Abstract
Purpose
To report the histopathological results of lacrimal gland biopsies over a 21-year period in a tertiary referral centre in the United Kingdom. To the best of our knowledge, this represents the largest series to be published in the United Kingdom.
Methods
A retrospective observational review was carried out for patients who underwent lacrimal gland biopsies in a tertiary referral centre at the University Hospitals of Leicester, United Kingdom between the years of 2000 and 2021.
Results
Lacrimal gland biopsies were performed on 248 patients during the specified 21-year period. They comprised 157 (63.3%) females and 91 (36.7%) males. The mean age at presentation was 50.8 years (range 15–94 years). The majority of patients were Caucasian (69.4%, n = 172) followed by Asians (25.0%, n = 62), African/Afro-Caribbean (4.8%, n = 12) and other ethnicities (0.8%, n = 2). The most common histopathological diagnosis was chronic inflammation dacryoadenitis (69.0%, n = 171) followed by lymphomas (15.3%, n = 38).
Conclusion
Our study shows that chronic inflammation accounts for the majority of histopathological diagnosis followed by lymphoproliferative disorders.
Similar content being viewed by others
Introduction
It was previously postulated that almost half of lacrimal gland lesions were of epithelial origin and the remaining were non-epithelial, based on figures derived from Reese’s 1956 clinico-pathologic survey of 112 consecutive expanding lesions of the lacrimal gland [1]. Furthermore, it found that one-half of the epithelial tumours were malignant, and a large proportion of the non-epithelial tumours were malignant lymphomas.
A clinico-pathologic review by Shields et al. in 1989 showed that the majority of lacrimal gland lesions arose from the non-epithelial part of the lacrimal gland and only 28% were of epithelial origin and contradicted the aforementioned results [2]. Historically, there has been a shortage of publications on lacrimal gland biopsies undertaken in the United Kingdom. This study reviewed all lacrimal gland lesions that were biopsied during a 21-year period in a tertiary referral centre, at the University Hospitals of Leicester, UK. We aim to provide factual data about the origin and frequency of lacrimal gland lesions within a diverse UK population.
Methods
A retrospective observational study of patients who underwent a diagnostic open sky approach lacrimal gland biopsy over a 21-year period from 2000 to 2021 was conducted. This included both incisional and excisional biopsies. Cases were identified from both our theatre and histopathology departmental electronic databases. Once identified, the medical records of the patients and their histological reports were obtained for analysis. Only intrinsic tumours of the lacrimal gland were included. Exclusion criteria included missing data in the case notes or incorrect patient details.
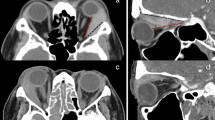
Data collected included socio-demographic variables, clinical symptoms and signs, and correlating imaging features. Tissue biopsy specimens were reviewed by a senior pathologist to confirm the histological diagnosis. In cases where there was a suspicion of lymphoproliferative disease or in cases of chronic inflammation, the specimens underwent further molecular genetic analysis including immune-phenotyping and gene rearrangement studies (Fig. 1).
Results
Lacrimal gland biopsies were performed on 248 patients during the specified 21-year period. They comprised 157 (63.3%) females and 91 (36.7%) males. The mean age at presentation was 50.8 years (range 15–94 years). Most patients were Caucasian (69.4%, n = 172) followed by Asians (25.0%, n = 62), African/Afro-Caribbean (4.8%, n = 12) and other ethnicities (0.8% n = 2).
Table 1 highlights a summary of the results that were found in this study. The most common histopathological diagnosis was specific or non-specific chronic inflammation (dacryoadenitis), which accounted for 69.0% of cases (n = 171), followed by lymphomas (15.3%, n = 38). There was no link identified between ethnicity and biopsy findings from our data.
Normal lacrimal gland was seen on histo-pathologic examination in two patients (0.8%) with prolapsed lacrimal glandular tissue. Seven biopsies (2.8%) showed lacrimal gland cysts with no dysplastic features.
Of the 171 patients reported to have dacryoadenitis on biopsy, 2 patients (1.2%) had evidence of small vessel vasculitis on histopathology and 4 patients (2.3%) had autoimmune Sjogren’s syndrome. One patient was diagnosed with granulomatosis with polyangiitis. Granulomatous inflammation secondary to sarcoidosis was seen in 7 patients (4.1%), and 1 patient (0.6%) was subsequently diagnosed with IgG4 disease. Two (1.2%) patients had an infective aetiology with a positive QuantiFERON® gold test indicative of tuberculosis.
Lymphomas accounted for 15.3% (n = 38) of all lacrimal gland biopsies performed. The mean age in the lymphoma group was older than the overall cohort as expected with a mean age of 66 years. Sixteen (42.1%) of lymphoma cases were male and 22 (57.9%) of cases were female. Extra-nodal marginal zone B cell lymphoma was diagnosed in 12 biopsies (31.6%), diffuse large B cell lymphoma in 9 cases (23.7%), mantle cell lymphoma in 7 cases (18.4%), follicular lymphoma in 6 cases (15.8%), and 4 cases (10.5%) had a diagnosis of unspecified lymphoma. One patient with B cell lymphoma had typical histopathological features of chronic lymphocytic leukaemia on subsequent analysis.
Of the lymphoma group, seven were initially diagnosed as inflammatory, but on further subsequent cellular analysis were confirmed as lymphomas. Nearly half of patients with a positive lacrimal lymphoproliferative result had evidence of systemic lymphoma concurrently or subsequent to the diagnosis of lacrimal gland lymphoma. With targeted treatment, five patients showed complete remission of their orbital and systemic disease.
Pleomorphic adenomas were detected in 2.0% (n = 5) of all biopsies and adenocarcinomas in 3.6% (n = 9). Of the adenocarcinoma group, two had high-grade carcinoma ex pleomorphic adenoma, two had adenoid cystic carcinomas, one had a primary lacrimal gland ductal carcinoma, one had a suspected metastasis from oesophageal carcinoma and the rest were unspecified. All the pleomorphic adenomas were suspected on clinical and imaging findings prior to surgery, and had planned excision biopsies.
Pre-operative computed tomography (CT) finding predictive of lymphoma on biopsy included moulding of lesion to orbital structures. Presence of globe and extra-ocular muscle displacement, especially of the superior and lateral recti muscles, were also noted to be predictors of lymphoma. No specific radiological finding was predictive of a histopathological diagnosis of dacryoadenitis.
Discussion
Lacrimal gland biopsies form an integral part in the diagnostic pathway of patients with lacrimal gland lesions. A normal lacrimal gland is composed of various cellular constituents, broadly classified into epithelial (glandular) and non-epithelial (non-glandular) components. Any of the cellular constituents within these components can give rise to various pathologies (Fig. 2).
Our study’s aim was to investigate the types of pathology that required an incisional or excisional lacrimal gland biopsy. Like other studies, it confirms that the majority of the biopsied specimens were of non-epithelial origin (see Table 2) [1,2,3,4,5,6,7,8,9,10,11,12].
The predominant lacrimal gland lesion, of non-epithelial origin, was found to be inflammation. Seven patients that were originally diagnosed with chronic inflammation were subsequently reclassified to lymphoma following molecular genetic analysis and immuno-phenotyping.
It is important to note that IgG4-related disease may have been reported as chronic non-specific dacryoadenitis in some of the earlier biopsies. In 2004, Kamisawa discovered that patients with autoimmune pancreatitis also showed the involvement of organs other than the pancreas [13]. In 2007, Cheuk et al. suggested that the previous chronic sclerosing dacryoadenitis may be part of the spectrum of IgG4-related sclerosing disease [14]. Although known by different names, there was international consensus and recommendation to unify the term IgG4-related disease followed by the organ or area affected (IgG4-related dacryoadenitis) [15].
Lacrimal gland enlargement was the most common presenting symptom in our study. Tamboli et al. [16] examined lacrimal gland size in 300 Caucasian orbits. They found that size decreases with age, and that there were no gender differences. They demonstrated that the mean (10th and 90th percentiles) lacrimal gland axial length in the right orbits were 14.7 mm (10.9 and 18.3 mm) and 14.5 mm (10.3 and 18.3 mm) in left orbits. Coronal length averaged 17.7 mm in right eyes (13.9 and 21.8 mm) and 16.9 mm (12.8 and 20.8 mm) in left eyes. These ranges can help in differentiating diseased versus non-diseased lacrimal glands, especially in conjunction with physical examination. CT and magnetic resonance imaging (MRI) features of lacrimal inflammation include moderate to intense enhancement, along with lacrimal gland enlargement and scleritis in idiopathic orbital inflammation [17].
The wedge sign, describing a triangle of tissue between the lateral rectus muscle and lateral orbital wall and the superior rectus muscle and the orbital roof, has been noted to be a prognostic feature in lacrimal gland inflammation, lacrimal gland carcinoma, or lymphoma [18].
One of the limitations of a study such as this in a tertiary centre may be due to the nature of referrals from surrounding areas. Referrals to tertiary centres may increase the proportion of epithelial tumours seen. In this study, all regional lacrimal gland biopsies are typically referred to our tertiary centre and hence this would be more representative of the population. This may also be an explanation for why a greater proportion of epithelial tumours may have been found in other studies.
In this study, over half of biopsies were reported as chronic inflammation with no cause attributed to this. As discussed earlier, IgG4-related dacryoadenitis is a recognised cause of chronic inflammation. In future studies, it would be interesting to assess what proportion of these chronic inflammatory biopsies could be attributed to IgG4-related disease with or without systemic involvement.
Equally, looking at the presence of other systemic autoimmune diseases in these cases would be useful to assess if this may be a predictor for chronic inflammatory dacryoadenitis.
Conclusion
Lacrimal gland biopsies may present a plethora of pathologies some of which may have grave implications; however, chronic inflammation remains the major pathological finding.
Summary
What was known before
-
Previous publications on lacrimal gland biopsies were equivocal in their findings of the proportion of epithelial versus non-epithelial origins.
What this study adds
-
Proportion of lesions of epithelial origin was found to be less than 10%.
-
Chronic inflammation accounted for the majority of biopsy results.
-
Extra-nodal marginal zone lymphoma was found to be the most frequent subtype of lymphoma identified.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Reese AB. The treatment of expanding lesions of the orbit with particular regard to those arising in the lacrimal gland; the seventh Arthur J. Bedell lecture. Am J Ophthalmol. 1956;41:3–11.
Shields CL, Shields JA, Eagle RC, Rathmell JP. Clinicopathologic review of 142 cases of lacrimal gland lesions. Ophthalmology. 1989;96:431–5.
Font RL, Smith SL, Bryan RG. Malignant epithelial tumors of the lacrimal gland: a clinicopathologic study of 21 cases. Arch Ophthalmol. 1998;116:613–6.
The Lacrimal Gland Tumour Study Group. An epidemiological survey of lacrimal fossa lesions in Japan: number of patients and their sex ratio by pathological diagnosis. Jpn J Ophthalmol. 2005;49:343–8.
Teo L, Seah LL, Choo CT, Chee SP, Chee E, Looi A. A survey of the histopathology of lacrimal gland lesions in a tertiary referral centre. Orbit. 2013;32:1–7.
Elbakary MA, Eldesouky MA, Sabik S, Shareef M. Lacrimal fossa lesions: a review of 146 cases in Egypt. Clin Ophthalmol. 2014;8:1603–9.
Ng DS, Chan E, Yau K, Chan CW. Clinicopathological survey of 23 patients with lacrimal fossa lesions in Hong Kong. Int J Ophthalmol. 2011;4:311–3.
Wright JE, Stewart WB, Krohel GB. Clinical presentation and management of lacrimal gland tumours. Br J Ophthalmol. 1979;63:600–6.
Tang SX, Lim RP, Al-Dahmash S, Blaydon SM, Cho RI, Choe CH, et al. Bilateral lacrimal gland disease. Ophthalmology. 2014;121:2040–6.e1–6e1.
Ahn C, Kang S, Sa H-S. Clinicopathologic features of biopsied lacrimal gland masses in 95 Korean patients. Graefe’s Arch Clin Exp Ophthalmol. 2019;257:1527–33.
Andrew NH, McNab AA, Selva D. Review of 268 lacrimal gland biopsies in an Australian cohort. Clin Exp Ophthalmol. 2014;43:5–11.
Von Holstein SL, Therkildsen MH, Prause JU, Stenman G, Siersma VD, Heegaard S. Lacrimal gland lesions in Denmark between 1974 and 2007. Acta Ophthalmol. 2012;91:349–54.
Kamisawa T. IgG4-positive plasma cells specifically infiltrate various organs in autoimmune pancreatitis. Pancreas. 2004;29:167–8.
Cheuk W, Yuen HK, Chan JK. Chronic sclerosing dacryoadenitis: part of the spectrum of IgG4-related sclerosing disease? Am J Surg Pathol. 2007;31:643–5.
Stone JH, Khosroshahi A, Deshpande V, Chan JK, Heathcote JG, Aalberse R, et al. Recommendations for the nomenclature of IgG4-related disease and its individual organ system manifestations. Arthritis Rheum. 2012;64:3061–7. https://doi.org/10.1002/art.34593.
Tamboli DA, Harris MA, Hogg JP, Realini T, Sivak-Callcott JA. Computed tomography dimensions of the lacrimal gland in normal Caucasian orbits. Ophthal Plast Reconstr Surg. 2011;27:453–6.
Vaidhyanath R, Kirke R, Brown L, Sampath R. Lacrimal fossa lesions: pictorial review of CT and MRI features. Orbit. 2008;27:410–8.
Lorenzano D, Rose GE. The “Wedge Sign”: an imaging sign for aggressive lacrimal gland disease. Ophthalmology. 2017;124:1081–3. https://doi.org/10.1016/j.ophtha.2017.03.004.
Author information
Authors and Affiliations
Contributions
SA was responsible for designing the study aims, methodology, collecting and analysing data, interpreting results, writing of paper and submission. EO was responsible for collecting and analysing data, interpreting results. MA was responsible for collecting and analysing data, interpreting results. HM was responsible for histopathological analysis and histopathology slides. JB was responsible for designing the study aims, methodology and editorial input. IDS was responsible for review of the paper and preparation of manuscript for submission following reviewers’ comments. RS was responsible for designing the study aims, methodology and editorial overview.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Awotesu, S., Obi, E., Awad, M. et al. Lacrimal gland biopsies—results from a tertiary centre in the UK. Eye 37, 983–987 (2023). https://doi.org/10.1038/s41433-022-02331-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02331-9
This article is cited by
-
Ocular oncology demystified
Eye (2023)