Abstract
Aims
To assess time to, cumulative incidence of, and functional benefit of achieving sustained ≥2-step Diabetic Retinopathy Severity Scale (DRSS) improvement in diabetic macular oedema (DMO).
Methods
Post hoc analysis of VISTA/VIVID including eyes with DMO treated with intravitreal aflibercept injections (IAI), 2 mg q4 weeks (2q4, n = 250) or q8 weeks after 5 monthly doses (2q8, n = 249), or laser control (n = 249). Changes from baseline in best-corrected visual acuity (BCVA) and central subfield thickness (CST) were evaluated in sustained (≥2 consecutive visits) DRSS subgroups (≥1-step worsening, no change, ≥2-step improvement).
Results
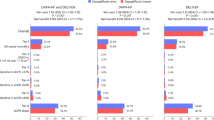
Time to sustained ≥2-step DRSS improvement was shorter for both the IAI 2q4 and IAI 2q8 groups versus laser (both log-rank p < 0.001). Cumulative incidences of sustained ≥2-step DRSS improvement with IAI 2q4 and IAI 2q8 versus laser were 40.0% and 42.8% versus 15.5% (both p < 0.001) through week 100. Mean differences (95% CI) in BCVA gains from baseline at weeks 52 and 100 between eyes with sustained ≥2-step DRSS improvement versus sustained ≥1-step DRSS worsening were –3.0 (–8.9, 2.9) and 6.2 (0.2, 12.2) letters with laser, and 4.2 (0.8, 7.6) and 4.9 (1.3, 8.4) letters with IAI combined, respectively. Difference (95% CI) in CST reduction was significantly greater only with IAI combined at week 100 (–83.0 [–140.8, –25.3]). Correlations between BCVA and CST changes were weak.
Conclusions
DMO eyes treated with IAI achieved sustained ≥2-step DRSS improvement significantly earlier and more frequently versus laser. This improvement was associated with greater BCVA gains, independent of CST reductions.
Trial registration
ClinicalTrials.gov (https://clinicaltrials.gov/) identifiers: NCT01363440 and NCT01331681.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Qualified researchers may request access to study documents (including the clinical study report, study protocol with any amendments, blank case report form, statistical analysis plan) that support the methods and findings reported in this manuscript. Individual anonymised participant data will be considered for sharing once the indication has been approved by major health authorities, if there is legal authority to share the data and there is not a reasonable likelihood of participant re-identification. Submit requests to https://vivli.org/.
References
Early Treatment Diabetic Retinopathy Study Research Group. Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Ophthalmology. 1991;98:823–33.
Coyne KS, Margolis MK, Kennedy-Martin T, Baker TM, Klein R, Paul MD, et al. The impact of diabetic retinopathy: perspectives from patient focus groups. Fam Pract. 2004;21:447–53.
Mazhar K, Varma R, Choudhury F, McKean-Cowdin R, Shtir CJ, Azen SP, et al. Severity of diabetic retinopathy and health-related quality of life: the Los Angeles Latino Eye Study. Ophthalmology. 2011;118:649–55.
Willis JR, Doan QV, Gleeson M, Haskova Z, Ramulu P, Morse L, et al. Vision-related functional burden of diabetic retinopathy across severity levels in the United States. JAMA Ophthalmol. 2017;135:926–32.
Klein R, Klein BE, Moss SE, Cruickshanks KJ. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. XV. The long-term incidence of macular edema. Ophthalmology. 1995;102:7–16.
Mitchell P, McAllister I, Larsen M, Staurenghi G, Korobelnik JF, Boyer DS, et al. Evaluating the impact of intravitreal aflibercept on diabetic retinopathy progression in the VIVID-DME and VISTA-DME studies. Ophthalmol Retin. 2018;2:988–96.
Korobelnik JF, Do DV, Schmidt-Erfurth U, Boyer DS, Holz FG, Heier JS, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121:2247–54.
Brown DM, Schmidt-Erfurth U, Do DV, Holz FG, Boyer DS, Midena E, et al. Intravitreal aflibercept for diabetic macular edema: 100-week results from the VISTA and VIVID studies. Ophthalmology. 2015;122:2044–52.
Ip MS, Zhang J, Ehrlich JS. The clinical importance of changes in diabetic retinopathy severity score. Ophthalmology. 2017;124:596–603.
Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol. 1985;103:1796–806.
Browning DJ, Glassman AR, Aiello LP, Beck RW, Brown DM, Fong DS, et al. Relationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology. 2007;114:525–36.
Bressler SB, Odia I, Maguire MG, Dhoot DS, Glassman AR, Jampol LM, et al. Factors associated with visual acuity and central subfield thickness changes when treating diabetic macular edema with anti-vascular endothelial growth factor therapy: an exploratory analysis of the Protocol T randomized clinical trial. JAMA Ophthalmol. 2019;137:382–9.
Brown DM, Wykoff CC, Boyer D, Heier JS, Clark WL, Emanuelli A, et al. Evaluation of intravitreal aflibercept for the treatment of severe nonproliferative diabetic retinopathy: results from the PANORAMA randomized clinical trial. JAMA Ophthalmol. 2021;139:946–55.
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119:789–801.
Acknowledgements
Medical writing support was provided by Melissa Purves, PhD, and Rob Campbell, PhD, of Core (London, UK) according to Good Publication Practice guidelines (link) and was funded by Regeneron Pharmaceuticals, Inc.
Funding
This study was funded by Regeneron Pharmaceuticals, Inc.
Author information
Authors and Affiliations
Contributions
All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the concept and design of the study; acquisition, analysis, and interpretation of the data; drafting of the manuscript; and critical revision of the manuscript for important intellectual content. WD provided the statistical analysis.
Corresponding author
Ethics declarations
Competing interests
DSD is a consultant for Bayer, Novartis, Regeneron Pharmaceuticals, Inc., Genentech, Allergan, Alimera, Santen, Allegro, Notal Vision, and Eyepoint Pharmaceuticals. HM, KR, WD, RV and AJB are employees of and hold equity in Regeneron Pharmaceuticals, Inc. RPS is a consultant for Genentech/Roche, Regeneron Pharmaceuticals, Inc., Novartis, Zeiss, Bausch and Lomb, Asclepix, Alcon, and Gyroscope and has received research funding from Apellis and NGM Biopharma.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Dhoot, D.S., Moini, H., Reed, K. et al. Functional outcomes of sustained improvement on Diabetic Retinopathy Severity Scale with intravitreal aflibercept in the VISTA and VIVID trials. Eye 37, 2020–2025 (2023). https://doi.org/10.1038/s41433-022-02058-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02058-7