Abstract
Background
To investigate choroidal vascularity index (CVI) changes after oral eplerenone treatment in chronic central serous chorioretinopathy (cCSC) using the Spectral-domain (SD)-Optical Coherence Tomography (OCT) with enhanced depth imaging (EDI) mode.
Methods
Thirty-six eyes of 18 patients suffering from cCSC with monolateral foveal subretinal fluid (FSRF) successfully treated with oral eplerenone treatment and 18 age-matched healthy subjects were enroled in this retrospective study. EDI-OCT images obtained using Heidelberg Spectralis OCT device in patients with cCSC and FSRF (group 1); fellow eye (group 2) or healthy patients (healthy) were exported and then imported into image analysis ImageJ software for subsequent quantitative analysis. The main outcome measures were luminal area (LA) and CVI.
Results
A higher value of CVI was detected in group 1 compared to healthy eyes (p = 0.006). LA and CVI significantly reduced during follow up in group 1 and group 2. LA at 120 days was significantly lower compared to all previous time points both in group 1 and group 2 (p < 0.001). Median and [1st -3rd quartile] CVI values were 0.8 [0.7; 1.1] at baseline, 0.8 [0.7; 0.9] at 30 days; 0.7 [0.6; 0.9] at 60 and 90 days and 0.6 [0.5; 0.8] at 120 days in group 1 (p = 0.007) and 0.7 [0.6; 0.9] at baseline, 0.7 [0.7; 0.8] at 30 days; 0.7 [0.6; 0.7] at 60 and 90 days and 0.6 [0.6; 0.7] at 120 days in group 2 (p = 0.018).
Conclusions
Choroidal vascularity index reduced in cCSC patients after oral eplerenone treatment during follow up both in eyes with SRF and fellow eyes thus demonstrating the effectiveness of mineral corticoid receptor antagonists in recovering choroidal morphology.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSC), first described by Von Graefe in 1866, is a retinal disease characterized by serous localized neurosensory retinal detachment and pigment epithelial detachment (PED). Although underestimated, CSC annual reported incidence is about 1:1000, mostly affecting young men, with a 6:1 male to female ratio [1]. Risk factors include “type- A” personality cluster, sympathetic-parasympathetic imbalance, pregnancy, stress and previous oral corticosteroid medications [2, 3]. CSC is a pachychoroid-spectrum disease with dilated choroidal vessels in Haller’s layer and thinning of the choriocapillaris and Sattler’s layer [4]. Dilated and hyperpermeable choroidal vessels with increased hydrostatic pressure, may cause focal Bruch’s membrane and retinal pigment epithelial (RPE) disruption that could lead to a serous retinal detachment. Based on the clinical presentation, CSC includes two different entities, the acute form with a usually spontaneous resolution within four/six months, and the chronic form (cCSC), previously known as “diffuse retinal epiteliopathy”, characterized by persistent subretinal fluid (SRF) with consequent neurosensory retinal atrophic changes and widespread RPE alterations. Zhao et al. were the first to observe a possible link between CSC disease and mineralcorticoids receptor (MR) activity and a MR overstimulation of choroidal vessels has been proposed as a cause of choroid hyperpermeability [5]. Approved by US FOOD and Drug Administration for different systemic conditions, Eplerenone is a mineralcorticoid specific receptor antagonist which has widely been used in acute and cCSC showing good efficacy, with retinal and choroidal anatomical recovery and consequent visual acuity improvement [6,7,8].
A randomised, placebo-controlled trial, assessing the efficacy and safety of eplerenone for treating patients with CSCR, found no evidence of a clinically important benefit after treatment. Indeed, they did not report any significant difference between groups in favour of eplerenone treatment in terms of central subfield retinal thickness, resolution of SRF or recurrence. However, many bias have been observed and some comments and replies to the authors have been subsequently published. Particularly, given that more patients in the placebo group were given PDT than in the eplerenone group, the inability to control the use of co-treatment has undoubtedly introduced some bias, as well as the fact of possible erroneous inclusion of eyes with choroidal neovascularization. The latter can be underestimated by conventional dye tests if compared with optical coherence tomography angiography which was not used in this study, as it is known they respond poorly to eplerenone [9,10,11].
Following oral eplerenone treatment, a reduction of subfoveal choroidal thickness associated with SRF resolution has been observed by several authors [6, 12].
Choroidal vascularity index (CVI) is a quantitative parameter which can help the assessment of choroidal vasculature in eyes with CSC using optical coherence tomography (OCT). The term refers to the ratio of the luminal area to the cross-sectional choroidal area [13]. CVI alteration may be representative for choroidal vasculature impairment and therefore may play a central role in monitoring the disease progression, patient follow-up and response to the therapy. Whereas recent reports have studied post- PDT choroidal alterations by focusing on the decrease of subfoveal choroidal thickness [14, 15], CVI may better describe the choriocapillaris and choroidal response [16, 17]. Iovino et al reported a reduced Luminal choroidal area (LCA) and total choroidal area (TCA) after PDT treatment. Hence, CVI alterations did not reach significance in their study [18]. Differently, by analysing 22 eyes, Izumi et al noted a decrease of SCFT, TCA, LCA and CVI 3 months after PDT [16]. Van Rijssen et al, did not report in their study a significantly reduced CVI after half-dose PDT or subthreshold micropulse laser (HSML) [19], whilst a decrease in SFCT and CVI was noted by Kwak et al in patients treated with oral carbonic anhydrase inhibitor [20]. The aim of our retrospective study was to assess choroidal changes interpreted as CVI alterations in eyes with cCSC and monolateral subfoveal SRF successfully treated with oral eplerenone, compared with fellow eyes and age-matched healthy controls.
Materials and methods
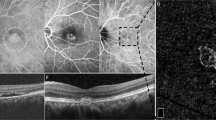
A total of 36 eyes of 18 patients were analysed in this retrospective observational study. In this retrospective study patients with cCSC and unilateral persistent foveal SRF longer than 4 months, successfully treated with oral eplerenone with complete resolution of subfoveal SRF during a 4-month follow up study were enroled at the University G. d’Annunzio, Chieti- Pescara, Italy for a retrospective assessment of anatomical changes during therapy. Patients with a diagnosis of other chorioretinal diseases, use of steroid systemically, systemic contraindications for antagonist of mineralcorticoid receptor treatment, previous surgical treatments within previous 12 months (including intravitreal anti-vascular endothelial growth factor or steroid injections) or photodynamic therapy (PDT) were excluded. CCSC was interpreted as the presence of non-resolving SRF with foveal involvement longer than four months evidenced at the ophtalmoscopic clinical evaluation and instrumental evaluation (multicolour imaging, FAF, FA, ICGA and SD OCT). A successful treatment was defined by the complete SRF reabsorption at both clinical and instrumental assessment. Administered treatment consisted of 25 mg of oral Eplerenone during the first week of treatment, and then 50 mg for the following weeks. The retrospective study included CSC eyes with foveal SRF (group 1; n = 18), fellow eyes healthy or with CSC without foveal SRF (group 2; n = 18); and controls eyes of healthy aged-matched subjects (group 3; n = 18). All patients received complete ophthalmologic examination, including best corrected visual acuity in LogMar measurements (BCVA), anterior segment biomicroscopy, intraocular pressure assessment (IOP), indirect fundus examination, multicolour imaging, and SD OCT. All evaluation were performed at baseline, 15 days and then monthly until SRF reabsorption. Choroidal evaluation was performed through SD-OCT imaging (Spectralis OCT, Heidelberg Engineering, Inc, Germany) with EDI- mode, obtaining a horizontal single line scan involving the fovea. Images with poor signal strength (<25) were excluded and thus repeated. CVI parameter was obtained through the application of a validated algorithm [17, 21, 22]: manual identification of the choroid was performed, defined as the area between the outer border of the RPE and the sclera and therefore known as total choroidal area (TCA). Images were binarized through “Niblack’s Auto Local threshold”, dark pixels were defined as the luminal area (LA) and light pixels were defined as stromal area (SA) [23]. CVI percentage (%) was obtained by dividing LA for TCA. CVI evaluation was performed at baseline, 15, 30, 60, 90, 120 days.
Statistical analysis
Quantitative variables were reported as median and Interquartile range (IQR) while quantitative data were summarized as frequency and percentage. Departures from normal distribution were evaluated for each variable using a Shapiro-Wilk’s test. To test for baseline differences between the experimental groups (group 1 and group 2) and healthy control different linear mixed models were applied. Linear mixed models allow explicit modelling of the within- and between-patient variation in the outcome while taking into account that each measurement is not independent from the other since are from both eyes within the same individual. Post-hoc analyses tested for statistically significant difference between groups. Bonferroni adjustment was applied to post-hoc analyses p values. Friedman test was used to assessed within groups differences. All statistical tests were twosided, with a significance level set at p < 0.05. Analyses were performed using the R software environment for statistical computing and graphics (version 3.4.1; http://www.r-project.org/).
Results
Figure 1 shows the boxplots of each group compared to healthy controls at baseline for LA and CVI and the adjust p values result from multiple comparisons showing a higher value of CVI in group 1 compared to healthy eyes. Table 1 reports median value [1st -3rd quartile] of LA and CVI of group 1 and group 2 at each time point. LA at 120 days was significantly lower compared to all previous time points both in group 1 and group 2 (p < 0.001). Median and [1st -3rd quartile] CVI values were 0.8 [0.7; 1.1] at baseline, 0.8 [0.7; 0.9] at 30 days; 0.7 [0.6; 0.9] at 60 and 90 days and 0.6 [0.5; 0.8] at 120 days in group 1 (p = 0.007) and 0.7 [0.6; 0.9] at baseline, 0.7 [0.7; 0.8] at 30 days; 0.7 [0.6; 0.7] at 60 and 90 days and 0.6 [0.6; 0.7] at 120 days in group 2 (p = 0.018). [Fig. 2].
Discussion
The use of MR antagonists has been justified by fundamental studies that showed that both vascular endothelial cells of the choroid and the retinal pigment epithelial cells express the MR [24, 25] and that overactivation of MR by either ligand excess or hyperexpression of human MR in transgenic model, induced choroidal pathology close to pachychoroid features [26]. Moreover, choroidal vascular blood flow has been reported to be under autonomous nervous system control [27] and several studies have shown that MR antagonists are able to regulate the autonomous nervous dysfunction in the heart, thus explaining in part their beneficial cardiac effects. In addition to this, the effect of MR antagonists on choroid vasculature has been further validated by an interesting study evaluating perfusion choroidal changes after isometric exercise in patients with chronic central serous chorioretinopathy nontreated or treated with mineralocorticoid receptor antagonists, underlining that only in the treated group a significant reduction of choroidal blood flow velocity and volume [28].
In our previous article we observed a restoration of retinal and choroidal morphology in eyes affected by cCSC treated with Eplerenone, with complete resolution of foveal SRF in all cases, at 60 days in 71.4% of treated eyes and within 120 days in the remaining 28.6%. Further, we demonstrated a significant improvement of BCVA and a decrease of central macular thickness (CMT), SRF and subfoveal choroidal thickness (SFCT), which significantly reduced at the OCT examination from 452.85 ± 132.74 micron at baseline to 386.85 ± 130.69 micron at 30 days, 354.85 ± 97.88 micron at 60 days, 358.57 ± 93.47 micron at 90 days and 358.28 ± 93.33 micron at 120 days. Interestingly, in our patients, there was no difference in SFCT at baseline between the affected and the fellow eye, however, as a result of treatment, the unaffected eye showed decreased SFCT as well [6]. Maruko et al. reported in his study the increased SFCT in the unaffected fellow eye to be a risk factor for retinal detachment, thus the systematic treatment with Eplerenone lowers this risk of retinal detachment [29]. Similarly, Sacconi et al observed complete resolution of SRF at the OCT-A at 13 weeks follow-up after Eplerenone treatment in more than 80% of eyes with cCSC without CNV (81% of complete resolution, 9.5% of partial resolution, and 9.5% of absence of response) whereas no patients with CNV at the OCT-A had complete resolution, 50% had partial response, and 50% had no response, assuming CNV as a possible unfavourable predictive biomarker of response to Eplerenone treatment. In their study, mean SFCT reduced from 432 ± 79 micron at baseline to 419 ± 76 micron at the end of treatment (13 weeks follow-up) and no difference was noted in SFCT between patients with complete response to treatment and without response [30]. The increased choroidal thickness frequently observed in the affected eyes has been intended as a result of choroidal hyperpermeability [31,32,33]. Indeed, vascular changes in CSC had already been assessed in literature [34], thus, the necessity of a tool able to evaluate choroidal vascular modifications. OCT has proven to be a valid device to analyse choroidal changes in different conditions (myopia, diabetes, CSC) [32]. CVI is a novel parameter first described by Agrawal [35] for the assessment of choroidal vascular pattern at the OCT examination, by studying the vascular ratio of the luminal area to the choroidal area. It is representative of the choroid in both its vascular and stromal factor, giving new additional structural information when compared to the choroidal thickness frequently reported in several studies. To date, different studies have analysed the choroidal features in order to assess and follow up the course and response to treatment with different devices including OCT, OCT-A [35,36,37] and enhanced depth imaging (EDI) OCT, whose introduction has allowed more detailed non invasive quantitative and qualitative choroid evaluation. Differently from choroidal thickness assessment, CVI has shown not to be influenced by systematic and local factor (age, systemic blood and intraocular pressure, axial length) [35]. This aspect makes CVI a good biomarker, previously chosen for different studies. Choroidal vascular index modifications have been investigated in cCSC patients after different treatments. Van Rijssen [20] and Park [38] as well described choroidal alterations after PDT treatment in eyes with chronic CSC, achieving different results. The former did not find a statistically significant reduction in CVI after half dose PDT in his study, whilst the latter reported an important reduction in CVI after half or full dose PDT. However, the different result may be attributed to differences in the two studies: Park included both acute CSC and cCSC patients establishing a 3-month follow up, whereas Van Rijssen only enroled patients with a diagnosis of cCSC with a follow-up of 8 months. Moreover, PDT may affect choriocapillaris vascular remodelling and permeability, however the luminal density to the total choroidal area (the so called CVI) may not be significantly influenced. Differently, in Van Rijssen study, SFCT decreased after half dose PDT in the treated eyes, whereas no significant change was observed in the unaffected eye. Similarly, Agrawal et al found in their retrospective study significant differences in CVI and SFCT in eyes with acute CSC compared to healthy fellow eyes (+3.12 and +73.03, respectively) and age-matched healthy eyes (+5.32 and + 196.13, respectively). Interestingly, no statistically significant difference in SFCT between acute and resolved CSC was found, (+ 27, P = 0.48) differently from CVI which was significantly higher in eyes with acute CSC ( + 5.10, P < 0.0001), probably due to the increased vascular component (LA) during the acute phase of CSC, leading to the increase in SFCT and CVI. In this study we aimed at reporting choroidal changes assessed evaluating CVI in eyes with cCSC and monolateral foveal SRF successfully treated with oral eplerenone with complete SRF resolution during a 4-month follow up compared to fellow eyes without SRF. CVI of both groups was also compared with healthy age-matched eyes at baseline. We demonstrated a significant reduction of LA and CVI during time (p < 0.001; p < 0.007) in cCSC eyes and in the fellow eyes (p < 0.001; p = 0.018). At baseline CVI and LA were significantly higher in cCSC eyes compared to healthy eyes (p = 0.056; p = 0.006). Hence, our speculation is that CVI gives a good representation of the vascular pattern and vascular modifications that occur when the choroid is affected by CSC and therefore is able to follow-up the efficacy of eplerenone in treating cCSC, being a good biomarker of therapy. The main limitations of our study are its retrospective nature and the small number of patients enroled in the present analysis. However, the strength of our study is the CVI change analysis conducted in a prospective manner and the evaluation of the efficacy of the Eplerenone by analysing CVI. Our study describes changes in choroidal vascularity in eyes with CSCR treated with oral eplerenone and fellow eyes through the study of LA and CVI, supporting the use of CVI as a non-invasive biomarker that may be useful as an index for early diagnosis, follow up and response to therapy. Choroidal vascular index reduced in cCSC patients after oral eplerenone treatment, proving the efficacy of mineral corticoid receptor antagonists in recovering choroidal morphology. Since MR antagonists act also on extracellular matrix remodelling, such treatment should be taken on the long term to observe their complete beneficial effect on ocular structure [39]. The use of CVI as a biomarker may further increase our knowledges on the physiopatological processes happening in the vascular pattern in cCSC in order to propose new therapeutic strategies. Further prospective studies with a larger sample of chronic CSC are requested to better understand functional and anatomical choroidal changes induced by mineralcorticoid receptor antagonists in order to propose new effective treatment modalities.
Summary
What was known before
-
Choroidal vascular index reduced in cCSC patients after oral eplerenone treatment, proving the efficacy of mineral corticoid receptor antagonists in recovering choroidal morphology.
What this study adds
-
The use of choroidal vascular index as a biomarker may further increase our knowledges on the physiopatological processes happening in the vascular pattern in cCSC in order to propose new therapeutic strategies.
Data availability
The data that support the findings of this study are available on request from the corresponding author, [RDA].
References
Kitzmann AS, Pulido JS, Diehl NN, Hodge DO, Burkel JP. The incidence of central serous chorioretinopathy in Olmsted County, Minnesota, 1980-2002. Ophthalmol. 2008;115:169–73.
Wong KH, Lau KP, Chhablani J, Tao Y, Li Q, Wong IY. Central serous chorioretinopathy: what we have learnt so far. Acta Ophtalmol. 2016;94:321–5.
Daruich A, Matet A, Dirani A, Gallice M, Nicholson L, Sivaprasad S, et al. Oral mineralocorticoid-receptor antagonists: real-life experience in clinical subtypes of nonresolving central serous chorioretinopathy with chronic epitheliopathy. Transl Vis Sci Technol. 2016;5:2.
Cheung CMG, Lee WK, Koizumi H, Dansingani K, Lai TYY, Freund KB. Pachychoroid disease. Eye(Lond). 2019;33:14–33.
Zhao M, Célérier I, Bousquet E, Jeanny JC, Jonet L, Savoldelli M, et al. Mineralocorticoid receptor is involved in rat and human ocular chorioretinopathy. J Clin Invest. 2012;122:2672–9.
Toto L, D’Aloisio R, Mastropasqua R, Di Antonio L, Di Nicola M, Di Martino G, et al. Anatomical and functional changes of the retina and the choroid after resolved chronic CSCR. J Clin Med. 2019;7;8:474.
Iacono P, Toto L, Eliana C, Varano M, Parravano MC. Pharmacotherapy of central serous chorioretinopathy: review of the current treatments. Curr Pharm Des. 2018;24:4864–73.
Lotery A, Sivaprasad S, O’ Connell A, Harris RA, Culliford L, Ellis L, et al. Eplerenone for chronic central serous chorioretinopathy in patients with active, previously untreated disease for more than 4 months (VICI): a randomised, double-blind, placebo-controlled trial. Lancet. 2020;395:294–303.
Rabiolo A, Bandello F. Eplerenone is not superior to placebo for chronic central serous chorioretinopathy. Comment. Lancet. 2020;25;395:252–3.
Sacconi R, Borrelli E, Querques G. Eplerenone for chronic central serous chorioretinopathy. Lancet. 2020;396:1556.
Lotery A, Sivaprasad S, O’Connell A, Harris RA, Culliford L, Ellis L, et al. Eplerenone for chronic central serous chorioretinopathy in patients with active, previously untreated disease for more than 4 months (VICI): a randomised, double-blind, placebo-controlled trial. Randomized Controlled Trial. Lancet. 2020;395:294–303.
Zola M, Daruich A, Matet A, Mantel I, Behar-Cohen F. Two-year follow-up of mineralocorticoid receptor antagonists for chronic central serous chorioretinopathy. Br J Ophtalmol. 2019;103:1184–9.
Yang J, Wang E, Yuan M, Chen Y. Three-dimensional choroidal vascularity index in acute central serous chorioretinopathy using swept-source optical coherence tomography. Graefes Arch Clin Exp Ophtalmol. 2020;258:241–7.
Yumusak E, Buyuktortop Gokcinar N, Ornek K. Choroidal thickness changes in non-treated acute and ranibizumab-treated chronic central serous chorioretinopathy. Observational Study. 2018;97:12885.
Manabe S, Shiragami C, Hirooka K, Izumibata S, Tsujikawa A, Shiraga F. Change of regional choroid thickness after reduced-fluence photodynamic therapy for chronic central serous chorioretinopathy. Am J Ophthalmol. 2015;159:644–51.
Izumi T, Koizumi H, Maruko I, Takahashi Y, Sonoda S, Sakamoto T, et al. Structural analyses of choroid after half-dose verteporfin photodynamic therapy for central serous chorioretinopathy. Br J Ophthalmol. 2017;101:433–7.
Sonoda S, Sakamoto T, Yamashita T, Uchino E, Kawano H, Yoshihara N, et al. Luminal and stromal areas of choroid determined by binarization method of optical coherence tomographic images. Am J Ophthalmol. 2015;159:1123–31.
Iovino C, Pellegrini M, Bernabei F, Borrelli E, Sacconi R, Govetto A, et al. Choroidal vascularity index: an in-depth analysis of this novel optical coherence tomography parameter. J Clin Med. 2020;9:595.
Van Rijssen TJ, Singh SR, Dijk EHC, Rasheed MA, Vupparaboina KK, Boon CJF, et al. Prospective evaluation of changes in choroidal vascularity index after half-dose photodynamic therapy versus micropulse laser treatment in chronic central serous chorioretinopathy. Graefes Arch Clin Exp Ophtalmol. 2020;258:1191–7.
Kwak JH, Hong S, Ra H, Kim EC, Kang NY, Baek J. Effect of acetazolamide on choroidal morphology in central serous chorioretinopathy. Korean J Ophtalmol. 2019;33:493–9.
Singh SR, Vupparaboina KK, Goud A, Dansingani KK, Chhablani J. Choroidal imaging biomarkers. Surv Ophthalmol. 2019;64:312–33.
Giannaccare G, Pellegrini M, Sebastiani S, Bernabei F, Moscardelli F, Claudio Iovino, et al. Choroidal vascularity index quantification in geographic atrophy using binarization of enhanced-depth imaging optical coherence tomographic scans. Retina. 2020;40:960–5.
Viggiano P, Toto L, Ferro G, Evangelista F, Porreca A, Mastropasqua R Choroidal structural changes in different intermediate AMD patterns. Eur J Ophtalmol. 1120672121992009 (2021).
Daruich A, Matet A, Dirani A, Bousquet E, Zhao M, Farman N, et al. Central serous chorioretinopathy: Recent findings and new physiopathology hypothesis. Prog Retin Eye Res. 2015;48:82–118.
Canonica J, Zhao M, Favez T, Gelizé E, Jonet L, Kowalczuk L, et al. Pathogenic effects of mineralocorticoid pathway activation in retinal pigment epithelium. Int J Mol Sci. 2021;22:9618.
Canonica J, Mehanna C, Bonnard B, Jonet L, Gelize E, Jais J-P, et al. Effect of acute and chronic aldosterone exposure on the retinal pigment epithelium-choroid complex in rodents. Exp Eye Res. 2019;187:107747.
Reiner A, Fitzgerald MEC, Del Mar N, Li C. Neural control of choroidal blood flow. Prog Retin Eye Res. 2018;64:96–130.
Gallice M, Daruich A, Matet A, Mouvet V, Dirani A, Evequoz G, et al. Acta Ophthalmol. 2021;99:e1375–e1381.
Maruko I, Iida T, Sugano Y, Ojima A, Sekiryu T. Subfoveal choroidal thickness in fellow eyes of patients with central serous chorioretinopathy. Retina. 2011;31:1603–8.
Sacconi R, Baldin G, Carnevali A, Querques L, Rabiolo A, Marchini G, et al. Response of central serous chorioretinopathy evaluated by multimodal retinal Imaging. Eye (Lond). 2018;32:734–42.
Goktas A. Correlation of subretinal fluid volume with choroidal thickness and macular volume in acute central serous chorioretinopathy. Eye (Lond). 2014;28:1431–6.
Imamura Y, Fujiwara F, Margolis R, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Retina. 2009;29:1469–73.
Li-hong Y, Bei T, Xue-hui S, Ding N, Zhou D, Wei W. Changes of choroidal thickness in central serous chorioretinopathy. Zhonghua Yan Ke Za Zhi. 2012;48:874–7.
Agrawal R, Gupta P, Tan KA, Cheung CMG, Wong T, Cheng C. Choroidal vascularity index as a measure of vascular status of the choroid: Measurements in healthy eyes from a population-based study. Sci Rep. 2016;12;6:21090.
Agrawal R, Chhablani J, Tann KA. Choroidal vascularity index in central serous chorioretinopathy. Retina. 2016;36:1646–51.
Maruko I, Lida T, Sugano Y, Ojima A, Ogasawara M, Spaide RF. Subfoveal choroidal thickness after treatment in central serous chorioretinopathy. Ophtalmol. 2010;117:1792–9.
Spaide RF, Koizumi H, Pozzonni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophtalmol. 2009;148:325.
Park W, Kim M, Kim RY, Park Y. Comparing effects of photodynamic therapy in central serous chorioretinopathy: full- dose versus half-dose versus half-dose-half-fluence. Graefes Arch Clin Exp Ophthalmol. 2019;257:2155–61.
Kasama S, Toyama T, Kumakura H, Takayama Y, Ichikawa S, Suzuki T, et al. J Am Coll Cardiol. 2003;41:574–81.
Author information
Authors and Affiliations
Contributions
Conceptualization, LT and RM; formal analysis, MDN and AP; investigation, PV; data curation, FE, CDN and GF; writing—original draft preparation, MLR; writing—review and editing, LT, RDA and RM. All authors have read and agreed to the published version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent statement
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Toto, L., Ruggeri, M.L., Evangelista, F. et al. Choroidal modifications assessed by means of choroidal vascularity index after oral eplerenone treatment in chronic central serous chorioretinopathy. Eye 37, 1214–1218 (2023). https://doi.org/10.1038/s41433-022-02091-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02091-6