Abstract
Small-aperture corneal inlays, commonly known as KAMRA, are tiny optical devices inserted in the corneal stroma aiming to gain near vision in patients with presbyopia. The purpose of this study was to systematically review case series of small-aperture corneal inlays performed in presbyopic emmetropic patients and to evaluate the visual outcomes of this procedure. This systematic review included 18 articles published between 2011 and 2018, overall studying 2724 eyes from 2691 participants. The mean longest follow-up was 19 months. Results showed that 78.5% of eyes reported an uncorrected near visual acuity of 20/32 or better and 90.50% of eyes achieved an uncorrected distance visual acuity of 20/25 or better. All patients experienced an improvement in uncorrected near visual acuity with a patient satisfaction ranging between 60% and 90%. The highlighted complications were keratocyte activation leading to corneal stromal haze, epithelial growth, iron deposits and poor distance visual acuity. Explantation was carried out in 101 eyes (3.7%) due to distance vision blurriness, development of epithelial microcysts, incorrect implant placement or hyperopic shift changes. KAMRA demonstrated high efficacy. However, safety and satisfaction rates remain unclear. Despite the low explantation rates reported in the literature, some complications were permanent. The results and conclusions should be taken with caution due to the conflict of interest stated in the reviewed articles.
摘要
小切口角膜镶嵌术又称为KAMRA, 是在角膜基质中植入微小光学植片 (Kamra), 旨在让老视患者提高近视力。本研究旨在系统性回顾在正视性老视患者中使用小切口角膜镶嵌术治疗的系列病例, 并评价该手术的视力结局。这项系统回顾性纳入了2011至2018年间的18篇已发表文献, 纳入2691位患者的2724只眼。平均最长随访时间为19个月。结果表明, 78.5%的患眼提升裸眼近视力至20/32或更好, 90.50%的患眼提升裸眼远视力至20/25或更好。所有患者的裸眼近视力均有所改善, 患者满意度为60%-90%。该手术突出的并发症是角膜细胞活化导致的角膜基质浑浊, 上皮增生, 铁质沉积和远视力下降。101只眼(3.7%)因出现远视力模糊、上皮微囊、植片位置不正确或远视漂移而取出角膜植片。 KAMRA对于治疗正视性老视有很好的疗效。然而, KAMRA的安全性和满意度仍不清楚。尽管文献中报告的取出率较低, 一些并发症是永久性的。由于所纳入文章中的利益冲突, 应谨慎使用文章的结果和结论。
Similar content being viewed by others
Introduction
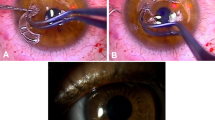
Presbyopia is the most common refractive error and its prevalence continues to increase every year [1]. Corneal inlay implantation devices are placed in the cornea in a monocular fashion, improving near and intermediate visual acuity while maintaining distance vision [2]. They are placed in a stromal pocket that is previously created using either femtosecond laser or mechanically using a microkeratome. This surgical procedure can be performed by either varying the corneal refractive index [3, 4] or by modifying the corneal curvature [3, 4]. However, the small-aperture intracorneal inlay (KAMRA™, AcuFocus Inc., Irvine, CA, USA) [5] has a pinhole mechanism. It should be remarked that the implanted lens does not have a refractive power, rather it achieves its effect by raising the centre of the cornea [6].
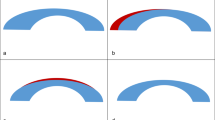
Small-aperture corneal inlay (SACI), commonly known as KAMRA corneal inlay, is a micro-drilled opening device with a diameter of 3.8 mm and a centre hole of 1.6 mm [7]. It is made of polyvinylidene fluoride and carbon nanoparticles, and it is placed within the stroma in a corneal pocket in the non-dominant eye. It works by allowing a channel light through the small opening and blocking the unfocused light from passing through the periphery, hence increasing the depth of focus as the central opening has a pinhole effect [7]. However, as it partially blocks light, it could influence in visual performance [8]. The visual experience in the patient is different from monovision in which one eye is corrected for distance vision and the other for near vision [9]. The KAMRA inlay is opaque and has 8400 pores that allow the passage of nutrients to avoid weight loss and epithelial problems, as well as to maintain the viability of the anterior stromal lamella [10]. It is designed to allow light to pass through the pupil due to its central opening, which blocks incident light and out-of-focus light from the periphery. The inlay yields a monocular pinhole effect but permits maintenance of binocular summation [7].
The purpose of this study was to systematically review case series of SACI performed in emmetropic presbyopic patients in order to evaluate the visual outcomes, postoperative complications and explantation reasons.
Methods
This systematic review was carried out by searching in PubMed, Web of Science and Scopus data bases on February 12, 2020. The study was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement recommendations [11]. An initial search was conducted, focused on obtaining case studies of corneal inlays in presbyopic patients. The keywords used were “SACI” and “KAMRA inlay”. From them, a total of 88 articles were identified, which were evaluated and selected according to inclusion and exclusion criteria. The inclusion criteria were: (1) KAMRA inlay implantation in emmetropic presbyopic patients with or without prior surgery. The exclusion criteria were: (2) narrative reviews; (3) animal studies; (4) non-English publications; (5) publications in which SACI was not performed exclusively (i.e. combined with myopic, hyperopic or astigmatism LASIK); (6) articles without findings or conclusions; (7) articles with a number of patients less or equal than 5; (8) articles in non-indexed scientific journals.
The following data was summarized in tables; (1) authors and year of publication, (2) study design, (3) maximum follow-up period expressed in months, (4) number of patients, (5) number of eyes implanted, (6) sex, (7) intrastromal flap/pocket creation technique (mechanical microkeratome or femtosecond laser), (8) pocket depth (expressed in microns, µm), (9) past medical history, namely previous surgeries, (10) visual postoperative improvements of uncorrected near visual acuity (UNVA), uncorrected intermediate visual acuity (UIVA) and uncorrected distance visual acuity (UDVA), (11) patient satisfaction rate, expressed in percentage, (12) postoperative complications after SACI (repeated cases were excluded from explantation rate), (13) explantation rate; in studies with KAMRA inlay explantation, percentage of eyes were reported in brackets, and finally, (14) explantation reason. To assess the risk of bias of the included studies, a summary table was elaborated (Table 1) based on the Quality Assessment Tool for Case Series Studies from the National Heart, Lung, and Blood Institute [12]. The questions included in the tool were (1) Is the study oriented to a clear question?; (2) Were all the patients results taken into account?; (3) Was the follow-up complete?; Were the same conditions used in surgical treatment?; (5) Was the intervention clearly described?; (6) Was the duration of follow-up adequate?; (7) Were the results described correctly? This analysis did not result in the exclusion of any article. However, articles with a higher risk of bias had a lower weight for the data synthesis. Risk of bias was assessed by I.PJ and J-MSG. In case of disagreements, C.RDL decided the tie-breaker.
Results
The selection process of this systematic review was presented with a flow chart diagram in Fig. 1. A total of eighteen articles [9, 10, 13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28] published between 2011 and 2018 were included in this systematic review. All of them were case series studies. Patients completing the inclusion criteria were presbyopic between 45 and 60 years old, with a preoperative manifest spherical equivalent refraction defined as −0.75D to +0.50D, with no more than −0.75D of refractive cylinder, and UNVA of 20/100–20/40 (Snellen scale) or 0.7–0.3 (Logarithm of the Minimum Angle of Resolution, LogMAR scale). Near addition target was between +1.00 dioptres (D) and +2.50 D, minimum central corneal thickness (CCT) was established as 500 µm for most of the articles, a minimum central endothelial cell count of 2000 cells/mm2 or more, and a corneal power from 41.00 D to 47.00 D in all meridians. According to exclusion criteria, patients with anterior or posterior segment disease, any type of immunodeficiency disorder, patients using systemic medications with associated side effects, and those with latent hyperopia were not included. Patient and surgery details of the selected articles were reported in Table 2.
This systematic review included 2724 eyes from a total of 2691 patients, and a maximum postoperative follow-up that ranged from 3 to 60 months, with a mean maximum follow-up of 19 months. Fifteen articles [9, 10, 13,14,15,16,17,18,19, 21, 24,25,26,27,28] used femtosecond laser for intrastromal pocket creation, two [20, 22] of them used mechanical microkeratome and one [23] did not report the surgical technique. The pocket depth ranged from 150 µm to 280 µm and the mean pocket depth was 202 µm. Results after SACI were presented in Table 3. Concerning previous ocular history of patients, there were 14 articles [9, 10, 14,15,16,17,18,19, 21,22,23, 25, 27, 28] that studied emmetropic presbyopic patients and four articles [13, 20, 24, 26] that studied the combination with previous cataract surgery or LASIK. There were no statistically significant differences in terms of the results obtained among the patients with or without previous surgery. In the postoperative period, there was a remarkable improvement in UNVA and UIVA. In the last follow-up appointment, UNVA ranged between 44% to 100% of eyes with 20/32 or better (J2, Jaeger), with a mean UNVA of 20/32 or better in 78.50% of eyes. UIVA was reported in only five studies [15,16,17, 23, 25] and ranged between 87% to 100% of eyes with 20/32 or better. Mean UIVA was 91.80%. UDVA ranged between 65% to 100% with 20/25 or better and ranged between 65% to 100%, with a mean UDVA of 90.50% of eyes with 20/25 or better. The exact distances in which UDVA, UIVA and UNVA were measured were not reported in the included articles.
Regarding complications, keratocyte activation, corneal oedema, haze, stromal thinning, iron deposits and dystrophies were reported. These issues were responsible for the explanted inlays and were the cause of the visual complaints and hyperopic changes. The number of explanted KAMRAs were 101 (3.7% from total implanted). Furthermore, 6 articles [9, 10, 18, 19, 24, 25] offered information on patient satisfaction and the overall percentage was between 60% and 90%. Finally, the included studies were grouped into three levels based on the risk of bias assessment tool. The groups were: low evidence (affirmative answers = 0–2); medium evidence (affirmative answers = 3 to 5); and high evidence (affirmative answers = 6–7). No studies reported low evidence level. Moshirfar et al. [22], Moshirfar et al. [24], Huseynova et al. [26], Tomita & Huseynova [13] and Waring [19] achieved a medium evidence level. Moshirfar et al. [21], Vukich et al. [9], Linn et al. [23], Dexl et al. [25], Abbouda et al. [27], Agca et al. [14], Tomita et al. [28], Dexl et al. [17], Dexl et al. [10], Seyeddain et al. [15], Seyeddain et al [16]. Dexl et al. [18] and Yımaz et al. [20], obtained a high evidence level.
Discussion
Visual outcomes
Postoperative results after this surgical technique proved an increase in distance visual acuity. UNVA improved in 78.5% of eyes to J2 or better. UIVA, only described in five articles [9, 15,16,17, 25], improved in 91.80% of eyes to 20/32 or better, and UDVA was shown to improve in 90.50% of eyes to 20/25 or better. The UNVA improvement had a slight effect on the UDVA. To achieve better visual outcomes, positioning and centring must be precise. An off-centre of only 0.5 mm may reduce the image quality [29, 30] since the opening would not be aligned with patient’s visual axis hence implying a new surgical procedure [31]. Usually, a femtosecond laser was used to create an intrastromal pocket which works using the photo disruption principle, emitting infra-red pulses and achieving tissue separation at the molecular level without impacting surrounding tissue. However, there were two cases that were performed with mechanical microkeratome [20, 22]. According to various authors [32, 33], femtosecond laser should be used to obtain better results in surgery. Mechanical microkeratome should be avoided due to its imprecision and its worse results [34]. However, this systematic review did not observe significant differences among both techniques.
Complications
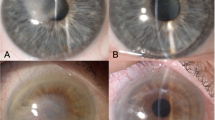
Cases of corneal oedema, blurring, stromal thinning, flap striae, epithelial growth [35] or iron deposits were some of the complications experienced by the patients included in the studies. Although the mentioned complications were localized near the Bowman’s membrane, they did not influence vision and they did not influence the refractive results. In addition, they occurred less frequently in implants with reduced thickness and a greater number of pores [36]. Another frequent postoperative complication was keratocyte activation that led to corneal haze [37], therefore reducing near and intermediate visual acuity. Cases requiring explantation experienced persistent corneal haze postoperatively and preoperative visual acuity was not recovered. To avoid postoperative haze, it is proposed to use lower laser energy or to increase steroid treatment [27]. Contrast sensitivity remained within normal ranges [38] and stereopsis was compromised in some patients, mainly in poor lighting enviroments [23]. In this review, there were patients who presented topographic changes. Some of them developed hyperopic changes [24, 25], which seemed to be associated with shallower inlays. Therefore, the ideal placement of KAMRA inlay is at a depth between 250 and 350 µm [10, 17, 24]. The recommended residual stroma bed is established at 250 µm. It should be noted that there was no significant induction of astigmatism in any meridian [8].
Safety
One hundred one eyes from a total of 2692 (without repeated cases in Dexl et al. [18] and Dexl et al. [25]) required inlay explantation. The inlay implantation did not reduce corneal thickness. Consequently, it seems that it can be used in patients who have previously been laser corrected and in pseudophakic patients. Previous results suggest that there are no differences between visual outcomes of virgin eyes and eyes with previous ocular surgery [24]. Patients in this study who had previously been corrected with LASIK reported a pocket depth between 170 and 250 µm. None of the cases studied placed KAMRA inlay in the LASIK flap. No significant differences were observed between men and women. Devices can be easily removed when required. Alió et al. [39] reported that it has a minimal impact on corneal topography and aberrometry during and after recovery when extraction occurs within six months of its implantation. However, changes may be permanent if explantation is performed after this period [7]. Although a longer follow-up could be necessary, most patients, between 60% and 90%, expressed a high satisfaction rate. Moreover, the explantation rate reported was between 1.8% and 33.4%, an average of 3.7% of eyes. After explantation, most patients recovered the near and intermediate visual acuity they had prior to implantation, but there is a risk of not being able to achieve the preoperative UDVA [40]. The long-term safety is therefore concerning and corneal inflammation requiring the inlay explantation is often not reversible resulting in significant scarring and visual impairment. Repositioning or reimplanting the corneal inlay could be an option for retreatment procedures in order to achieve the desirable refractive result once it has been removed. The main reasons for explantation were incorrect implant placement [41, 42], blurring and refractive changes [43].
Strengths and limitations
To the best of our knowledge, this is the first systematic review of SACI available in the scientific literature. The PRISMA method improves the evidence level available to date. Within the limitations, only eighteen studies could enrol this review, there is a lack of literature regarding randomized clinical trials comparing KAMRA with other corneal inlays, and many articles were published by the same researchers. Satisfaction rate relevance was limited since only one third of the studies provided this information. In the same way, there is a great heterogeneity in the follow-up and therefore it should be standardized. In addition, six studies [10, 15,16,17,18, 25] that reported the best outcomes among the included studies in this review have a risks of bias. For instance, Acufocus Inc., Irvine, California, USA, financially supported the research, authors received travel expenses from Acufocus, and other authors work as clinical specialists for Acufocus. Therefore, sixteen from eighteen studies reported conflict of interest with AcuFocus. Thus, we allow readers to weigh the results and conclusions of this systematic review. In addition, in some articles [10, 17, 18, 21, 22, 24, 25] the follow-up length match with the progressively publication date. Therefore, some eyes could have been included in more than one paper making the total eye sample lower than 2724. However, it was impossible to calculate it in this study.
SACI outcomes achieved a high efficacy and satisfaction rate, although its safety is still questionable. The inlay improves near and intermediate vision with slight effect on visual acuity at distance. Furthermore, the inlay may be explanted when necessary, although the visual acuity may not improve to the preoperative state. Surgical process, patient selection and pocket or flap depth are essential for successful surgery outcomes.
Data availability
Data are available on demand.
References
Moarefi MA, Bafna S, Wiley W. A review of presbyopia treatment with corneal inlays. Ophthalmol Ther. 2017;6:55–65.
Duignan ES, Farrell S, Treacy MP, Fulcher T, O’Brien P, Power W, et al. Corneal inlay implantation complicated by infectious keratitis. Br J Ophthalmol. 2016;100:269–73.
Parkhurst GD, Garza EB, Medina AA. Femtosecond laser-assisted cataract surgery after implantation of a transparent near vision corneal inlay. J Refract Surg. 2015;31:206–8.
Garza EB, Gomez S, Chayet A, Dishler J. One-year safety and efficacy results of a hydrogel inlay to improve near vision in patients with emmetropic presbyopia. J Refract Surg. 2013;29:166–72.
Elling M, Schojai M, Schultz T, Hauschild S, Burkhard Dick H. Implantation of a corneal inlay in pseudophakic eyes: A prospective comparative clinical trial. J Refract Surg. 2018;34:746–50.
Binder PS. Intracorneal inlays for the correction of presbyopia. Eye Contact Lens. 2017;43:267–75.
Naroo SA, Bilkhu PS. Clinical utility of the KAMRA corneal inlay. Clin Ophthalmol. 2016;10:913–9.
Burkhard Dick H. Small-aperture strategies for the correction of presbyopia. Curr Opin Ophthalmol. 2019;30:236–42.
Vukich JA, Durrie DS, Pepose JS, Thompson V, van de Pol C, Lin L. Evaluation of the small-aperture intracorneal inlay: three-year results from the cohort of the U.S. Food and Drug Administration clinical trial. J Cataract Refract Surg. 2018;44:541–56.
Dexl AK, Seyeddain O, Riha W, Rückl T, Bachernegg A, Emesz M, et al. Reading performance and patient satisfaction after corneal inlay implantation for presbyopia correction: two-year follow-up. J Cataract Refract Surg. 2012;38:1808–16.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
National Heart, Lung and BI (NHLBI). Quality assessment tool for observational cohort and cross-sectional studies. Bethesda, MD: Natl. Institutes Heal. Dep. Heal. Hum. Serv; 2014. p. 1–4.
Tomita M, Huseynova T. Evaluating the short-term results of KAMRA inlay implantation using real-time optical coherence tomography-guided femtosecond laser technology. J Refract Surg. 2014;30:326–9.
Agca A, Demirok A, Çelik HU, Van De Pol C, Çankaya KI, Çelik NB, et al. Corneal hysteresis, corneal resistance factor, and intraocular pressure measurements in eyes implanted with a small aperture corneal inlay. J Refract Surg. 2014;30:831–6.
Seyeddain O, Bachernegg A, Riha W, Rückl T, Reitsamer H, Grabner G, et al. Femtosecond laser-assisted small-aperture corneal inlay implantation for corneal compensation of presbyopia: two-year follow-up. J Cataract Refract Surg. 2013;39:234–241.
Seyeddain O, Hohensinn M, Riha W, Nix G, Rückl T, Grabner G, et al. Small-aperture corneal inlay for the correction of presbyopia: 3-year follow-up. J Cataract Refract Surg. 2012;38:35–45.
Dexl AK, Seyeddain O, Riha W, Hohensinn M, Rückl T, Reischl V, et al. One-year visual outcomes and patient satisfaction after surgical correction of presbyopia with an intracorneal inlay of a new design. J Cataract Refract Surg. 2012;38:262–9.
Dexl AK, Seyeddain O, Riha W, Hohensinn M, Hitzl W, Grabner G. Reading performance after implantation of a small-aperture corneal inlay for the surgical correction of presbyopia: two-year follow-up. J Cataract Refract Surg. 2011;37:525–31.
Waring GO IV. Correction of presbyopia with a small aperture corneal inlay. J Refract Surg. 2011;27:842–5.
Ylmaz ÖF, Alagöz N, Pekel G, Azman E, Aksoy EF, Çakr H, et al. Intracorneal inlay to correct presbyopia: Long-term results. J Cataract Refract Surg. 2011;37:1275–81.
Moshirfar M, Desautels JD, Walker BD, Birdsong OC, Skanchy DF, Quist TS, et al. Long-term changes in keratometry and refraction after small aperture corneal inlay implantation. Clin Ophthalmol. 2018;12:1931–8.
Moshirfar M, Desautels JD, Wallace RT, Koen N, Hoopes PC. Comparison of FDA safety and efficacy data for KAMRA and raindrop corneal inlays. Int J Ophthalmol. 2017;10:1446–51.
Linn SH, Skanchy DF, Quist TS, Desautels JD, Moshirfar M. Stereoacuity after small aperture corneal inlay implantation. Clin Ophthalmol. 2017;11:233–5.
Moshirfar M, Quist TS, Skanchy DF, Wallace RT, Linn SH, Hoopes PC. Six-month visual outcomes for the correction of presbyopia using a small-aperture corneal inlay: Single-site experience. Clin Ophthalmol. 2016;10:2191–8.
Dexl AK, Jell G, Strohmaier C, Seyeddain O, Riha W, Rückl T, et al. Long-term outcomes after monocular corneal inlay implantation for the surgical compensation of presbyopia. J Cataract Refract Surg. 2015;41:566–75.
Huseynova T, Kanamori T, Waring GO, Tomita M. Outcomes of small aperture corneal inlay implantation in patients with pseudophakia. J Refract Surg. 2014;30:110–5.
Abbouda A, Javaloy J, Alió JL. Confocal microscopy evaluation of the corneal response following AcuFocus KAMRA inlay implantation. J Refract Surg. 2014;30:172–8.
Tomita M, Kanamori T, Waring GO IV, Huseynova T. Retrospective evaluation of the influence of pupil size on visual acuity after KAMRA inlay implantation. J Refract Surg. 2014;30:448–53.
Manzanera S, Webb K, Artal P. Adaptation to brightness perception in patients implanted with a small aperture. Am J Ophthalmol. 2019;197:36–44.
Artal P, Manzanera S. Perceived brightness with small apertures. J Cataract Refract Surg. 2018;44:734–7.
Arlt EM, Krall EM, Moussa S, Grabner G, Dexl AK. Implantable inlay devices for presbyopia: the evidence to date. Clin Ophthalmol. 2015;9:129–37.
Xia LK, Yu J, Chai GR, Wang D, Li Y. Comparison of the femtosecond laser and mechanical microkeratome for flap cutting in LASIK. Int J Ophthalmol. 2015;8:784–90.
Chen S, Feng Y, Stojanovic A, Jankov MR, Wang Q. Intralase femtosecond laser vs mechanical microkeratomes in LASIK for myopia: A systematic review and meta-analysis. J Refract Surg. 2012;28:15–24.
Igras E, O’Caoimh R, O’Brien P, Power W. Long-term results of combined LASIK and monocular small-aperture corneal inlay implantation. J Refract Surg. 2016;32:379–84.
Antonios R, Jabbur NS, Ahmed MA, Awwad ST. Refractory interface haze developing after epithelial ingrowth following laser in situ keratomileusis and small aperture corneal inlay implantation. Am J Ophthalmol Case Rep. 2018;10:10–2.
Alió JL, Wolter NV, Piñero DP, Amparo F, Sari ES, Cankaya C, et al. Pediatric refractive surgery and its role in the treatment of amblyopia: Meta-analysis of the peer-reviewed literature. J Refract Surg. 2011;27:364–74.
Romito N, Basli E, Goemaere I, Borderie V, Laroche L, Bouheraoua N. Persistent corneal fibrosis after explantation of a small-aperture corneal inlay. J Cataract Refract Surg. 2019;45:367–71.
Lin L, Van De Pol C, Vilupuru S, Pepose JS. Contrast sensitivity in patients with emmetropic presbyopia before and after small-aperture inlay implantation. J Refract Surg. 2016;32:386–93.
Alió JL, Abbouda A, Huseynli S, Knorz MC, Homs MEM, Durrie DS. Removability of a small aperture intracorneal Inlay for presbyopia correction. J Refract Surg. 2013;29:550–6.
Moshirfar M, Skanchy DF, Rosen DB, Heiland MB, Liu HY, Buckner B, et al. Visual prognosis after explantation of small-aperture corneal inlays in presbyopic eyes: a case series. Med Hypothesis Discov Innov Ophthalmol J. 2019;8:129–33.
Hoopes PC, Walker BD, Birdsong OC, Moshirfar M. Small-aperture corneal inlay repositioning. J Cataract Refract Surg. 2018;44:3–5.
Gatinel D, El Danasoury A, Rajchles S, Saad A. Recentration of a small-aperture corneal inlay. J Cataract Refract Surg. 2012;38:2186–91.
Amigó A, Martinez-Sorribes P, Recuerda M. Late-onset refractive shift after small-aperture corneal inlay implantation. J Cataract Refract Surg. 2018;44:658–64.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design: I.P-J, C.R-d-L, R.R-A and J-M.S-G; data collection: I.P-J, C.R-d-L, R.R-A and J-M.S-G; analysis and interpretation of results: I.P-J, C.R-d-L, R.R-A and J-M.S-G. Author; draft manuscript preparation: I.P-J, C.R-d-L, R.R-A and J-M.S-G. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was conducted in accordance with the tenets of the Helsinki Declaration and obtained Institutional Review Board approval.
Consent for publication
All patients included in this work were adequately informed verbally and in writing of the benefits, characteristics, and risks of the surgeries. All patients signed an informed consent prior to the surgery and after the interview performed with the ophthalmologist.
Consent to participate
All authors consent publication of this article.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pluma-Jaramago, I., Rocha-de-Lossada, C., Rachwani-Anil, R. et al. Small-aperture intracorneal inlay implantation in emmetropic presbyopic patients: a systematic review. Eye 36, 1747–1753 (2022). https://doi.org/10.1038/s41433-022-02032-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02032-3