consequences on future occupation choices, and mental health issues [8, 9]. Contrary to the traditional notion that amblyopia treatment may be ineffective for children above 7 years old [10], the Paediatric Eye Disease Investigator Group (PEDIG) studies demonstrated that treatment of amblyopia may still be effective in children aged 7 to 17 years [11, 12], with the effectiveness of treatment becoming significantly reduced with time [13]. Hence, it is better to detect amblyopia early via screening.
Traditionally, vision screening for amblyopia was performed in the healthcare setting by experienced or trained healthcare professionals, including orthoptists, optometrists, and ophthalmologists, or by non-trained professionals in schools. Many programmes have not been successful due to inconsistencies in screening modalities utilised and lack of systematic assessment of their impact [14]. Overcoming barriers to these traditional amblyopia screening methods such as cost, limited access to healthcare and a limited number of qualified screeners is an ongoing issue [15]. With the COVID-19 pandemic and its related restrictions and lockdowns, traditional vision screening has become more difficult and the use of home-based screening tools for amblyopia are increasingly advocated, so that children do not miss out on opportunities for amblyopia screening [16, 17]. However, the role of home-based screening tools for amblyopia has not yet been rigorously assessed by a systematic review.
Here, we performed a systematic review to evaluate the accuracy and reliability of home-based amblyopia screening tools compared with the existing gold standard.
Methods
This systematic review was conducted in accordance with Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines [18]. The study was registered on PROSPERO (CRD42021233511) and the protocol is published in BMJ Open [19].
Eligibility criteria for studies in this review
Eligibility criteria were established prior to the conduct of this systematic review. All studies reporting diagnostic accuracies of home-based amblyopia screening tools among subjects less than 18 years old were included. Home-based screening tools included web or internet-based screening tools, mobile applications and other low-cost instruments such as digital cameras which could be used from home. All studies evaluating orthoptist or ophthalmologist-led screening, commercial photoscreeners, instruments incorporating artificial intelligence, autorefractors, and of adult subjects were excluded. Only Oxford Centre of Evidence Based Medicine (CEBM) level 4 evidence and above were included [20]. This includes case-series, cross-sectional studies, case-control studies, cohort studies, randomised controlled trials, and systematic reviews. All studies which did not report outcomes pertinent to the diagnostic accuracy of home-based amblyopia screening tools, such as studies reporting only validity or repeatability, epidemiological studies, case reports, expert reviews, opinion pieces, and conference abstracts without full publications, were excluded.
Information sources and search strategy
Electronic searches were performed through Ovid MEDLINE (1946 to present), PubMed, The Cochrane Library, Embase (1974 to present), Web of Science Core Collection (1970 to present), and Clinicaltrials.gov. Searches were conducted from inception until 31st August 2021. References of relevant studies were also searched and included if they met the inclusion criteria.
Medical subject heading (MeSH) terms such as ‘amblyopia’, ‘visual acuity’, ‘vision screening’ and terms to capture home-based screening tools such as ‘home’, ‘web’, ‘internet’ ‘app’, ‘smartphone’, and ‘mobile’ were used for the search where applicable. The full search strategy can be obtained via Online Supplementary Appendix 1. EndNote V.X9 (Thomson Reuters, New York, New York, USA) was used for data management. No date or language restrictions were stipulated.
Selection process
All studies went through a three-stage screening process involving title, abstract and full texts by two independent reviewers (SS, CS) according to the screening criteria available via Online Supplementary Appendix 2. Any disagreements were resolved with a third arbitrator (HJK). If there were any ambiguity on the screening tool, an email was sent to the first author of the paper to ask for more clarification before these studies were included. If there were missing data on specificity or sensitivity values, an email was also sent to the first author of the paper to acquire them. A reminder email was sent again if they did not respond after two weeks. If there was still no response after four weeks in total, those data were excluded from our analysis.
Data Collection
The main outcome measure reported was the diagnostic accuracy of home-based screening tools for amblyopia detection, expressed as sensitivity and specificity values.
Data was extracted from eligible studies using a tool adapted from the Cochrane Collaboration in the form of a table (Online Supplemental Appendix 3). Data collected included study design, number of included patients, duration of study, method of intervention used, index test, and reference standard where applicable. Data pertinent to the quality of diagnostic studies including investigators conducting test, subjects receiving test, method of interpretation of test, blinding of participants or investigators, and withdrawal rate of participants were also collected.
Risk of bias assessment
Risk of bias assessment was assessed using the QUADAS-2 tool for diagnostic accuracy studies (available via Online Supplementary Appendix 4) [21]. These judgments were made independently by two review authors (SS, CSC) and any disagreements resolved by the third arbitrator (HJK). Risk of bias and applicability concern were graded as low, unclear, or high.
Risk of bias and applicability concerns were graded for the following domains:
-
i.
Patient selection
-
ii.
Index test
-
iii.
Reference test
-
iv.
Flow and Timing
Summary measures
In addition to specificity and sensitivity values, confusion matrices (tables containing true positive, false positive, true negative, and false negative outcomes) were extracted from the included studies. Authors of papers that did not publish these values were contacted via email and given two weeks to respond. A reminder email was sent again if they did not respond after two weeks. If there was still no response after four weeks in total, those data were excluded from our analysis. If there were multiple thresholds used for amblyopia detection within the same study, or more than one sensitivity or specificity value were reported, the results will be reported based on the thresholds specified.
Patient and public involvement
There was no patient and public involvement during the conduct of this systematic review.
Results
Descriptive synthesis
The search was executed on 14 August 2021 and the screening was completed on 31 November 2021. Our search returned 3670 studies in total, of which 1021 were duplicates. Following title, abstract and full text screening, 28 studies were included in our systematic review (Fig. 1). The full list of excluded articles and reasons for exclusion is available on Online Supplementary Table 1. Among the home-based screening tools for amblyopia, there were seven internet-based tools measuring visual acuity [22,23,24,25,26,27,28], 16 mobile phone or iPad applications [29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44], three digital cameras; [45,46,47] whilst two studies used a combination of visual acuity charts and questionnaires [48, 49]. The included studies reported different forms of amblyogenic conditions including high refractive errors, astigmatism, ocular misalignment, and leukocoria. For these conditions except leukocoria, there are different criteria used as a cut-off point for amblyopia detection. Age of patients included in studies ranged from 0 to 16 years old.
*Reasons for exclusion were as follows: Wrong intervention (n = 28); conference abstracts, short article or pre-prints (n = 19); Tool does not qualify as home-based tool (n = 12); wrong population (n = 4); wrong outcomes (n = 4); no results available (n = 2). Online Supplementary Table 1 contains the full list of excluded studies with reasons.
All 28 studies included a reference standard except one longitudinal study, which compared facial photographs of patients with and without leukocoria. 22 studies had full ophthalmological examination whilst 6 studies had validated visual acuity measurement tools as their reference standard.
Of the 27 studies included, the sample size ranged from 70 to 36,973 patients, with a mean of 2004 patients. A summary of the studies included in the systematic review is presented in Table 1.
Sensitivity and specificity values were reported in 25 studies. Confusion matrices were included in 16 studies and can be assessed through Online Supplementary Table 2.
Risk of bias assessment
We used the QUADAS-2 tool in the systematic appraisal of all but one longitudinal study which did not include a reference standard or index test (Table 2) [39].
With regards to patient selection, 52% of included studies were shown to have high applicability concern. This was primarily due to patient selection from tertiary centres which were not representative of the normal population. A similar proportion showed unclear or high risk of bias in patient selection as the process was either unclear or non-systematic. Around a quarter of studies showed unclear or high risk of bias and applicability concern in index test used: 18.5% showed unclear or high risk of applicability concern in reference test used, whilst 33.3% showed unclear or high risk of bias in reference test used.
15% of studies were also shown to have a high risk of bias in flow and timing, as not all patients who went through the index test were subjected to the reference test or were lost to follow up.
Quantitative synthesis
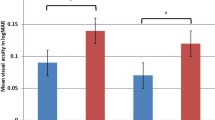
Specificity and sensitivity varied across studies with regards to the type of diagnostic tests used, country of study, patient selection and age of children included. Sensitivity estimates for internet-based tests ranged from 50.0% [22] to 93.8% [25] while specificity estimates ranged from 70.0% [27] to 98.9% [22]. Sensitivity estimates for mobile applications were between 15.4% [42] to 94.9% [34], while specificity estimates were between 63.0% [36] to 93.0% [38]. Digital camera as index test showed sensitivity estimates between 89.0% [46] to 94.6% [47] and specificity estimates between 82.9% [46] to 98% [45].
A meta-analysis could not be carried out as the studies were heterogenous in terms of type of screening tool used, differing cut-off values for amblyogenic conditions detected, population, reference standard used, and lack of raw data from confusion matrices. The heterogeneity of studies included is demonstrated in Fig. 2.
Discussion
Summary
To the best of our knowledge, this represents the first systematic review on the diagnostic accuracy of home-based amblyopia screening tools. Our systematic review revealed that there is a broad variety of home-based amblyopia screening tools available globally in the form of internet-based tests, mobile applications, digital cameras, and a combination of others. However, based on our rigorous assessment on the quality of studies included, there is an overall risk of bias in the existing studies. Lack of raw data pertinent for a pooled analysis, heterogeneity in the studies, and lack of standardisation on age-defining values for detecting amblyogenic conditions makes meaningful comparison of sensitivity and specificity estimates limited, which is crucial for the systematic appraisal of diagnostic accuracy studies [50].
Quality of evidence
Patient selection in around half of the studies demonstrated unclear or high risk of bias, either due to patient selection from tertiary centres, or non-systematic methods of recruitment. The paediatric clinic represents a population that could have a higher prevalence of amblyogenic risk factors. This may lead to overestimation of sensitivity values. Less than half of the studies showed unclear or high risk of bias in the index and reference test used. This is due to the lack of clarity on blinding during the conduct of the index test, or its interpretation which is not independent of the reference test, and the lack of uniformity in the reference test used across the studies. In studies that included full ophthalmological examination as their reference test, most included slit lamp and fundus examination by ophthalmologists, but not all specified whether retinoscopy, cover tests, or assessment of ocular motility were included. It was also difficult to standardise the visual acuity measurement tools used for studies that selected this as their reference standard, as the modality of tests would depend on the age of children recruited. In addition, there is lack of standardisation and international consensus on the age-defining values for detecting amblyogenic conditions such as high refractive errors, astigmatism, and ocular misalignment. Response bias was also present in studies that used a combination of screening tools, including questionnaires, as this depended on the response rate of the population involved [25, 48, 49].
Internet-based tests
Five studies published computer algorithm-generated standard visual acuity tests [22,23,24,25, 28], one study involved the use of video game (Eyespy) [26], and another study used computer generated checkboards of various frequencies for amblyopia detection [28]. Among these, only Longmuir et al. [23], Schlenker et al. [24], and Trivedi et al. [26] included lay screeners or parents in the conduct of the index test. The Jaeb Visual Acuity Screener (JVAS) [27], a free internet-based visual acuity screening test has been developed and validated for use among non-ophthalmic health professionals by the PEDIG group.
Mobile applications
The most common mobile application from the diagnostic accuracy studies included was GoCheck Kids (Gobiquity Mobile Health, Scottsdale, AZ, USA) [29,30,31, 35,36,37,38, 41, 44]. One of the advantages of mobile applications for screening is it can be used for younger children, such as the CRADLE app [39, 42] which is used on children as young as two months old to detect leukocoria. However, it demonstrated low sensitivity as it does not detect other amblyogenic risk factors with higher prevalence. In contrast, the GoCheck Kids app and Peek acuity app were used to detect high refractive errors and astigmatism, which were more common in the study population, hence reporting higher sensitivity values. The Eyeturn app [32] and Mhealth [38] were both used to detect ocular misalignment. Table 3 summarises the existing internet-based tests or mobile applications from our systematic review which has gone through validation studies and are free of charge.
Peek Acuity is the only app to date which had been shown through a cluster randomized controlled trial to increase follow-up rates through an integrated system involving the app [51].
Digital camera
There were only three studies that used digital camera for amblyopia screening. One incorporated a DV-S20 [45], and the other two utilised modified digital camera [46, 47]. However, the interpretation of the images was either by professionals or based on computer-generated analysis, and they tend to be more expensive than internet or mobile applications, making them less ideal as home-based screening tools.
Research in context
This systematic review is the first to publish a descriptive summary on the diagnostic accuracy of the latest available home-based amblyopia screening tools. There are parallels on the use of telemedicine rapidly in the COVID-19 era for the diagnosis and management of diabetic retinopathy, glaucoma, age-related macular degeneration, and for triage in emergency eye care [52]. Amblyopia detection to date has been largely undertaken by trained ophthalmic professionals. Even though the advent of photoscreeners such as the Plusoptix™, SPOT™, and autorefractors have enabled the screening process to be easier and less time-consuming, there is a lack of strong evidence on its cost-effectiveness for use in the community [53]. Home-based tools for amblyopia screening satisfies the WHO criteria for a good screening test [54]. Amblyopia has a pre-clinical phase that enables early detection and is a condition that can be treated. Home-based screening tools are easily available, less costly, or free of change, and reduce the dependence on trained ophthalmic professionals. Our systematic review showed that the sensitivity and specificity of some home-based tools to be comparable to photoscreeners or autorefractors [55]. As there has been a lot of research into the effectiveness of home-based tools for detection of amblyopia, this systematic review is important to summarise the existing evidence from literature in this field.
Strengths and limitations
This systematic review has highlighted key findings which may help pave the way for further research using home-based tools in amblyopia screening. The home-based tools included in this review are not restricted to the digital age, as questionnaires, digital cameras, and visual acuity charts used in the home setting are also included. Even though this systematic review included a comprehensive range of home-based tools in diagnostic accuracy studies, we did not include any studies reporting validity or reliability of home-based amblyopia screening tools or studies evaluating the cost-effectiveness of these tools. In addition, there is a possibility that other validated home-based tools are not captured in this systematic review if they have not been evaluated in diagnostic accuracy studies. Moreover, studies examining the feasibility of these tools by lay screeners were not included. Some of these internet-based tools or mobile applications may require some training before use, which may exclude some users.
Conclusions
This systematic review highlighted the availability of home-based screening tools, which could aid in amblyopia screening. However, there is a need to improve the quality and reporting of diagnostic accuracy studies using these tools. Home-based screening tools could be advantageous especially due to the COVID-19 pandemic, where amblyopia screening has stalled. Such tools may be a suitable option for low- and middle-income countries. However, as the incentive is upon the parents or lay screeners to utilise these resources, there is a need to educate the public on the importance of amblyopia screening at home, given the various options available for this. Ideally, evidence-based amblyopia screening tools could made be widely available for home-use, but further work is needed to identify the most effective tools for this purpose.
References
Levi DM. Rethinking amblyopia 2020. Vis Res. 2020;176:118–29.
Rahi JS, Logan S, Timms C, Russell-Eggitt I, Taylor D. Risk, causes, and outcomes of visual impairment after loss of vision in the non-amblyopic eye: a population-based study. Lancet. 2002;360:597–602.
Repka M, Simons K, Kraker R. Laterality of amblyopia. Am J Ophthalmol. 2010;150:270–4.
Shaw DE, Fielder AR, Minshull C, Rosenthal AR. Amblyopia – Factors influencing age of presentation. Lancet 1988;2:207–9.
Powell C, Hatt SR. Vision screening for amblyopia in childhood. Cochrane Database Syst Rev. 2009;8:CD005020 https://doi.org/10.1002/14651858.CD005020.pub3. PMID: 19588363
Friedman DA, Repka MX, Katz J, Giordano L, Ibironke J, Hawse P, et al. Prevalence of amblyopia and strabismus in White and African-American children aged 6 through 71 months: The Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116:2128–34.
Multi-Ethnic Paediatric Eye Disease Study Group. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months the multi-ethnic pediatric eye disease study. Ophthalmology. 2008;115:1229–36.
Jonas DE, Amick HR, Wallace IF, Feltner C, Schaaf EVB, Brown CL, et al. Vision screening in children aged 6 months to 5 years: evidence report and systematic review for the US Preventive Services Task Force. JAMA 2017;318:845–58.
Tandon AK, Velez FG, Isenberg SJ, Demer JL, Pineles SL. Binocular inhibition in strabismic patients is associated with diminished quality of life. J AAPOS. 2014;18:423–6.
Assaf AA. The sensitive period: transfer of fixation after occlusion for strabismic amblyopia. Br J Ophthalmol. 1982;66:64–70.
Scheiman MM, Hertle RW, Beck RW, Edwards AR, Birch E, Cotter SA, et al. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123:437–47.
Scheiman MM, Hertle RW, Kraker RT, Beck RW, Birch EE, Felius J, et al. Patching vs atropine to treat amblyopia in children aged 7 to 12 years: a randomized trial. Arch Ophthalmol. 2008;126:1634–42.
Holmes JM, Lazar EL, Melia BM, Astle WF, Dagi LR, Donahue SP, et al. Effect of age on response to amblyopia treatment in children. Arch Ophthalmol. 2011;129:1451–57.
Atowa UC, Wajuihian SO, Hansraj R. A review of paediatric vision screening protocols and guidelines. Int J Ophthalmol. 2019;12:1194.
Birch EE, Kelly KR, Wang J. Recent advances in screening and treatment for amblyopia. Ophthalmol Ther. 2021;10:815–30.
Painter S, Ramm L, Wadlow L, O’Connor M, Sond B. Parental home vision testing of children during Covid-19 pandemic. Br Ir Orthopt J. 2021;17:13–19.
Samanta A, Mauntana S, Barsi Z, Yarlagadda B, Nelson PC Is your vision blurry? A systematic review of home-based visual acuity for telemedicine. J Telemed Telecare. 2020 Nov:1357633X20970398. https://doi.org/10.1177/1357633X20970398.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647.
Sii S, Chean CS, Kuht HJ, Thomas MG, Rufai SR. Home-based screening tools for amblyopia: a systematic review protocol. BMJ Open. 2021;11:e051830.
OCEBM Levels of Evidence Working Group*. “The Oxford 2011 Levels of Evidence”. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653.
Whiting P, Rutjes A, Westwood M QUADAS-2: an updated quality assessment tool for diagnostic accuracy studies. In: Abstracts of the 19th Cochrane Colloquium; 2011. https://abstracts.cochrane.org/2011-madrid/quadas-2-updated-quality-assessment-tool-diagnostic-accuracy-studies (accessed 27 Feb 2011).
Briscoe D, Lifshitz T, Grotman M, Kushelevsky A, Vardi H, Weizman S, et al. A new computer program for mass screening of visual defects in preschool children. Br J Ophthalmol 1998;82:415–8.
Longmuir SQ, Pfeifer W, Shah SS, Olson R. Validity of a layperson-administered Web-based vision screening test. J AAPOS 2015;19:29–32.
Schlenker MB, Christakis TJ, Braga-Mele RM. Comparing a traditional single optotype visual acuity test with a computer-based visual acuity test for childhood amblyopia vision screening: a pilot study. Can J Ophthalmol 2010;45:368–74.
Thomson WD, Evans B. A new approach to vision screening in schools. Ophthalmic Physiol Opt 1999;19:196–209.
Trivedi RH, Wilson ME, Peterseim MM, Cole KB, Teed RG. A pilot study evaluating the use of EyeSpy video game software to perform vision screening in school-aged children. J AAPOS. 2010;14:311–6.
Yamada T, Hatt SR, Leske DA, Moke PS, Parrucci NL, Reese JJ, et al. A new computer-based pediatric vision-screening test. J AAPOS. 2015;19:157–62.
Qin YY, Liu ZZ, Zhu LY, Bao X, Luo FR, Liu YZ, et al. A computerized resolution visual acuity test in preschool and school-age children. Int J Ophthalmol 2020;13:284–91.
Arnold RW, Arnold AW, Hunt-Smith TT, Grendahl RL, Winkle RK. The positive predictive value of smartphone photoscreening in pediatric practices. J Pediatr Ophthalmol Strabismus. 2018;55:393–6.
Arnold RW, Armitage MD. Performance of four new photoscreeners on pediatric patients with high risk amblyopia. J Pediatr Ophthalmol Strabismus. 2014;51:46–52.
Arnold RW, O’Neil JW, Cooper KL, Silbert DI, Donahue SP. Evaluation of a smartphone photoscreening app to detect refractive amblyopia risk factors in children aged 1-6 years. Clin Ophthalmol. 2018;12:1533–7.
Cheng W, Lynn MH, Pundlik S, Almeida C, Luo G, Houston K. A smartphone ocular alignment measurement app in school screening for strabismus. BMC Ophthalmol 2021;21:150–w.
Di Foggia E, Stoll N, Meunier H, Rimelé A, Ance P, Moreau PH, et al. A new visual acuity test on touchpad for vision screening in children. Int J Ophthalmol 2020;13:1436–42.
Gupta R, Agrawal S, Srivastava RM, Singh V, Katiyar V. Smartphone photography for screening amblyogenic conditions in children. Indian J Ophthalmol 2019;67:1560–3.
Law MX, Pimentel MF, Oldenburg CE, de Alba Campomanes AG. Positive predictive value and screening performance of GoCheck Kids in a primary care university clinic. J AAPOS 2020;24:17.e1–17.e5.
Levitt AH, Martin SJ, Arnold RW. Performance of glow fixation GoCheck Kids and 2WIN photoscreeners and retinomax to uncover hyperopia. Clin Ophthalmol. 2020;14:2237–44.
Martin SJ, Htoo HE, Hser N, Arnold RW. Performance of two photoscreeners enhanced by protective cases. Clin Ophthalmol 2020;14:1427–35.
Mesquita MJ, Valente TL, de Almeida JD, Teixeira JA, Medina FM, Santos AM. A mhealth application for automated detection and diagnosis of strabismus. Int J Med Inform. 2021;153:104527.
Munson MC, Plewman DL, Baumer KM, Henning R, Zahler CT, Kietzman AT. Autonomous early detection of eye disease in childhood photographs. Sci Adv. 2019;5:eaax6363.
Nik Azis NN, Chew FLM, Rosland SF, Ramlee A, Che-Hamzah J. Parents’ performance using the AAPOS Vision Screening App to test visual acuity in Malaysian preschoolers. J AAPOS. 2019;23:268.e1–268.e6.
Peterseim MMW, Rhodes RS, Patel RN, Wilson ME, Edmondson LE, Logan SA. Effectiveness of the GoCheck kids vision screener in detecting amblyopia risk factors. Am J Ophthalmol. 2018;187:87–91.
Vagge A, Wangtiraumnuay N, Pellegrini M, Scotto R, Lester M, Traverso CE. Evaluation of a free public smartphone application to detect leukocoria in high-risk children aged 1 to 6 years. J Pediatr Ophthalmol Strabismus. 2019;56:229–32.
de Venecia B, Bradfield Y, Trane RM, Bareiro A, Scalamogna M. Validation of Peek Acuity application in pediatric screening programs in Paraguay. Int J Ophthalmol. 2018;11:1384–9.
Walker M, Duvall A, Daniels M, Doan M, Edmondson LE, Cheeseman EW, et al. Effectiveness of the iPhone GoCheck Kids smartphone vision screener in detecting amblyopia risk factors. J AAPOS. 2020;24:16.e1–16.e5.
Arnold RW, Arnold AW, Stark L, Arnold KK, Leman R, Armitage MD. Amblyopia detection by camera: Gateway to portable, inexpensive vision screening (calibration and validation of inexpensive, pocket-sized photoscreeners). Alsk Med. 2004;46:63–72.
Granet DB, Hoover A, Smith AR, Brown SI, Bartsch DU, Brody B. A new objective digital computerized vision screening system. J Pediatr Ophthalmol Strabismus. 1999;36:251–6.
Guo X, Jia X, Guo L, Xiao X, Shen H, Li S, et al. Comparison of computer-photoscreening with non-cycloplegic retinoscopy for amblyopiogenic risk factors in children. Chin Med J. 2000;113:1007–10.
Lan W, Zhao F, Li Z, Zeng J, Liu W, Lu J, et al. Validation and cost-effectiveness of a home-based screening system for amblyopia. Ophthalmology. 2012;119:1265–71.
Lim HT, Yu YS, Park SH, Ahn H, Kim S, Lee M, et al. The Seoul Metropolitan Preschool Vision Screening Programme: results from South Korea. Br J Ophthalmol. 2004;88:929–33.
Campbell J, Klugar M, Ding S, Carmody DP, Hakonsen SJ, Jadotte YT, et al. Diagnostic test accuracy. Int J Evid Based Health. 2015;13:154–62.
Rono HK, Bastawrous A, Macleod D, Wanjala E, Di Tanna GL, Weiss HA, et al. Smartphone-based screening for visual impairment in Kenyan school children: a cluster randomised controlled trial. Lancet Glob Health. 2018;6:e924–32.
Sommer AC, Blumenthal EZ. Telemedicine in ophthalmology in view of the emerging COVID-19 outbreak. Graefes Arch Clin Exp Ophthalmol 2020;258:2341–52. https://doi.org/10.1007/s00417-020-04879-2.
Horwood, A.M., Griffiths, H.J., Carlton, J. Mazzone P, Channa A, Nordmann M, et al. Scope and costs of autorefraction and photoscreening for childhood amblyopia—a systematic narrative review in relation to the EUSCREEN project data. Eye 2021;35,739–52.
Wilson JMG, Jungner G. Principles and practice of screening for disease. Public Health Paper Number 34. Geneva: WHO, 1968.
Sanchez I, Ortiz-Toquero S, Martin R, de Juan V. Advantages, limitations, and diagnostic accuracy of photoscreeners in early detection of amblyopia: a review. Clin Ophthalmol. 2016;10:1365–73. https://doi.org/10.2147/OPTH.S93714.
Silverstein E, Williams JS, Brown JR, Bylykbashi E, Stinnett SS. Teleophthalmology: Evaluation of phone-based visual acuity in a pediatric population. Am J Ophthalmol. 2021 Jan;221:199–206.
A. Bastawrous, H.K. Rono, I.A. Livingstone, Weiss HA, Jordan S, Kuper H, et al. Development and validation of a smartphone-based visual acuity test (peek acuity) for clinical practice and community-based fieldwork, JAMA Ophthalmol. 2015;133:930–937.
Zhao L, Stinnett SS, Prakalapakorn SG. Visual acuity assessment and vision screening using a novel smartphone application. J Pediatr. 2019;213:203–10.
Acknowledgements
We thank Selina Lock, Research Services Consultant at the University of Leicester David Wilson Library, for providing expert guidance in our systematic search strategy. We thank the authors of the included study who responded when contacted to provide more explanation and data from their publications.
Funding
SRR’s post is funded by a National Institute for Health and Care Research (NIHR) Doctoral Fellowship Award (NIHR300155). MGT’s post is funded by the NIHR (CL-2017-11-003). CB’s post is part funded/supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London. The views expressed are those of the authors and not necessarily those of The Institute of Cancer Research, the NHS, the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
SS: Design and conceptualisation of the study; major role in consolidating search strategies and screening criteria; acquisition, analysis, and interpretation of the data; drafted the manuscript for intellectual content. CSC: Acquisition of data; revised the manuscript for intellectual content. HK: Role as third arbitrator; revised the manuscript for intellectual content. CB: Analysis and interpretation of the data. MTG: Supervised design and conceptualisation of the study, revised the manuscript for intellectual content. SRR: Supervised design and conceptualisation of the study, consolidating search strategies and screening criteria, revised the manuscript for intellectual content.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sii, S.S.Z., Chean, C.S., Kuht, H. et al. Home-based screening tools for amblyopia: a systematic review. Eye 37, 2649–2658 (2023). https://doi.org/10.1038/s41433-023-02412-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02412-3