Abstract
Background
Growing evidence supports an individualised approach rather than radical surgery for conjunctival melanoma (CM). This study aimed to compare the long-term outcome between individualised and conventional exenteration techniques.
Methods
Our study retrospectively recruited advanced CM (clinical T3 stage) patients treated with individualised (13 cases) or conventional (18 cases) exenteration from June 2014 to April 2019. The individualised approach preserved at least three quadrants of the orbit, and the conventional procedures removed at least one third of the orbital tissues. The medical records were collected and analyzed during April 2020, including demographics, tumour characteristics, surgical details, postoperative rehabilitation and tumour-related prognosis.
Results
The tumour basal diameter was statistically (P = 0.011) larger in the conventional group (23.3 ± 7.6 mm) than in the individualised group (15.4 ± 6.3 mm). More tissues were preserved in the individualised group, resulting in a shorter duration of wound healing (2.1 ± 0.6 vs. 3.6 ± 2.0 weeks, P = 0.018) and less incidence of hollow appearance (15% vs. 72%, P = 0.003) than the conventional group. After follow-up for 39.3 ± 17.3 months, a comparison of survival curves showed no significant differences (P = 0.638) between the two groups. The 1- and 2-year overall survival rates were estimated as 100% and 80.0% in the individualised group, and 93.8% and 72.5% in the conventional group, respectively. Low or mixed pigmentation was identified as the risk factor for tumour-related mortality based on multivariate regression analysis.
Conclusions
The individualised approach to exenteration offers improved aesthetic results while still maximises the curable chance for advanced CM.
Similar content being viewed by others
Introduction
Conjunctival melanoma (CM), arising from atypical melanocytes in the basal layer of the conjunctival epithelium, is a rare but potentially life-threatening malignancy. The disease comprises 2% of all ocular tumours and 5% of eye melanomas [1]. The annual age-adjusted incidence per million population is 0.49 in non-Hispanic white, 0.33 in Hispanics, 0.18 in blacks, 0.17 in native Americans and 0.15 in Asians [2]. Based on Cancer Staging Manual (eighth edition) published by the American Joint Committee on Cancer, the staging system of CM contains a clinical T (cT) scale and a pathological T (pT) scale. Clinically advanced CM indicates local invasion of globe (cT3a), eyelid (cT3b), orbit (cT3c), lacrimal sac/nasolacrimal duct/paranasal sinuses (cT3d) or central nervous system (cT4). The 5-year mortality rate of advanced CM, estimated around 30.5–60.0%, is significantly higher than the locally circumscribed cases [3, 4].
Surgery is the first-line treatment for CM. Tumour excision with ‘no-touch’ technique is advocated for cT1 and cT2 staged CM, and orbital exenteration is recommended for cT3 staged CM [5]. According to the extent of resection, orbital exenteration can be further classified as total and subtotal approaches. Total exenteration removes the entire orbital contents, while subtotal exenteration preserves at least a quadrant of the orbit or the apical orbital tissues posterior to the globe [6]. Over the past decades, the surgical principle of CM shifted from radically extensive resection to a less invasive, more individualised approach. The safety surgical margin was initially secured at 5–7 mm but reduced to 2–3 mm during local excision [7, 8]. An eyelid-sparing exenteration technique is preferred rather than an eyelid-sacrificing technique, because the eyelid-sparing approach can achieve both favourable cosmetic outcome and acceptable tumour control [9, 10]. More and more surgeons embrace the concept that the surgical plan for exenteration should be tailored in each case to maximise the preserved tissues and to minimise the deforming effect [11]. A retrospective study provided evidence that the individualised subtotal exenteration offered improved aesthetic results than the total exenteration and still maximised the chance for surgical cure [6]. Nevertheless, few studies have compared the long-term outcome between the individualised and conventional subtotal exenteration techniques in advanced CM patients.
Subjects and methods
Patient recruitment
We retrospectively recruited consecutive cT3 staged CM cases who underwent subtotal exenteration from June 1 2014 to April 30 2019 at Fudan Eye & ENT Hospital. These cases were assigned into the individualised group and the conventional group based on exenteration techniques. The individualised approach customised the surgical margin based on tumour location and reconstructive options and preserved at least three quadrants of the orbital tissues [11]. The conventional procedures removed at least one third of the orbital tissues according to the surgical procedures of subtotal exenteration as previously described [9, 12]. The study protocol was in accordance with the Declaration of Helsinki, and informed consents were obtained from all patients.
Data collection
The medical records were reviewed, including demographics, tumour characteristics, TNM staging, pathologic margins, pre- and post-exenteration treatments, preserved tissues and rehabilitation. The follow-up data were collected during April 2020, including local recurrence, distant metastasis and tumour-related mortality. Time to recurrence, metastasis, and death was defined as the interval between the date of exenteration and the date of corresponding event.
Statistical analysis
Data were analysed with Statistical Product and Service Solutions. Student unpaired t test was used for continuous variables. Two-tailed χ2 test or Fisher exact test was used for categorical variables as appropriate. Cumulative survival rates were calculated by Kaplan-Meier curves and compared by log-rank test between different groups. Risk factors for tumour-related mortality were assessed using Cox proportional hazards regression model. A value of P < 0.05 was considered statistically significant.
Results
Clinical characteristics
Thirty-one patients were recruited in our study, including 13 cases in the individualised group and 18 cases in the conventional group. No significant differences were detected between the two groups regarding to the patient and tumour characteristics, except that the tumour basal diameter was statistically larger in the conventional group (23.3 ± 7.6 mm) than in the individualised group (15.4 ± 6.3 mm) (Table 1). In three cases, the pT stages were more advanced than the cT stages due to microscopic detection of orbit or lacrimal sac invasion.
Rehabilitation and cosmetics
More tissues were preserved in the individualised group (Fig. 1), resulting in shorter duration of wound healing and less incidence of hollow appearance than the conventional group (Table 2). In cases without volume replacement, 3 out of 5 patients (60%) in the individualised group achieved favourable cosmetic outcome, while only 1 patient (7%) in the conventional group was satisfied with the postoperative appearance (Fisher’s exact test, P = 0.037).
a–c A 59-year old male was referred for a 9-year history of recurrence after local excision of PAM on the left ocular surface 11 years ago. The multifocal lesions extended onto the limbus, bulbar conjunctiva, tarsal conjunctiva, caruncle and eyelids (cT3bN0M0). d The proposed skin incision was marked at 3 mm surgical margin. The preserved tissues included the upper and lower eyelid skin, the majority of middle orbit, and the entire posterior orbit. An orbital implant was placed for volume replacement. e, f The enhanced MRI scan at 2-year follow-up showed no tumour recurrence, no hollow appearance, and sufficient vascularisation of the orbital implant on both T1-weighted and T2-weighted images.
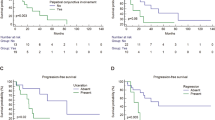
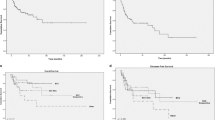
Recurrence, metastasis and mortality
Follow-up data were available for all patients with a mean duration of 39.3 ± 17.3 months (median 34.0, range 12–70), among which 25 cases (80.6%) have follow-up time for over 2 years and six cases (19.4%) for over 5 years. Local recurrence developed in two patients (15%) in the individualised group and two patients (11%) in the conventional group (one-tailed Fisher’s exact test, P = 0.566) with a mean recurrent time of 16.8 ± 10.9 months. Among them, one case in the conventional group reoccurred in the orbit due to positive surgical margin; the other three cases reoccurred in the nasolacrimal duct with no melanoma detected in the lacrimal sac during exenteration (Fig. 2). The local reginal control rate was estimated as 93.2% at 1 year, 88.8% at 2 years and 80.7% at 5 years.
a–d A 28-year old male noted diffuse, pigmented lesions of the left eye for 1 month. An incisional biopsy on the upper palpebral conjunctiva confirmed the diagnosis of CM (cT3bN0M0). The patient was then referred to our centre and treated with individualised subtotal exenteration. The lacrimal sac was removed during surgery, and histopathologic analysis revealed intraepithelial melanocytic proliferation without atypia in the lacrimal sac. e, f At 1-year follow-up, both physical palpation and enhanced MRI imaging showed no local recurrence at the lacrimal drainage system. g At 2-year follow-up, CT scan presented a nodular lesion at the nasolacrimal duct with extensive bony invasion. The recurrent lesion probably resulted from noncontiguous spread of floating melanoma cells during tear drainage.
Distant metastasis developed in four patients (31%) in the individualised group and seven patients (39%) in the conventional group (two-tailed Fisher’s exact test, P = 0.718) with a mean metastatic time of 19.4 ± 9.0 months (median 17.0, range 9–40). The metastasis-free survival rate was estimated as 89.5% (95% CI, 70.9–96.5%) at 1 year, 69.3% (95% CI, 47.6–83.5%) at 2 years, and 51.4% (95% CI, 28.1–70.5%) at 5 years. The overall survival rate was estimated as 96.6% (95% CI, 77.9–99.5%) at 1 year, 75.8% (95% CI, 53.8–88.4%) at 2 years, and 51.5% (95% CI, 26.1–71.4%) at 5 years. Comparison of the survival curves showed no significant differences between the individualised group and the conventional group (log-rank test, P = 0.638). The 1-, 2- and 5-year overall survival rate was 100%, 80.0% and 53.3% in the individualised group, and 93.8%, 72.5% and 50.8% in the conventional group, respectively.
Based on univariate Cox regression analyses, five variates were identified as the risk factors for mortality, including low or mixed pigmentation (P = 0.020), largest basal diameter ≥22 mm (P = 0.048), greatest tumour thickness diameter ≥5.5 mm (P = 0.045), advanced pathologic stage (pT3c/3d, P = 0.037), and previous recurrence (P = 0.009). After multivariate analysis, only one factor, low or mixed pigmentation (P = 0.048), remained to be predictive of tumour-related death (Table 3).
Discussion
Consistent with international assessment, there was slight preponderance of right eye involvement in our case series [1]. Male patients relatively predominated, and this propensity was reported in other Chinese case series but not in Indian or Caucasian studies [3, 4, 13,14,15]. Palpebral conjunctiva was mostly commonly involved in our study, while bulbar conjunctiva was considered as the most common site in previous studies [16]. This discrepancy of tumour location may be attributed to more advanced cT stages of our CM cases. Similarly, the discordance of cT stages between our and previous studies contributes to larger tumour diameter and greater tumour thickness in our series. Other clinical and oncologic characteristics, such as age, precancerous lesion, tumour epicentre location, tumour pigmentation and configuration, were comparable between our study and the other Caucasian and Asian reports [3, 4, 13,14,15,16]. Notably, we noticed incongruity between the cT and pT designations in three CM cases, indicating a potential pitfall of the cT scale that extensive CM may be overlooked while localised CM may be overrated under this staging system [17].
The principle goal of individualised exenteration is to completely remove tumours while maximise the preserved tissues. The surgical plan should take into account many factors, including tumour behaviour, anatomic location, local extension, and reconstructive options [6, 11]. In our case series, the tumour diameter was significantly smaller in the individualised group than the conventional group, suggesting that tumour size is an essential determinant of surgical plan. Based on our experience, we recommend small tumours with largest basal diameter <22 mm for the individualised approach to exenteration. During surgery, we prefer an eyelid-sparing technique with a surgical margin of 2–3 mm and always remove at least 5 mm of surrounding orbital tissues if possible. Follow-up results confirmed that this maximal tissue-preserving technique could achieve more rapid rehabilitation, more favourable cosmetic outcome and equally effective tumour control in comparison with the conventional exenteration. It is worth mentioning that tumour recurrence in the nasolacrimal duct occurred in both surgical groups even though the lacrimal sac was free of melanoma. This unique phenomenon of noncontiguous spread may be attributed to free‑floating melanoma cells in the tear film which implant in the lacrimal system during tear drainage (termed as ‘melanorrhea’) [18]. Therefore, some surgeons propose that both the lacrimal sac and the upper nasolacrimal duct should be intentionally removed during orbital exenteration [19].
The overall survival rates in our study, estimated as 75.8% at 2 years and 51.5% at 5 years, are relatively lower than previous reports. A retrospective study in Dutch evaluated 70 cases of CM (T1 = 54, T2 = 16), and the 2-year overall survival rate was calculated as 90% [14]. Similar result was published in an Indian study (T1 = 16, T2 = 14, T3 = 2), reporting that the 2-year overall survival rate was 89% [15]. A recent study of Chinese CM cases (T1 = 3, T2 = 25, T3 = 29) concluded that the 5-year overall survival rate was 69.5% [3]. Since advanced stages predict poor prognosis, we speculate that the relatively higher mortality rate in our study is associated with more pT3c and pT3d staged cases. According to an international study of CM, the 5-year overall survival rate was calculated as 50.0% for pT3c cases and 58.3% for all pT3 cases [1]. Another comparable study was conducted in Chinese CM patients, reporting that the 5-year survival was 40.0% for T3 cases [4]. Our study identified five risk factors for CM-related mortality, among which previous recurrence was also a risk factor in the conventional group. A growing evidence supports that local recurrence plays negative role in CM prognosis [20,21,22]. Moreover, a large Denmark study of 129 CM cases discovered that patients with incisional biopsy had higher risk of distant metastasis [5]. Although the choice of incisional biopsy still varies among surgical centres, most surgeons have reached consensus that a ‘no-touch technique’ should be used for local excision of circumscribed CM to ensure complete tumour removal [7, 8, 23, 24]. Many other factors have been proposed to predict poor prognosis, such as de novo arising, involvement of plica/caruncle, involvement of extralimbus conjunctiva, ulceration on tumour surface, positive surgical margin and so forth [3,4,5, 13,14,15,16,17, 20, 21]. However, these variables were not identified as risk factors in our case series. Thus, more studies are required to evaluate controversial variables in estimating unfavourable outcome in CM cases.
Pitfalls of our study stem from the retrospective design. For instance, sentinel lymph node biopsy may be beneficial for long-term survival, but these data are not available in our case series [25]. Proton radiation, small molecule inhibitors, and immune checkpoint inhibitors are novel treatments for CM, but none of our cases received these therapies [2, 26,27,28,29,30]. We anticipate well-designed prospective studies to investigate the long-term outcome of the above novel therapies. In addition, only 6 cases in the series have follow-up time of 5 years and therefore the 5-year survival rate is misleading. However, analysis of 1- and 2-year data, preoperative characteristics, tumour pathology, rehabilitation and aesthetic results was possible. To conclude, our study retrospectively recruited exenteration cases with cT3 staged CM, compared the clinical and prognostic data between individualised and conventional techniques, and provided evidence that the individualised approach can achieve both favourable prognosis and improved rehabilitative results.
Summary
What was known before
-
Orbital exenteration is the first-line treatment for advanced CM. The surgical principle has shifted from extensive resection to an individualised approach. Little is known about the long-term outcome of individualised exenteration.
What this study adds
-
The study retrospectively compared the long-term outcome between individualised and conventional exenteration for advanced CM. The study provided evidence that the individualised approach minimised the disfiguring effect and maximised the curable chance.
References
Jain P, Finger PT, Damato B, Coupland SE, Heimann H, Kenawy N, et al. Multicenter, International Assessment of the Eighth Edition of the American Joint Committee on Cancer Cancer Staging Manual for Conjunctival Melanoma. JAMA Ophthalmol. 2019. https://doi.org/10.1001/jamaophthalmol.2019.1640.
Grimes JM, Shah NV, Samie FH, Carvajal RD, Marr BP. Conjunctival melanoma: current treatments and future options. Am J Clin Dermatol. 2020. https://doi.org/10.1007/s40257-019-00500-3.
Zhou C, Wang Y, Jia R, Fan X. Conjunctival melanoma in chinese patients: local recurrence, metastasis, mortality, and comparisons with caucasian patients. Investig Ophthalmol Vis Sci. 2017;58:5452–9.
Sheng X, Li S, Chi Z, Si L, Cui C, Mao L, et al. Prognostic factors for conjunctival melanoma: a study in ethnic Chinese patients. Br J Ophthalmol. 2015;99:990–6.
Larsen AC. Conjunctival malignant melanoma in Denmark: epidemiology, treatment and prognosis with special emphasis on tumorigenesis and genetic profile. Acta Ophthalmol. 2016;94:842.
Goldberg RA, Kim JW, Shorr N. Orbital exenteration: results of an individualized approach. Ophthalmic Plast Reconstr Surg. 2003;19:229–36.
Shields JA, Shields CL, De Potter P. Surgical management of circumscribed conjunctival melanomas. Ophthalmic Plast Reconstr Surg. 1998;14:208–15.
Vora GK, Demirci H, Marr B, Mruthyunjaya P. Advances in the management of conjunctival melanoma. Surv Ophthalmol. 2017;62:26–42.
Shields JA, Shields CL, Demirci H, Honavar SG, Singh AD. Experience with eyelid-sparing orbital exenteration: the 2000 Tullos O. Coston Lecture. Ophthalmic Plast Reconstr Surg. 2001;17:355–61.
Günalp I, Gündüz K, Dürük K. Orbital exenteration: a review of 429 cases. Int Ophthalmol. 1996;19:177–84.
Ben Simon GJ, Schwarcz RM, Douglas R, Fiaschetti D, McCann JD, Goldberg RA. Orbital exenteration: one size does not fit all. Am J Ophthalmol. 2005;139:11–7.
Shore JW, Burks R, Leone CR Jr, McCord CD Jr. Dermis-fat graft for orbital reconstruction after subtotal exenteration. Am J Ophthalmol. 1986;102:228–36.
Martel A, Oberic A, Moulin A, Zografos L, Bellini L, Almairac F, et al. Orbital exenteration and conjunctival melanoma: a 14-year study at the Jules Gonin Eye Hospital. Eye. 2020. https://doi.org/10.1038/s41433-020-0767-6.
Brouwer NJ, Marinkovic M, van Duinen SG, Bleeker JC, Jager MJ, Luyten GPM. Treatment of conjunctival melanoma in a Dutch referral centre. Br J Ophthalmol. 2018;102:1277–82.
Kaliki S, Vasanthapuram VH1, Mishra DK. Conjunctival melanoma in Asian Indians: a study of 42 patients. Semin Ophthalmol. 2019;34:182–7.
Shields CL, Alset AE, Boal NS, Casey MG, Knapp AN, Sugarman JA, et al. Conjunctival tumors in 5002 cases. Comparative analysis of benign versus malignant counterparts. The 2016 James D. Allen lecture. Am J Ophthalmol. 2017;173:106–33.
Esmaeli B. Inclusion of histologic ulceration and tumor thickness in future American Joint Committee on cancer T category definitions for conjunctival melanoma. JAMA Ophthalmol. 2019. https://doi.org/10.1001/jamaophthalmol.2019.1656.
Rao R, Honavar SG, De Padua M, Mulay K, Reddy VP. Melanorrhea: Noncontiguous spread of palpebral conjunctival melanoma to the nasolacrimal duct. Indian J Ophthalmol. 2018;66:302–3.
Satchi K, McKelvie P, McNab AA. Malignant melanoma of the lacrimal drainage apparatus complicating conjunctival melanoma. Ophthalmic Plast Reconstr Surg. 2015;31:207–10.
Shields CL. Conjunctival melanoma: risk factors for recurrence, exenteration, metastasis, and death in 150 consecutive patients. Trans Am Ophthalmol Soc. 2000;98:471–92.
Aryasit O, Preechawai P, Hirunpat C, Horatanaruang O, Singha P. Factors related to survival outcomes following orbital exenteration: a retrospective, comparative, case series. BMC Ophthalmol. 2018;18:186.
Pacheco GE, Garcia-Onrubia L, Garcia-Alvarez C, Muñoz MF, Garcia-Lagarto E, Perez DM, et al. A retrospective review of conjunctival melanoma: presentation, treatment and evolution. Arch Soc Esp Oftalmol. 2019;94:218–24.
Cohen VML, O’Day RF. Management issues in conjunctival tumours: conjunctival melanoma and primary acquired melanosis. Ophthalmol Ther. 2019;8:501–10.
Shields JA, Shields CL, De Potter P. Surgical management of conjunctival tumors. The 1994 Lynn B. McMahan Lecture. Arch Ophthalmol. 1997;115:808–15.
Mor JM, Rokohl AC, Koch KR, Heindl LM. Sentinel lymph node biopsy in the management of conjunctival melanoma: current insights. Clin Ophthalmol. 2019;13:1297–302.
Finger PT, Pavlick AC. Checkpoint inhibition immunotherapy for advanced local and systemic conjunctival melanoma: a clinical case series. J Immunother Cancer. 2019;7:83.
Lami H, Epstein RJ, Cherepanoff S, Conway RM. Effective conservative management of locally advanced conjunctival melanoma using initial systemic therapy. Clin Exp Ophthalmol. 2020;48:402–4.
Thariat J, Salleron J, Maschi C, Fevrier E, Lassalle S, Gastaud L, et al. Oncologic and visual outcomes after postoperative proton therapy of localized conjunctival melanomas. Radiat Oncol. 2019;14:239.
Scholz SL, Hérault J, Stang A, Griewank KG, Meller D, Thariat J, et al. Proton radiotherapy in advanced malignant melanoma of the conjunctiva. Graefes Arch Clin Exp Ophthalmol. 2019;257:1309–18.
Kim JM, Weiss S, Sinard JH, Pointdujour-Lim R. Dabrafenib and trametinib for BRAF-mutated conjunctival melanoma. Ocul Oncol Pathol. 2020;6:35–8.
Acknowledgements
The authors thank Dr. Rui Zhang (Fudan Eye & ENT Hospital) and Dr. Yifei Yuan (Fudan Eye & ENT Hospital) for providing medical records of patients treated with conventional exenteration.
Funding
This work was supported by the National Natural Science Foundation of China [grant number 82000940, 81970835 and 81800867].
Author information
Authors and Affiliations
Contributions
RM and HR conceived and designed the study. RM, HR and XZ reviewed the medical records. XZ, LG, BX and JG analysed the data. HR and JQ supervised the study. RM and HR wrote the paper. All authors revised the final version of the paper. JQ is the principal investigator of this work and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, R., Ren, H., Zhou, X. et al. Orbital exenteration for conjunctival melanoma: comparison of long-term outcome between individualised and conventional techniques. Eye 35, 3410–3418 (2021). https://doi.org/10.1038/s41433-021-01454-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01454-9