Abstract
Background/Objectives
To investigate the association between visual acuity (VA) and visual field (VF) and its reproducibility in patients with retinitis pigmentosa (RP).
Subjects/Methods
The study cohort comprised 227 eyes of 227 patients with RP. The reproducibility of two Humphrey VF tests (10-2 Swedish Interactive Threshold Algorithm [SITA] tests) performed within a period of 3 months was calculated using the root mean squared error (RMSE) of each VF test point’s sensitivity. The association between the logarithm of the minimum angle of resolution (logMAR) VA and VF sensitivity was investigated. Additionally, the relationship between RMSE and age, fixation loss, false positives, false negatives, and logMAR VA was determined.
Results
The association between visual sensitivity and VA was most tight at the fovea, and it became weak toward the peripheral region in an eccentric manner. VF reproducibility appreciably increased as VA decreased. In particular, reproducibility was significantly decreased when logMAR VA was >0.5 compared with logMAR VA ≤ 0.
Conclusion
Reproducibility of VF tests decreases with a decrease in VA. Careful consideration is necessary when a patient’s logMAR VA is >0.5.
Similar content being viewed by others
Introduction
Retinitis pigmentosa (RP) is a hereditary retinal disease characterized by the progressive loss of photoreceptors [1, 2]. The symptoms include nyctalopia and constriction of the visual field (VF), which sometimes progresses to legal blindness. Precise VF measurement is crucial to assess RP and can be performed using a static automated perimeter, such as the Humphrey Field Analyzer (HFA) (Carl Zeiss Meditec Inc., Dublin, CA) [3, 4]. In particular, the central VF can be quantitatively measured using the HFA 10-2 test [5,6,7]. However, the sensitivity of the measured VF fluctuates [8, 9], which is problematic when detecting progression using either event-type or trend-type analysis for the clinical settings because the detectability of progression is markedly reduced in a series of VFs with poor reproducibility [10]. This is also important when interpreting the results of clinical studies because VF measurements are often the primary endpoint in clinical research studies, including clinical trials evaluating the effect of pharmacologic agents [11,12,13,14,15] and other variables [6, 7]. An ideal method to estimate the reliability of measured VF may be repeating the VF measurement and calculating the test-retest reproducibility, but it is unrealistic to adopt this approach in all patients. Instead, the reliability of VF measurements is usually estimated using fixation loss (FL), false-positive (FP), and false-negative (FN) rates [16, 17]. However, recent studies have highlighted limitations of these measurements [18,19,20,21,22].
Generally, VF reproducibility worsens as the VF deteriorates [23]. Visual acuity (VA) is closely correlated with sensitivities in the central area of the VF, and it is usually unaffected until late-stage RP. Indubitably, VA is essential to accurately measure VF because stable fixation cannot be ensured otherwise, implying that VA is closely related to VF reproducibility. Nonetheless, VA has not been included in the inclusion criteria in previous studies in general [6, 7, 11,12,13,14], which would make the assessment of VF progression inaccurate, and as a result, the difference of VF progression between two groups, such as between treated and placebo groups, may be masked. Thus, the primary objective of this study was to comprehensively investigate the association between visual sensitivity in the central VF and VA in eyes with RP. Subsequently, the association between VF reproducibility and VA was analysed.
Method
This study was approved by the Research Ethics Committee of the Graduate School of Medicine and Faculty of Medicine at the University of Tokyo and Kyoto University. The study complied with the tenets of the Declaration of Helsinki. Written informed consent was given by patients for their information to be stored in the hospital database and used for research. Otherwise, based on the regulations of the Japanese Guidelines for Epidemiologic Study 2008 (issued by the Japanese Government), the study protocols did not require that each patient provide written informed consent. Instead, the protocol was posted at the outpatient clinic and/or website of the department to notify study participants.
Subjects
We retrospectively examined 238 eyes of 227 patients with RP (96 males and 131 females). All patients underwent 10-2 HFA VF tests (Humphrey Field Analyzer II; Carl Zeiss Meditec Inc.) twice within 3 months between June 2007 and September 2019. Only one eye per patient was included, and if both eyes satisfied the inclusion criteria, the right eye was automatically chosen.
RP was diagnosed when the following findings were present: (1) typical fundus findings of RP, such as bone spicule pigmentation, arteriolar attenuation, and waxy pallor of the optic disc; (2) reduction in a- and b-wave amplitudes or nondetectable full-field electroretinogram; and (3) RP was the only disease causing VF damage. VF measurements were performed using the HFA with the 10-2 program and the Swedish Interactive Threshold Algorithm (SITA) Standard. Other inclusion criteria were as follows: (1) no previous ocular surgery except for cataract extraction and intraocular lens implantation; (2) no other diseases of the anterior and posterior segments of the eye that could affect VF, including cataracts, except for clinically insignificant senile cataracts; (3) logarithm of the minimum angle of resolution (logMAR) VA ≤ 2.0, and (4) age ≥20 years. Those with intraocular surgery, including cataract surgery, during the observation period were excluded. Reliability criteria for VFs were applied, including FLs of <20% and false-positive responses of <15%. Based on a previous report [22], FN rate was not applied as a reliability criterion, as suggested in the recommendation by the manufacturer. The VF of the left eye was mirror-imaged to that of the right eye for statistical analyses.
Visual acuity
All participants underwent measurements of subjective refraction and corneal dioptric power with an autokeratorefractometer without cycloplegia within 3 months of the VF measurement. VA was measured using a Landolt ring chart at a distance of 5 m from the illuminated target; each ring was presented one at a time. If the VA was not 20/20 or better, refractive correction was performed beginning with the results of autokeratorefractometry, and the corrective lenses were adjusted manually. The refractive error was measured in −0.25 D steps, and the cylindrical power was measured and recorded in negative form. The refractive error was determined according to the results of corrective lenses that provided the best-corrected VA [24]. VA was estimated as logMAR VA, and the examined eyes were divided into five subgroups according to logMAR VA (group 1: ≤0, group 2: >0 and ≤0.15, group 3: >0.15 and ≤0.35, group 4: >0.35 and ≤0.5, and group 5: >0.5).
Visual field
VF tests were undertaken using the HFA II (Carl Zeiss Meditec Inc.) with a Goldmann size III stimulus under standard perimetric conditions (background, 10 candela/m2) and the SITA Standard strategy.
Statistical analysis
VF sensitivities and VA
The Spearman rank test analysed the correlation between VA and different VF sensitivity measures, using the first VF of each patient: (1) the sensitivity of all 69 test points including foveal sensitivity in the HFA 10-2 VF, (2) the point with highest sensitivity from the fovea and central four points around the fovea in the HFA 10-2 VF (R2), (3) the point with highest sensitivity from the fovea and central 17 points in the 10-2VF (R3), and (4) the point with highest sensitivity from the fovea and central 37 points in the 10-2VF (R4). Thus, VF sensitivity measures (2)–(4) were chosen to gradually expand outward from the fovea. Correlation coefficients were compared using the Meng–Rosenthal–Rubin method [25], which tests the difference between two overlapping (having a variable in common) correlation coefficients, using a z-test.
VF reproducibility and VA
VF reproducibility was assessed using the root mean squared error (RMSE) of the measured threshold at each test point, as follows:
Then, the relationship between RMSE and FP, FN, FL, MD (mean deviation of the 1st and 2nd VFs), VA, and age, was analysed using linear modelling. All analyses were performed using the statistical programming language R (v2.15.1; The Foundation for Statistical Computing, Vienna, Austria).
Results
The demographics of the study subjects are summarized in Table 1. The mean age ± standard deviation [SD](range) of the study cohort was 51.0 ± 14.1 years (21–84). The MD value in the initial VF was –17.8 ± 9.0 (−35.2 to 0.1) and –17.7 ± 8.8 (−35.5 to −0.03) in the second VF. The pattern standard deviation (PSD) in the initial VF and second VF was 6.8 ± 2.7 (0.86 to 14.1) and 6.9 ± 2.7 (0.99 to 13.6), respectively. There were no significant differences in MD and PSD between paired VF tests (paired t test, p = 0.43 and 0.66, respectively).
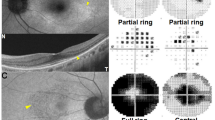
Spearman correlation coefficients between VA and each test point on the HFA 10-2 VF are illustrated in S1. R1, R2, R3, and R4 were −0.7200 (p < 0.01), −0.7274 (p < 0.01), −0.7220 (p < 0.01), and −0.7272 (p < 0.01), respectively (Fig. 1A–D), but these values were not significantly different (Meng–Rosenthal–Rubin method, p > 0.05).
A Sensitivity of foveal test point. B Test point with the highest sensitivity from the central five points in the 10-2 VF. C Test point with the highest sensitivity from the central 17 points in the 10-2 VF. D Test point with the highest sensitivity from the central 37 points in the 10-2 VF. There were no significant differences among the Spearman correlation coefficient values (Meng–Rosenthal–Rubin method, p > 0.05) VF visual field.
There was a significant relationship between RMSE and logMAR VA (RMSE = 3.7 + 1.63 × logMAR VA, R2 = 0.089, p < 0.001). The RMSE distribution in each VA group is shown in Fig. 2; the mean ± SD (range) was 3.6 ± 1.7 (1.2–13.1) in group 1 (logMAR VA ≤ 0), 4.1 ± 1.7 (1.5–11.6) in group 2 (logMAR VA > 0 and ≤0.15), 4.1 ± 1.3 (1.5–9.5) in group 3 (logMAR VA > 0.15 and ≤0.35), 3.9 ± 1.7 (1.0–6.8) in group 4 (logMAR VA > 0.35 and ≤0.5), and 4.8 ± 2.1 [2.0–10.6] in group 5 (logMAR VA > 0.5). The group 4 RMSE was significantly larger than that of group 1 (Tukey multiple comparison test: P < 0.001). However, there was no significant difference between the RMSE in group 1 versus groups 2, 3, and 4 (P = 0.52, 0.38, and 0.98, respectively), and in group 5 versus groups 2, 3, and 4 (P = 0.32, 0.25 and 0.43, respectively). The demographic characteristics of each VA group are shown in S2. Significant differences were observed between group 4 versus group 1 for age (P = 0.019) and groups 4, 3, and 2 versus group 1 for MD in the initial and second VF (p < 0.001).
The average rates of FL, FP, and FN are presented in Table 1. The average FN rate and logMAR VA were significantly associated with RMSE (both P < 0.001, multiple linear regression analysis, Table 2), but the average FL, FP, and age were not. This analysis was conducted in 191 eyes because FN was estimated as not applicable in 36 eyes (FN was not used as an as exclusion criterion, as recommended by the manufacturer: see Method section).
Discussion
Our study first investigated the relationships between visual sensitivity and VA. The association between visual sensitivity and VA was most tight at the fovea, becoming weak toward the peripheral region in an eccentric manner. Additionally, the association between visual sensitivity at the fovea and VA was not significantly improved by replacing the foveal sensitivity with the higher visual sensitivity around the fovea. Subsequently, we investigated the association between VF reproducibility and VA, revealing that the VF reproducibility appreciably increases as VA decreases, as shown in the significant relationship between RMSE and logMAR VA. Notably, reproducibility significantly decreased when logMAR VA was >1.0 compared with eyes with logMAR VA ≤ 0. (see Fig. 1), implying that a recommended cut-off value of logMAR VA > 0.5 be used as an inclusion criterion when using VF outcomes in research, not only in studies evaluating structure-function, progression prediction, and progression detection but also when defining the outcome of any observation/intervention. This is because, as Jansonius previously reported, the detection of disease progression is delayed in VFs with large variability [10, 26]. For instance, the time to detect progression with 80% power for an MD slope of −1.0 dB/year was 3 years when the SD of the MD was 0.5 dB (when VF was measured twice a year); however, this estimated duration rocketed to more than double (6.5 years) when the SD of the MD was 2.0 dB [10]. This duration was almost identical to when VF was measured annually, and the SD of the MD was 0.5 dB (6.0 years). Thus, careful consideration should be given when interpreting VF progression in eyes with logMAR VA > 0.5.
The clinical implications of the current results are as follows. The assessment of visual function is conducted using VF in RP. However, our results suggested clinicians can be warned that VF measurements are not reliable when logMAR VA was >1.0. This was in particular obvious when visual sensitivity around fovea is damaged, because it is directly associated with the deterioration of VA.
In this study, FN rate was significantly associated with the reproducibility of VFs, but FP and FL were not (Table 2). We previously analysed the relationship between VF (HFA 10-2 test) reproducibility and VF reliability indices, revealing that the FN, FL, and FP rates were useful in assessing VF reproducibility [27]. The reason for these contradicting results is unclear, but could be due to the wider range of FN rate in the current study (0–33.0%) compared with the previous study (0–19.5%) as well as the differences in sample size (227 and 42 eyes in the current and previous studies, respectively). An FN occurs when a patient fails to respond to a much more intense stimulus than they had responded to previously, and FNs are thought to represent inattention during the examination [28,29,30]. Although FN is no longer recommended for HFA by the manufacturers because it simply increases in accordance with VF deterioration [22], the results from this study suggest the usefulness of this parameter. Our recent studies suggested the usefulness of this index in estimating the accuracy of VF trend analysis [27] and VF reproducibility with the HFA 24-2 test [31], which further supports this standpoint.
FL and FP rates are considered indications of test reliability and vision fixation and “trigger-happy” patients, respectively [28,29,30]. However, some studies have suggested that the usefulness of these indices is limited [19,20,21], which agrees with the findings of our current study, where the rates were not significantly associated with VF reproducibility. Nonetheless, this does not totally negate the usefulness of these indices because we have previously reported their usefulness for estimating different purposes, such as over- or underestimation of VF in trend analysis [32] or structure-function relationships [33].
In contrast, logMAR VA was a significant parameter for VF reproducibility; reproducibility significantly decreased when logMAR VA was >0.5. This finding was very similar to the result in our previous study with the HFA 24-2 test in eyes with glaucoma [34], and the same cut-off level (logMAR >0.5) was suggested. Notably, this finding was observed despite some differences between these studies. VA was most strongly associated with foveal sensitivity in eyes with both glaucoma and RP, but the association was not improved by including the surrounding VF test points in eyes with RP, whereas it was significantly improved by including the 16 innermost VF test points in eyes with glaucoma. Thus, logMAR VA is more directly associated with foveal sensitivity in eyes with RP than in eyes with glaucoma. Additionally, the area with high association between logMAR VA and visual sensitivity expands more peripherally in the direction of the papillomacular bundle in eyes with glaucoma compared with eyes with RP. Eye fixation including such a region would have a poor VF reproducibility, regardless of the logMAR VA level.
In both RP and glaucoma, central visual function is usually preserved until late-stage disease. Reflecting this, a close relationship was observed between VA and foveal sensitivity in the current study (R = −0.72; Fig. 1A), similar to the previous study in glaucoma (R = −0.64) [35]. However, a considerable difference was observed in the association of the VF test points surrounding the fovea; it became weak toward the peripheral region in an eccentric manner. Additionally, the association between visual sensitivity at the fovea in the current study was in contrast to a strong correlation in the temporal paracentral area in eyes with glaucoma. This difference is probably because retinal nerve fibre layers in this area penetrate the optic disc margin at the temporal angle, which usually is less likely to be affected in cases of early to moderate glaucoma [36,37,38,39,40]. Indeed, we have proposed the clinical usefulness of VF clusters derived from the intercorrelation across VF test points in both RP and glaucoma. The mapping was concentric around the fovea in eyes with RP [41], whereas it reflected the mapping of the retinal nerve fibre distribution in eyes with glaucoma [42,43,44].
A limitation of the current study is that the results were not investigated using the HFA 24-2 test, and future studies using the HFA 24-2 should be undertaken. It would also be interesting to analyse the effect of parameters of optical coherence tomography, such as photoreceptor layer thickness, on VF reproducibility.
In conclusion, VA should be considered when assessing VF reproducibility. Specifically, careful consideration is necessary when logMAR VA is >0.5 because the reproducibility significantly increased beyond this level.
Summary
What was known before
-
The association between the reproducibility of the visual field and visual acuity has not been investigated in detail.
What this study adds
-
Reproducibility of visual field becomes poor with a decrease in visual acuity, in particular less than 0.5 logMAR in eyes with retinitis pigmentosa.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to the regulation at the ethics committees, but are available from the corresponding author on reasonable request.
References
Hartong DT, Berson EL, Dryja TP. Retinitis pigmentosa. Lancet. 2006;368:1795–809.
Narayan DS, Wood JP, Chidlow G, Casson RJ. A review of the mechanisms of cone degeneration in retinitis pigmentosa. Acta Ophthalmologica. 2016;94:748–54.
Abe K, Iijima H, Hirakawa H, Tsukahara Y, Toda Y. Visual acuity and 10 degrees automated static perimetry in eyes with retinitis pigmentosa. Jpn J Ophthalmol. 2002;46:581–5.
Swanson WH, Felius J, Birch DG. Effect of stimulus size on static visual fields in patients with retinitis pigmentosa. Ophthalmology. 2000;107:1950–4.
Kim LS, McAnany JJ, Alexander KR, Fishman GA. Intersession repeatability of humphrey perimetry measurements in patients with retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2007;48:4720–4.
Sayo A, Ueno S, Kominami T, Nishida K, Inooka D, Nakanishi A, et al. Longitudinal study of visual field changes determined by Humphrey Field Analyzer 10-2 in patients with Retinitis Pigmentosa. Sci Rep. 2017;7:16383.
Fujiwara K, Ikeda Y, Murakami Y, Tachibana T, Funatsu J, Koyanagi Y, et al. Aqueous flare and progression of visual field loss in patients with retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2020;61:26.
Flammer J, Drance SM, Fankhauser F, Augustiny L. Differential light threshold in automated static perimetry. Factors influencing short-term fluctuation. Arch Ophthalmol. 1984;102:876–9.
Flammer J, Drance SM, Zulauf M. Differential light threshold. Short- and long-term fluctuation in patients with glaucoma, normal controls, and patients with suspected glaucoma. Arch Ophthalmol. 1984;102:704–6.
Jansonius NM. On the accuracy of measuring rates of visual field change in glaucoma. Br J Ophthalmol. 2010;94:1404–5.
Berson EL, Rosner B, Sandberg MA, Weigel-DiFranco C, Moser A, Brockhurst RJ, et al. Further evaluation of docosahexaenoic acid in patients with retinitis pigmentosa receiving vitamin A treatment: subgroup analyses. Arch Ophthalmol. 2004;122:1306–14.
Berson EL, Rosner B, Sandberg MA, Weigel-DiFranco C, Moser A, Brockhurst RJ, et al. Clinical trial of docosahexaenoic acid in patients with retinitis pigmentosa receiving vitamin A treatment. Arch Ophthalmol. 2004;122:1297–305.
Hoffman DR, Locke KG, Wheaton DH, Fish GE, Spencer R, Birch DG. A randomized, placebo-controlled clinical trial of docosahexaenoic acid supplementation for X-linked retinitis pigmentosa. Am J Ophthalmol. 2004;137:704–18.
Hoffman DR, Hughbanks-Wheaton DK, Spencer R, Fish GE, Pearson NS, Wang YZ, et al. Docosahexaenoic Acid Slows Visual Field Progression in X-Linked Retinitis Pigmentosa: Ancillary Outcomes of the DHAX Trial. Invest Ophthalmol Vis Sci. 2015;56:6646–53.
Schwartz SG, Wang X, Chavis P, Kuriyan AE, Abariga SA. Vitamin A and fish oils for preventing the progression of retinitis pigmentosa. Cochrane Database Syst Rev. 2020;6:CD008428.
McMillan TA, Stewart WC, Hunt HH. Association of reliability with reproducibility of the glaucomatous visual field. Acta Ophthalmologica. 1992;70:665–70.
Katz J, Sommer A. Screening for glaucomatous visual field loss. The effect of patient reliability. Ophthalmology. 1990;97:1032–7.
Bengtsson B. Reliability of computerized perimetric threshold tests as assessed by reliability indices and threshold reproducibility in patients with suspect and manifest glaucoma. Acta Ophthalmol Scand. 2000;78:519–22.
Sanabria O, Feuer WJ, Anderson DR. Pseudo-loss of fixation in automated perimetry. Ophthalmology. 1991;98:76–8.
Demirel S, Vingrys AJ. Eye movements during perimetry and the effect that fixational instability has on perimetric outcomes. J Glaucoma. 1994;3:28–35.
Demirel S, Vingrys AJ Fixational instability during perimetry and the blindspot monitor. Perimetry Update 1992/1993. Kugler Publications: Amsterdam; 1992.
Bengtsson B, Heijl A. False-negative responses in glaucoma perimetry: indicators of patient performance or test reliability? Invest Ophthalmol Vis Sci. 2000;41:2201–4.
Artes PH, Iwase A, Ohno Y, Kitazawa Y, Chauhan BC. Properties of perimetric threshold estimates from Full Threshold, SITA Standard, and SITA Fast strategies. Investigative Ophthalmol Vis Sci. 2002;43:2654–9.
Sawada A, Tomidokoro A, Araie M, Iwase A, Yamamoto T. Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology. 2008;115:363–70.
Meng X-L, Rosenthal R, Rubin DB. Comparing correlated correlation coefficients. Psychological Bull Psychological Bull. 1992;111:172–5.
Chauhan BC, Garway-Heath DF, Goni FJ, Rossetti L, Bengtsson B, Viswanathan AC, et al. Practical recommendations for measuring rates of visual field change in glaucoma. Br J Ophthalmol. 2008;92:569–73.
Asaoka R, Fujino Y, Aoki S, Matsuura M, Murata H. Estimating the Reliability of Glaucomatous Visual Field for the Accurate Assessment of Progression Using the Gaze-Tracking and Reliability Indices. Ophthalmol Glaucoma. 2019;2:111–9.
Fankhauser F, Spahr J, Bebie H. Some aspects of the automation of perimetry. Surv Ophthalmol. 1977;22:131–41.
Anderson DR, Patella VM. Automated Static Perimetry. 2nd ed. Mosby: St. Louis; 1999.
Johnson CA, Sherman K, Doyle C, Wall M. A comparison of false-negative responses for full threshold and SITA standard perimetry in glaucoma patients and normal observers. J Glaucoma. 2014;23:288–92.
Ishiyama Y, Murata H, Mayama C, Asaoka R. An objective evaluation of gaze tracking in Humphrey perimetry and the relation with the reproducibility of visual fields: a pilot study in glaucoma. Investigative Ophthalmol Vis Sci. 2014;55:8149–52.
Ishiyama Y, Murata H, Asaoka R. The Usefulness of Gaze Tracking as an Index of Visual Field Reliability in Glaucoma Patients. Investigative Ophthalmol Vis Sci. 2015;56:6233–6.
Ishiyama Y, Murata H, Hirasawa H, Asaoka R. Estimating the Usefulness of Humphrey Perimetry Gaze Tracking for Evaluating Structure-Function Relationship in Glaucoma. Investigative Ophthalmol Vis Sci. 2015;56:7801–5.
Matsuura M, Hirasawa K, Murata H, Asaoka R. The Relationship Between Visual Acuity and the Reproducibility of Visual Field Measurements in Glaucoma Patients. Investigative Ophthalmol Vis Sci. 2015;56:5630–5.
Asaoka R. The relationship between visual acuity and central visual field sensitivity in advanced glaucoma. Br J Ophthalmol. 2013;97:1355–6.
Su D, Park SC, Simonson JL, Liebmann JM, Ritch R. Progression Pattern of Initial Parafoveal Scotomas in Glaucoma. Ophthalmology. 2013;120:520–27.
Koseki N, Araie M, Yamagami J, Suzuki Y. Sectorization of central 10-deg visual field in open-angle glaucoma. An approach for its brief evaluation. Graefe’s Arch Clin Exp Ophthalmol = Albrecht von Graefes Arch fur klinische und experimentelle Ophthalmologie. 1995;233:621–6.
Weber J, Schultze T, Ulrich H. The visual field in advanced glaucoma. Int Ophthalmol. 1989;13:47–50.
Hood DC, Kardon RH. A framework for comparing structural and functional measures of glaucomatous damage. Prog Retin Eye Res. 2007;26:688–710.
Hood DC, Raza AS, de Moraes CG, Johnson CA, Liebmann JM, Ritch R. The Nature of Macular Damage in Glaucoma as Revealed by Averaging Optical Coherence Tomography Data. Transl Vis Sci Technol. 2012;1:3.
Omoto T, Oishi A, Asaoka R, Fujino Y, Murata H, Azuma K, et al. Development and validation of a visual field cluster in retinitis pigmentosa. Sci Rep. 2021;11:9671.
Hood DC, Raza AS, de Moraes CG, Liebmann JM, Ritch R. Glaucomatous damage of the macula. Prog Retin Eye Res. 2013;32:1–21.
de Moraes CG, Song C, Liebmann JM, Simonson JL, Furlanetto RL, Ritch R. Defining 10-2 visual field progression criteria: exploratory and confirmatory factor analysis using pointwise linear regression. Ophthalmology. 2014;121:741–9.
Asaoka R. Mapping glaucoma patients’ 30-2 and 10-2 visual fields reveals clusters of test points damaged in the 10-2 grid that are not sampled in the sparse 30-2 grid. PLoS ONE. 2014;9:e98525.
Funding
This study was supported, in part, by grants (numbers 19H01114, 18KK0253, 20K09784, 20768254, and 80635748) from the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Translational Research program; the Strategic Promotion for Practical Application of Innovative Medical Technology (TR-SPRINT) from the Japan Agency for Medical Research and Development (AMED); an AIP Acceleration Research grant from the Japan Science and Technology Agency; and a grant from the Japanese Retinitis Pigmentosa Society (JRPS).
Author information
Authors and Affiliations
Contributions
RA contributed the conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualisation, writing – original draft, and writing – review & editing. MM, AO, YF, HM, KA, RO and TA contributed methodology and the resources and writing – review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41433_2022_2043_MOESM1_ESM.tif
S1 - Spearman correlation coefficients between visual acuity and visual field (VF) sensitivity in the 24-2 and 10-2 VFs.
Rights and permissions
About this article
Cite this article
Asaoka, R., Miyata, M., Oishi, A. et al. Relationship between visual acuity and visual field and its reproducibility in patients with retinitis pigmentosa. Eye 37, 1094–1099 (2023). https://doi.org/10.1038/s41433-022-02043-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02043-0