Abstract
Purpose
To assess the choroidal vascularity index (CVI) after subthreshold laser treatment in patients with central serous chorioretinopathy (CSC).
Method
A total of 32 eyes with CSC were included in this study. In group 1, 14 eyes with persistent CSC were treated with the PASCAL (Endpoint Management Software) at 577-nm wavelength and in group 2, 18 eyes without treatment. The luminal area (LA), stromal area (SA), total area of choroid (TA), and CVI were measured by binarization (ImageJ) of optical coherence tomography images. Changes of choroidal structure parameters were evaluated over 3 months.
Result
A significant decrease was observed in LA, TA, and CVI at the third month after the laser treatment (p = 0.018, p = 0.024, p = 0.046). The best-corrected visual acuity (BCVA) and choriocapillaris plexus (CCP) flow area values were increased after treatment in group 1 (p < 0.001, p = 0.002). The final subfoveal fluid height, and CVI were lower in group 1 (p = 0.003, p = 0.011). The visual acuity and CCP flow area were higher in group 1 at the third month (p < 0.001, p = 0.003). A positive correlation between the final BCVA and CVI was observed (r = 0.539, p = 0.01).
Discussion
Decreased CVI was observed in CSC eyes after subthreshold yellow laser treatment. The CVI may be a useful index to evaluate the response to treatment.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSC) is a frequent cause of vision loss, particularly affecting men aged 20–50 years and idiopathic retinal disorder with therapeutic challenges. The pathway mechanisms of the underlying pathogenesis of the disease are still controversial. Increased permeability of the choriocapillaris is associated with detachment of the neurosensory retina due to a dysfunctional retinal pigment epithelium (RPE) [1, 2]. In 5–10% of patients, subretinal fluid may persist and RPE changes may occur, resulting in chronic disease that requires treatment [3].
In recent years, various novel nondamaging laser treatments that minimize tissue thermal damage have increased. These treatments limit the transmission of thermal energy to photoreceptors by raising the temperature of the RPE to just below the protein denaturation threshold, and no visible burns occur [4, 5]. The important advantages of subthreshold laser therapy are that we can apply the treatment near the fovea and treat the same area multiple times. Subthreshold laser treatment applied to CSC patients has been described before and its effects on visual improvement are evaluated [6]. A previous clinical study has shown that subthreshold laser therapy reduces subretinal fluid and provides a visual improvement in patients with CSC [5,6,7].
Expansion of the choroidal vessels and leakage into the interstitial space are well-recognized hallmarks of CSC, and anatomical follow-up of the disease is often performed with enhanced depth imaging-optical coherence tomography (EDI-OCT). In recent years, more detailed information has been obtained through digital image processing research and various software programs. The choroidal vascularity index (CVI) is also a useful method to assess the anatomical components of the choroid, obtained by these digital image binarization methods [8].
In the current study, we evaluated the luminal area of choroid (LA), stromal area (SA), and the CVI and the association of these anatomical parametric with functional outcomes in CSC patients after subthreshold laser photocoagulation in the patients with CSC.
Method
Thirty-two CSC patients have been included in this prospective study. The study was approved by the institutional review board/ethics committee of Mugla Sitki Kocman University, Faculty of Medicine, and followed all the ethical standards stated in the Declaration of Helsinki (approval number: 9/IV). All participants were informed about the clinical study, the treatment to be performed, and their written consent was obtained. All of the cases had CSC (≥4 months of duration), and all of them were treatment-naive patients.
The inclusion criterion was the diagnosis of CSC disease lasting 4 months or longer. Cases with any history of other macular disease, choroidal neovascular membrane (CNV), retinal vessel occlusion, diabetic retinopathy, a history of photodynamic therapy (PDT), antivascular endothelial growth factor (anti-VEGF) treatment, laser photocoagulation or intraocular surgery were excluded from the study.
Demographic information and treatment follow-up notes of all participating individuals were recorded. All cases underwent a detailed ophthalmic examination that included measurement of best-corrected visual acuity (BCVA), slit-lamp examination, fundus examination, OCT, fundus fluorescein angiography (FFA), EDI-OCT, and optical coherence tomography angiography (OCTA). BCVA was measured using the Snellen visual acuity chart, then converted to logarithms of minimum angle of resolution (logMAR) units for statistical analysis. Written and verbal informed consent, clearly explaining all potential risks and possible benefits of subthreshold laser treatment or observation, was discussed with and obtained from every patient, adhering to good clinical practice regulations and the tenets of the Declaration of Helsinki. As a result of the informed consent, laser treatment was applied to those who accepted to have subthreshold yellow laser treatment. We elected in favor of a real-life random distribution with each study participant deciding their treatment of choice based on the received standardized information. The CSC patients were split into two parts by whether they received subthreshold yellow laser treatment or not. Group 1 consisted of 14 eyes of 14 patients treated with the subthreshold laser. Group 2 consisted of 18 eyes of 18 patients without laser treatment.
PASCAL laser (Topcon Medical Laser Systems, CA) with a wavelength of 577 nm (yellow laser) was preferred as phototherapy. OCT thickness map, FFA, and fundus autofluorescence images were evaluated together to determine the extent of the subretinal fluid and the location of serous detachment. When adjusting the laser power, we firstly titrated the laser power with 15 ms pulses, defined as 100% pulse energy, creating a barely visible burn in a region distant from the macula between the temporal arcades. All energy level corresponds to an individual pair of laser power and pulse duration, as was explained previously [9]. We used Endpoint Management (EpM) Software. The EpM permits putting some of the edge spots of the pattern at 100% energy to produce visible marks for adjustment. Then phototherapy was done on the leaky site in the FFA and over the area with subretinal fluid, using 30% pulse energy with 200-µm retinal spot sizes and the spot spacing of 0.25 beam diameter. To prevent possible photo-injury of the fovea, laser beams were applied at a safe distance of 500 µm from the fovea.
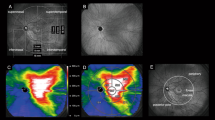
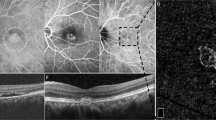
The central macular thickness (CMT) was automatically measured with OCT (Spectralis OCT, Heidelberg, Germany). Subfoveal choroidal thickness (SCT) and the subretinal fluid height (SFH) were manually measured using EDI-OCT scans. The CVI was measured by binarization of EDI-OCT images. The image binarization was performed using a public domain software (ImageJ, National Institutes of Health, Bethesda, MD, USA) previously described by Agrawal et al. [8]. The choroidal area was measured manually at 3000-μm wide with the margins of 1500-μm nasal and 1500-μm temporal from the foveal center horizontally and from the RPE to the choroidoscleral border vertically. First, the unit of length (as µm) and pixel distance (200 µm) was designated in the set scale. The images were converted to 8-bit type, and then binarized to view the choroid-scleral junction using the Niblack autolocal threshold. Next, the polygon tool was used to select the total choroidal area between the RPE and choroid-scleral junction. This area was saved to the region of interest (ROI) manager. The images were then converted to Red–Green–Blue color type, and the color threshold tool was used to select the dark pixels expressing the LA and was added to the ROI manager. Finally, in order to determine the area of vascularity within the selected polygon, both areas in the ROI manager were selected and merged using the “AND” command (Fig. 1A). CVI value was determined as the ratio of LA to TA. The light color pixels represented SA that was calculated by subtracting the LA from the TA. These values were measured separately by two researchers who were blinded to the clinical information of the patients. The means of measurements by the two researchers were used in the statistical analysis. The interobserver reliability of manual calculations was evaluated using intraclass correlation coefficients. Interinvestigator reliability between two retina specialists was assessed with a κ value, which was 0.978 (p < 0.001).
The choriocapillaris plexus (CCP) flow area was automatically measured as just the detected flow signals at a radius of 3000 µm centered on the FAZ via OCTA (RTVue; Optovue, CA) (Fig. 1B). The images that scan quality of OCTA below 7/10 were excluded from the study. In cases where the device was faulty or insufficient in automatic segmentation, we corrected it manually. Changes in BCVA and choroidal structure parameters were evaluated over 3 months of follow-up and were compared between the groups at the third month.
The SPSS 21.0 software program was used. The quantitative variables were controlled by the Kolmogorov–Smirnov test for the normality hypothesis. The contingency tables and χ2 test or Fisher’s test (when required) were used to compare the categorical variables. The independent t-test was used for comparisons of parameters between independent groups at baseline and at the third month. The paired Student t-test was used to compare the clinical values over time after the treatment. To determine the relationship between visual acuity and clinical choroidal structure parameters, Pearson’s correlation tests were measured. The p value <0.05 was considered statistically significant.
Results
A total of 32 eyes from 32 patients with CSC were identified in this prospective study comprising 23 men and 9 women with a mean age of 48 years. No statistically significant differences were present among the groups with respect to age, sex, duration of symptoms, smoking status, prior steroid use. Furthermore, no significance in initial visual acuity or anatomical parameters among the groups was observed. A summary of the baseline characteristics and outcomes of image binarization analysis used in this study is presented in Table 1.
Compared to the initial assessments in group 1, a significant decrease was obtained in CMT, SCT, SFH, LA, TA, and CVI after subthreshold laser treatment at the third month (respectively, p ≤ 0.001, p = 0.03, p < 0.001, p = 0.018, p = 0.024, p = 0.046). The mean CVI was decreased from 74.29 ± 8.27 to 67.67 ± 5.44 after the laser treatment in group 1. The BCVA was increased from 0.41 ± 0.1 to 0.11 ± 0.09 logMAR and CCP flow area values were increased from 19,341 ± 572.6 to 20,269 ± 469 mm2 at 3 months after laser treatment in group 1 (p < 0.001, p = 0.002). SFH was regressed from 186.2 ± 68.1 to 48.2 ± 48.8 µm in eyes receiving laser treatment (p < 0.001). However, there was no statistically significant change concerning BCVA, SFH, and choroidal structure parameters in group 2 at the final visit compared to the baseline values (Table 2).
There were no adverse effects associated with the treatment. After laser treatment, there were no visible traces detectable by OCT or fundus autofluorescence. The solely noticeable marks of the approach were the landmarks, which seem like a point of increased autofluorescence of the RPE in the titration region.
At the third month, the CVI was 67.67 ± 5.44% in group 1 and 72.7 ± 5.13% in group 2. The final CMT, SFH, and CVI was significantly lower in group 1 than group 2 (p = 0.006, p = 0.003, p = 0.003, p = 0.011). The final BCVA was 0.11 ± 0.09 logMAR in the group 1 and 0.36 ± 0.18 logMAR in the group 2. The BCVA and CCP flow area were higher in group 1 at the 3 months (p < 0.001, p = 0.003) (Table 3). Subretinal fluid totally resolved in 10 eyes of 14 eyes (71.4%) of the patients after laser treatment at the third month. In 4 (28.6%) laser-treated eyes, the subretinal fluid persisted at the final visit and the mean SFH decreased from 210 ± 83 to 168.5 ± 59 µm. In eyes with complete response to laser treatment, the mean CVI, TA, and LA were lower than in the eyes with limited response (for eyes without subretinal fluid, the mean CVI = 66.5 ± 5.6%, TA = 1.25 ± 0.28 mm2, LA = 0.84 ± 0.23 mm2; for eyes with subretinal fluid persisted at the final visit, the mean CVI = 70.6 ± 3.8%, TA = 1.5 ± 0.16 mm2, LA = 1.06 ± 0.13 mm2).
When we examined the follow-ups of the untreated group, subretinal fluid in 2 eyes (11.1%) of 18 eyes completely resolved spontaneously after three months. Subretinal fluid persisted in the other 16 eyes at the end of the third month. In 5 of 16 eyes, CMT was decreased (min–max: 10–47 µm). There was no statistically significant change in terms of CMT and SFH in 16 eyes of untreated patients at the final visit compared to the baseline values (CMT was decreased from 439.3 ± 24 to 429.9 ± 31 µm, p = 0.353. SFH was decreased from 156.2 ± 56 to 143.9 ± 75 µm, p = 0.580).
We obtained a positive correlation between the BCVA and CMT, SFH, LA, and CVI by month 3. A negative correlation between BCVA and CCP flow area was observed (Table 4).
Discussion
In the current study, we reported the visual acuity and choroidal anatomic results obtained with the image binarization method after subthreshold yellow laser photocoagulation. The visual acuity was improved at 3-month in the laser-treated group. Concerning the choroidal structural outcomes, in CSC eyes with subthreshold yellow laser treatment, a significant decrease was remarked in SFH, LA, and CVI at the third month after treatment. A positive correlation between the BCVA and SFH, LA, and CVI was obtained in our study.
Several authors have demonstrated dilatation of choroidal vessels and increased SCT in CSC patients using EDI-OCT [10, 11]. Previous studies with indocyanine green angiography have shown that CSC shows choroidal vessel dilatation in the acute phase, as well as diffuse leakage from the choriocapillaris to the stroma [12, 13]. The pachychoroid spectrum disorders are affected by increased choroidal vascularity due to functional and structural changes of the choroid. Therefore, measuring choroidal thickness alone may not be sufficient to investigate the disease profile and response to therapy. For this reason, new quantitative values such as CVI, which provides more detailed information about anatomy by processing images obtained in pachychoroid spectrum diseases, have been frequently used in clinical investigations in recent years. The CVI may be a valuable index to provide additional data to evaluate the choroidal anatomical structure.
Agrawal et al. showed that there is also an increase in LA, the vascular component associated with an increase in CVI in CSC compared to fellow eyes and healthy eyes [8]. Furthermore, increased CVI in the CSC patients had been demonstrated by other studies [8, 14], The CVI, the ratio of LA to TA, is a parameter that quantitatively describes the choroidal vasculature and is evaluated in various chorioretinal diseases in the literature. Another study that included the chronic CSC patients demonstrated a significant decrease in SCT and TA, LA, and CVI after half-dose full fluency PDT treatment [15]. Iovino et al. demonstrated that the CMT, SCT, TA, and LA were decreased after PDT for chronic CSC. Furthermore, they supported that these choroidal parameters may provide additional quantitative biomarkers to evaluate the anatomic response to therapy. However, they did not find any significant difference in terms of CVI [3]. In contrast to their study, we observed a significant decrease in CVI values after subthreshold yellow laser treatment. This difference may be due to the following reasons: we applied subthreshold laser treatment instead of PDT and a submacular 3-mm choroidal area was used for calculating CVI and image processing.
Acute CSC often does not require treatment, but in chronic CSC, the prolonged presence of subretinal fluid can damage the photoreceptor layer and cause permanent vision loss [16]. Therefore, treatment may be indicated in chronic CSC to achieve earlier visual recovery and also to reduce the possible risk of macular damage. In recent years, various treatment approaches have been reported for chronic CSC. Conventional laser treatments can induce thermal injuries in the retina, they have also side effects such as visual field defects, focal scar enlargement, CNV, and the development of new leak sites [17]. PDT, another alternative therapy, has achieved successful anatomical outcomes in the treatment of chronic CSC, but has various side effects such as choroidal ischemia, rupture or RPE atrophy, and CNV [6, 18,19,20,21]. Anti-VEGF agents have little place in the management of CSC in daily practice unless secondary CNV develops [21].
Previous studies using subthreshold micropulse laser (SML) treatment demonstrated a success rate of approximately 70% in patients with chronic CSC [22, 23]. Kim et al. presented that in chronic CSC patients subretinal fluid was resolved in 81.5% at 1 year after the SML treatment [6]. In the PLACE trial which was a multicentric randomized controlled clinical trial, the investigators compared the anatomic and functional efficacy and safety of half-dose PDT versus high-density subthreshold micropulse diode laser (HSML) treatment in patients with chronic CSC [24]. The outcomes of the study demonstrated that 67.2% of PDT-treated patients and 28.8% of HSML-treated patients had complete resorption of subretinal fluid at 8 months. They found that the efficacy of half-dose PDT concerning for complete resolution of subretinal fluid was superior compared with HSML. However, at the final evaluation visit, there is no significant difference in terms of the increase in BCVA relative to baseline between the groups and the authors reported similar results to prevent visual loss [24]. Van Rijssen et al. evaluated the CVI in 29 chronic CSC eyes after the PDT and HSML treatment. In their study, the change in CVI, when comparing CVI before and after treatment for both groups, was not significant. Furthermore, they observed no significant correlation between CVI and BCVA [25]. Although different devices and lasers of different wavelengths were used in all these studies, similar mechanisms (stimulation of the RPE pump, increase of cellular functions) of nondamaging subthreshold laser beam therapy in chronic CSR mediated the decrease in subretinal fluid and the increase in visual acuity.
However, in our study, we applied subthreshold yellow laser treatment with EpM software to eyes with CSC instead of micropulse laser. EpM software has some advantages over micropulse laser therapy, such as providing a suitable titration protocol for each patient, providing the appropriate energy level to stimulate the RPE in each patient, using shorter pulses and patterns, allowing faster and more reproducible treatment, and allowing the treatment site to be marked [26]. Lavinsky et al. reported that 75% of laser-treated patients had demonstrated no subretinal fluid in the sixth month in a study that used EpM software at 577-nm wavelength. They concluded that the 577-nm PASCAL laser treatment with EpM was safe, and it increased visual acuity and resolved subretinal fluid in CSC [26]. Similar to previous results, in our study, 71.4% of laser-treated patients had complete regression of subretinal fluid and BCVA was significantly increased after subthreshold yellow laser treatment at the third month. CVI was found to be lower in cases with good response (subretinal fluid totally resolved) to subthreshold laser compared to eyes with limited response. Although the sample size was small for definitive conclusions, it suggested that CVI may be valuable in evaluating response to treatment.
The dynamic response of the retina to non-destructive hyperthermia was observed by evaluating the amount of heat shock protein (HSP70) expressed in previous animal experiments [27, 28]. The mechanism of action is hypothesized to be as follows; The upregulation of HSPs induced by thermal stress in the RPE and choroid results in increased fluid pumping ability and cellular functions of the retina [26]. Furthermore, the 577-nm yellow laser has some advantages over the 810-nm diode laser. The subthreshold yellow laser treatment produces combined absorption by both melanin and oxyhaemoglobin, resulting in maximum absorption in the RPE and choriocapillaris. It also has little xanthophyll absorption that allows the repeated therapy close to the fovea. It causes lower intraocular light scattering and lower pain. The major advantages of the procedure are the tissue-sparing effect and the reproducibility of the sessions after 3 months in case of recurrence or unresponsiveness of subretinal fluid [6, 29].
The precise pathophysiological changes that lead to CSC-related RPE leakage remain unclear. Studies with indocyanine green angiography have also shown delayed filling of areas with choroidal hyperpermeability, suspecting that this may be a functional result of CCP ischemia in CSC [30, 31]. Demirel et. al reported that the vascular density and flow area of CCP were lower in eyes with CSC. They also suggest that the severity of the CCP ischemia secondary to enlarged choroidal vessels may be related to RPE abnormalities and subretinal fluid [31]. Shadowing artifacts or a decrease in perfusion of choriocapillaris may cause a decreased CCP flow area. In our study, the CCP flow area was increased after treatment. It was due to decrease ischemia of CCP or reducing shadowing artifact after laser treatment. Therefore, it is difficult to make a definitive comment on this issue, and detailed studies are needed in the future.
Limitations of the study are relatively short follow-up times, non-randomized nature, and lack of a control group. Another limitation is that settings such as treatment type, laser characteristics such as duration, power, titration, and wavelength are different in recently published studies. This limitation is important when evaluating outcomes and response to treatment compared to previous studies. There were also some methodological restrictions with the binarization method, such as the absence of a spatial resolution to detect the luminal and stromal components of the choriocapillaris, shadowing of more extended retinal vascular structures on the choroid that could result in CVI variations [32]. However, the prospective design of our study and the homogenization of the groups in the study increase the value of the results obtained in the study. In addition, our study included preliminary choroidal structure and CVI findings regarding CSC patients treated with subthreshold yellow laser and will shed light on future studies. As far as we know, there has been no investigation linked to CVI in CSC patients who received subthreshold yellow laser photocoagulation.
In conclusion, this study showed a significant decline of SCT, LA, TA, and CVI in patients with chronic CSC undergoing nondamaging subthreshold yellow laser at 3-month with visual acuity gain. Our investigation may contribute further confirmation of the targeted influence of subthreshold yellow laser on the healing of the hyperpermeable choroidal vessels. The nondamaging laser was effective in improving both visual acuity and resorption of the subretinal fluid, providing good anatomical and physiological results. However, no significant functional and anatomical improvement was observed in patients who did not receive treatment. The results of our study suggest that quantification of CVI in addition to SCT from EDI-OCT can contribute to assessing the choroidal anatomical response to therapy. Further comprehensive multidisciplinary studies are needed for more precise interpretations.
Summary
What was known before
-
CVI was previously known to provide additional data to evaluate the anatomical structure of the choroid. Subthreshold laser treatment applied to CSC patients has been described before and its effects on visual improvement.
What this study adds
-
The 577-nm subthreshold laser treatment with EpM increased the visual acuity and resolved subretinal fluid in CSC. Decreased CVI in CSC eyes after subthreshold yellow laser treatment is useful in the anatomical evaluation of the choroid.
References
Piccolino FC, de la Longrais RR, Ravera G, Eandi CM, Ventre L, Abdollahi A, et al. The foveal photoreceptor layer and visual acuity loss in central serous chorioretinopathy. Am J Ophthalmol. 2005;139:87–99.
Bae SH, Heo JW, Kim C, Kim TW, Lee JY, Song SJ, et al. A randomized pilot study of low-fluence photodynamic therapy versus intravitreal ranibizumab for chronic central serous chorioretinopathy. Am J Ophthalmol. 2011;152:784–92.e782.
Iovino C, Au A, Chhablani J, Parameswarappa DC, Rasheed MA, Cennamo G, et al. Choroidal anatomic alterations after photodynamic therapy for chronic central serous chorioretinopathy: a multicenter study. Am J Ophthalmol. 2020;217:104–13.
Gupta B, Elagouz M, McHugh D, Chong V, Sivaprasad S. Micropulse diode laser photocoagulation for central serous chorio-retinopathy. Clin Exp Ophthalmol. 2009;37:801–5.
Lavinsky D, Wang J, Huie P, Dalal R, Lee SJ, Lee DY, et al. Nondamaging retinal laser therapy: rationale and applications to the macula. Invest Ophthalmol Vis Sci. 2016;57:2488–500.
Kim YJ, Kim SY, Ha S, Moon D, Seong S, Kwon OW, et al. Short-duration multiple-session subthreshold micropulse yellow laser (577 nm) for chronic central serous chorioretinopathy: results at 3 years. Eye (Lond). 2019;33:819–25.
Koss MJ, Beger I, Koch FH. Subthreshold diode laser micropulse photocoagulation versus intravitreal injections of bevacizumab in the treatment of central serous chorioretinopathy. Eye (Lond). 2012;26:307–14.
Agrawal R, Chhablani J, Tan KA, Shah S, Sarvaiya C, Banker A. Choroidal vascularity index in central serous chorioretinopathy. Retina. 2016;36:1646–51.
Lavinsky D, Sramek C, Wang J, Huie P, Dalal R, Mandel Y, et al. Subvisible retinal laser therapy: titration algorithm and tissue response. Retina. 2014;34:87–97.
Brandl C, Helbig H, Gamulescu MA. Choroidal thickness measurements during central serous chorioretinopathy treatment. Int Ophthalmol. 2014;34:7–13.
Kim YT, Kang SW, Bai KH. Choroidal thickness in both eyes of patients with unilaterally active central serous chorioretinopathy. Eye (Lond). 2011;25:1635–40.
Guyer DR, Yannuzzi LA, Slakter JS, Sorenson JA, Ho A, Orlock D. Digital indocyanine green videoangiography of central serous chorioretinopathy. Arch Ophthalmol. 1994;112:1057–62.
Borooah S, Sim PY, Phatak S, Moraes G, Wu CY, Cheung CMG, et al. Pachychoroid spectrum disease. Acta Ophthalmol. 2021;99:e806–e822.
Singh SR, Vupparaboina KK, Goud A, Dansingani KK, Chhablani J. Choroidal imaging biomarkers. Surv Ophthalmol. 2019;64:312–33.
Izumi T, Koizumi H, Maruko I, Takahashi Y, Sonoda S, Sakamoto T, et al. Structural analyses of choroid after half-dose verteporfin photodynamic therapy for central serous chorioretinopathy. Br J Ophthalmol. 2017;101:433–7.
Wang M, Munch IC, Hasler PW, Prunte C, Larsen M. Central serous chorioretinopathy. Acta Ophthalmol. 2008;86:126–45.
Little HL. Complications of argon laser retinal photocoagulation: a five-year study. Int Ophthalmol Clin. 1976;16:145–59.
Cardillo Piccolino F, Eandi CM, Ventre L, Rigault de la Longrais RC, Grignolo FM. Photodynamic therapy for chronic central serous chorioretinopathy. Retina. 2003;23:752–63.
Koytak A, Erol K, Coskun E, Asik N, Ozturk H, Ozerturk Y. Fluorescein angiography-guided photodynamic therapy with half-dose verteporfin for chronic central serous chorioretinopathy. Retina. 2010;30:1698–703.
Taban M, Boyer DS, Thomas EL, Taban M. Chronic central serous chorioretinopathy: photodynamic therapy. Am J Ophthalmol. 2004;137:1073–80.
Pitcher JD III, Witkin AJ, DeCroos FC, Ho AC. A prospective pilot study of intravitreal aflibercept for the treatment of chronic central serous chorioretinopathy: the CONTAIN study. Br J Ophthalmol. 2015;99:848–52.
Chen SN, Hwang JF, Tseng LF, Lin CJ. Subthreshold diode micropulse photocoagulation for the treatment of chronic central serous chorioretinopathy with juxtafoveal leakage. Ophthalmology. 2008;115:2229–34.
Yadav NK, Jayadev C, Mohan A, Vijayan P, Battu R, Dabir S, et al. Subthreshold micropulse yellow laser (577 nm) in chronic central serous chorioretinopathy: safety profile and treatment outcome. Eye (Lond). 2015;29:258–64.
van Dijk EHC, Fauser S, Breukink MB, Blanco-Garavito R, Groenewoud JMM, Keunen JEE, et al. Half-dose photodynamic therapy versus high-density subthreshold micropulse laser treatment in patients with chronic central serous chorioretinopathy: The PLACE Trial. Ophthalmology. 2018;125:1547–55.
van Rijssen TJ, Singh SR, van Dijk EHC, Rasheed MA, Vupparaboina KK, Boon CJF, et al. Prospective evaluation of changes in choroidal vascularity index after half-dose photodynamic therapy versus micropulse laser treatment in chronic central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol. 2020;258:1191–7.
Lavinsky D, Palanker D. Nondamaging photothermal therapy for the retina: initial clinical experience with chronic central serous retinopathy. Retina. 2015;35:213–22.
Sramek C, Mackanos M, Spitler R, Leung LS, Nomoto H, Contag CH, et al. Non-damaging retinal phototherapy: dynamic range of heat shock protein expression. Invest Ophthalmol Vis Sci. 2011;52:1780–7.
Kern K, Mertineit CL, Brinkmann R, Miura Y. Expression of heat shock protein 70 and cell death kinetics after different thermal impacts on cultured retinal pigment epithelial cells. Exp Eye Res. 2018;170:117–26.
Mainster MA. Decreasing retinal photocoagulation damage: principles and techniques. Semin Ophthalmol. 1999;14:200–9.
Spaide RF, Hall L, Haas A, Campeas L, Yannuzzi LA, Fisher YL, et al. Indocyanine green videoangiography of older patients with central serous chorioretinopathy. Retina. 1996;16:203–13.
Demirel S, Degirmenci MFK, Batioglu F, Ozmert E. Evaluation of the choroidal features in pachychoroid spectrum diseases by optical coherence tomography and optical coherence tomography angiography. Eur J Ophthalmol. 2021;31:184–93.
Agrawal R, Ding J, Sen P, Rousselot A, Chan A, Nivison-Smith L, et al. Exploring choroidal angioarchitecture in health and disease using choroidal vascularity index. Prog Retin Eye Res. 2020;77:100829.
Author information
Authors and Affiliations
Contributions
STK was responsible for designing the review protocol, writing the protocol and report, conducting the search, screening potentially eligible studies, extracting and analyzing data, interpreting results, updating reference lists, and creating tables. AK was responsible for designing the review protocol and screening potentially eligible studies. She contributed to writing the report, extracting and analyzing data, interpreting results, and creating tables. AhK conducted the meta-regression analyses and contributed to the design of the review protocol, writing the report, arbitrating potentially eligible studies, extracting and analyzing data, and interpreting results. SCT contributed to data extraction and provided feedback on the report. SS provided feedback on the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaderli, S.T., Karalezli, A., Kaderli, A. et al. Evaluation of the choroidal vascularity index after subthreshold yellow laser treatment in the patients with chronic central serous chorioretinopathy. Eye 36, 1826–1831 (2022). https://doi.org/10.1038/s41433-022-02090-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02090-7