Abstract
Objective
To investigate practice patterns and clinical outcomes in the repair of uncomplicated rhegmatogenous retinal detachments (RRD) in a real-world setting over a 10-year period.
Methods
We compared preferences for scleral buckling (SB), pars plana vitrectomy (PPV), PPV/SB, or pneumatic retinopexy (PR) over time, and examined the 1-year single surgery anatomic success (SSAS) and best-corrected visual acuity (BCVA) at a tertiary academic institution from 2008–2018.
Results
Eight hundred eight eyes had RRD repair between 2008–2011 (n = 240), 2012–2014 (n = 271), and 2015–2017 (n = 297). Compared to 2008–2011, PPV was preferred over SB in 2012–2014 (OR: 2.93; 95% CI: 1.86–4.63) and 2015–2017 (OR: 5.94; 95% CI: 3.76–9.38), and over PPV/SB in 2012–2014 (OR: 2.74; 95% CI: 1.65–4.56) and 2015–2017 (OR: 3.16; 95% CI: 31.96–5.12). PR was uncommonly utilized (<10%). Younger surgeons (graduating 2010–2017) favored PPV over SB when compared to older surgeons [graduating 1984–2000 (OR: 1.77; 95% CI: 1.18–2.65) and 2001–2009 (OR 1.73; 95% CI: 1.14–2.65)], but similarly selected PPV vs. PPV/SB as their older counterparts (p > 0.05). Compared to PPV, SSAS was higher with SB (OR: 1.53; 95% CI: 1.03–2.26) and PPV/SB (OR: 2.55; 95% CI: 1.56–4.17). One-year BCVA was markedly improved compared to baseline only for eyes that achieved SSAS (p < 0.001).
Conclusions
Over the past 10 years, PPV has become the favored approach to repair uncomplicated RRD and this appears to be driven by younger surgeons’ preferences. Given the superior long-term SSAS in SB and PPV/SB as compared to PPV, SB and PPV/SB should be more frequently considered when determining the appropriate repair strategy for uncomplicated RRD.
Similar content being viewed by others
Introduction
In 1929, Gonin successfully repaired a rhegmatogenous retinal detachment (RRD) by surrounding retinal breaks with Paqueline thermocautery, and thus proved that sealing retinal tears was essential for successful repair of RRD [1]. Since then, several approaches have emerged for treating RRDs, including scleral buckling (SB) in the 1950s [2], pars plana vitrectomy (PPV) in the 1970s [3], and pneumatic retinopexy (PR) in the 1980s [4].
SB was the gold standard for RRD repair for more than 60 years and remained so even after the introduction of PPV. PPV was initially considered high-risk surgery and was reserved for complicated RRDs, such as giant retinal tear or proliferative vitreoretinopathy. PPV became popular after the introduction of transconjunctival small gauge instruments in the 2000s [5]. PPV is now selected over SB among Medicare and commercially insured patients [6, 7]. Likewise, PPV is now preferred over SB and PPV/SB in Singapore [8], Spain [9], and Austria [10]. The factors driving this evolution in practice pattern based on a comprehensive analysis of patient and ocular characteristics are unclear. Likewise, prior studies assessing RRD repair have had short postoperative follow-up, such that the long-term success of these surgical choices is uncertain.
In this study, we investigated the practice pattern change for managing uncomplicated primary RRDs at a single academic institution over a ten-year period. We also compared the variation in practice trends among subgroups of patients with diverse demographics and ocular characteristics and examined differences in vitreoretinal surgeons’ practice patterns based on year of fellowship graduation. Lastly, we compared anatomic and visual acuity outcomes among the different RRD repair procedures in patients with 1 year of postoperative follow-up.
Methods
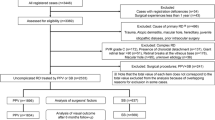
This study was approved by the Institutional Review Board of Johns Hopkins University School of Medicine. The study adhered to the Declaration of Helsinki and is Health Insurance Portability and Accountability Act compliant. A retrospective chart review, which included records between January 1, 2008 and December 31, 2018, was conducted. Four thousand nine hundred and seventy-four charts were identified using the following codes: ICD-9 codes 361.00, 361.03, 361.02, 361.91 and ICD-10 codes H33.00-, H33.03-, H33.02-, H33.01-; CPT codes 67101, 67105, 67107, 67108, 67110, 67113, 67115, 67120, 67121.
The study included patients 18 years and older who underwent primary repair of uncomplicated RRD at the Wilmer Eye Institute within the study period with at least one-year follow-up. Exclusion criteria include complex RRD with proliferative vitreoretinopathy (PVR) grade C or worse, presence of giant retinal tear, tractional retinal detachment, history of globe rupture, as well as surgical interventions for infectious or inflammatory aetiologies, epiretinal membrane, macular hole-related detachments, and retinoschisis-related detachments.
Patient, ocular, and RRD characteristics including age at presentation, gender, race, myopia, refractive error, prior trauma, history of RRD in the contralateral eye, prior intraocular surgery and type of surgery, lens status, best-corrected visual acuity, intraocular pressure, foveal and macular involvement, extent and location of detachment, characteristics of retinal breaks, inferior location of retinal breaks (defined as 4–8 o’clock), presence of lattice degeneration were collected. The type of repair (SB, PPV, SB/PPV, and PR) and year of repair were recorded. The attending surgeon’s fellowship graduation year was also collected. Single surgery anatomic success (SSAS) was defined as retinal reattachment without any additional procedures after the first repair procedure.
Statistical analyses were completed using RStudio (R version 4.0.2), Stata (version 16.0), and JMP Pro (version 14.0). Chi-square and Fisher’s exact test were used for categorical variables. The analysis of variance and Kruskal-Wallis test were used for continuous variables. We constructed logistic regression models to calculate odds ratios for the proportion of eyes that underwent PPV versus (1) SB, or (2) PPV/SB. For each outcome, the independent variables were time period of primary retinal reattachment surgery, attending surgeons’ fellowship graduation year and SSAS. A linear mixed effects model was constructed to compare how BCVA changes over time, how it differs by type of surgery, and whether SSAS was achieved at one year. The independent variables in the model are lens status at each visit, and the three-way interaction terms are among visit, type of surgery, and primary reattachment at one year. The models included a random intercept for patients to account for correlation between bilateral eyes and a random intercept for eyes to account for correlation among BCVA from the same eyes.
Results
Three time periods over the 10-year study interval were selected to yield a comparable number of patients per group. Of the 772 patients and 808 eyes, 234 patients (240 eyes) underwent primary retinal reattachment surgery between 2008 and 2011 (time period 1 or T1), 255 patients (271 eyes) between 2012 and 2014 (T2), and 283 patients (297 eyes) between 2015 and 2017 (T3). Baseline demographics and ocular characteristics are summarized in Table 1 and were stable over time except for a higher proportion of female patients in T2.
Notably, the proportion of eyes that underwent PPV, SB, or PR significantly changed over time (p < 0.0001). In T1, most eyes underwent SB (46.7%). This proportion decreased to 34.3% in T2, and 23.2% in T3. A small percentage of eyes underwent PPV in T1 (17.1%), and this proportion increased to 36.9% in T2, and 50.2% in T3. In T3, PPV was the most utilized surgical approach for the primary repair of RRDs. The proportion of eyes that underwent PPV/SB remained relatively stable over time (T1: 26.7%, T2: 21.0%, and T3: 24.9%). PR was not commonly utilized in T1 (9.6%) and became more infrequently employed over time (T2: 7.8% and T3: 1.7%). The percentage of eyes that were treated using PPV, SB, PPV/SB, and PR over the 10-year study period is summarized in Fig. 1 and the baseline characteristics of eyes that were treated with each of these procedures are shown in Supplemental Table 1. As expected, eyes that underwent SB tended to be younger, were less likely to have a history of prior intraocular surgery, and were more likely to have lattice degeneration compared to eyes that underwent the other three procedures, while eyes that underwent PPV/SB were more likely to present with worse VA, macula-involving retinal detachment, larger retinal detachment size, more retinal breaks, and inferior retinal breaks compared to the other three procedures. No aphakic eye was treated with SB or PR, and no eye with retinal dialysis, unlocatable retinal break, or inferior retinal break underwent PR. Interestingly, all of the patients that underwent PR were white.
Change in practice pattern for primary RRD repair procedure based on ocular characteristics
When compared to T1, eyes in T2 and T3 were more likely to undergo PPV rather than SB for most of the subgroups studied based on ocular characteristics (Supplemental Table 2). Exceptions included those younger than 50, and eyes with more than 2 quadrants of detachment and inferior retinal tears in T2. Notably, the odds ratio of undergoing PPV vs SB in T3 when compared to T1 increased to 12.7 for pseudophakic/aphakic eyes, 9.48 for eyes with macular involving detachments, and 31.5 for eyes with more than 2 quadrants of detachment. The percentage of eyes that underwent PPV as compared to PPV/SB also increased in T2 and T3 when compared to T1 for most subgroups of eyes examined. Exceptions included those younger than 50 and eyes with more than 2 quadrants of detachment in T2 and T3.
Anatomic outcomes
Table 2 shows that SSAS at the one-year follow-up was highest in the PPV/SB group (87.2%), followed by the SB (80.3%), PPV (72.8%), and PR (59.2%) groups (p < 0.0001). This pattern persisted across several different presenting characteristics examined (age 50 and above, phakic or pseudophakic/aphakic status, macula detached or attached status, 2 or fewer quadrants detached and presence of lattice degeneration). In patients younger than 50 years, and eyes with more than 2 quadrants of detachment, there was no difference in SSAS across the four repair procedures examined. Most eyes were attached at final follow-up (>98% in all four groups). Mean time to first redetachment ranged from 3.0 months in the PPV/SB group to 3.7 months in the SB group.
Logistic regression was performed (Table 3) and showed that when compared to PPV, SB (p = 0.04) and PPV/SB (p = 0.0002) both had a higher overall SSAS at 1 year. When compared to SB, PPV/SB had a higher overall one-year SSAS (OR: 1.67; 95% CI: 1.000–2.792; p = 0.05) and this trend almost reached statistical significance. When stratified by presenting characteristics, SB had a superior SSAS at 1 year compared to PPV in patients who were 50 and older, as well as in eyes with retinal breaks within the inferior 4 clock hours. Patients younger than 50 were more likely to have inferior retinal breaks (74/158 eyes, 46.8%) than older patients (203/627 eyes, 32.4%) (p = 0.0008) so SB superiority in older patients was not due to a higher incidence of inferior retinal breaks. Quadrants of detachment were not included in the logistic regression due to a large number of eyes with missing information (n = 209).
Visual outcomes
Figure 2 illustrates that while mean BCVA at every postoperative visit [postoperative month (POM) 1–2, 3–7 and 8–15] is improved compared to baseline for eyes that achieved SSAS at one year (except at POM1–2 for the SB group), mean BCVA remained unchanged between baseline and all the follow-up visits for eyes that did not achieve SSAS at one year.
Influence of surgeons’ fellowship graduation year on practice trends
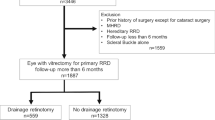
Surgeons’ fellowship graduation year was divided into three groups for analysis (1984–2000, 2001–2009, and 2010–2017). Six, eight, and eleven surgeons graduated in 1984–2000, 2001–2009, and 2010–2017, respectively, and completed 298, 251, and 259 surgeries, respectively (Supplemental Fig. 1). Most surgeons completed vitreoretinal training at Wilmer (n = 11), followed by Casey Eye Institute (n = 3), Duke Eye Center (n = 2), Wills Eye Hospital (n = 2) and Massachusetts Eye and Ear Infirmary (n = 2). One surgeon graduated from each of the following programs: Emory University, University of Texas Southwestern, Moorfields Eye Hospital, University of Tübingen, and Universidad del Rosario. Surgeons who graduated in the most recent years (2010–2017) were more likely to choose PPV over SB compared to their colleagues who graduated earlier [1984–2000: OR: 1.79; 95% CI: 1.19–2.68; p = 0.005]; [2001–2009: OR: 1.73; 95% CI: 1.14–2.65; p = 0.01]. There was no difference in odds of choosing PPV vs. PPV/SB for surgeons who graduated from 2010–2017 compared to those who completed training in 1984–2000 (p = 0.7) or 2001–2009 (p = 0.8).
Interestingly, preference for PPV increased for surgeons not only collectively but also at the individual level, and includes those who graduated earlier in 1984–2000 and 2001–2009. The practice patterns of six surgeons who had performed procedures across all three time periods were shown in Supplemental Fig. 2. The percentage of PPV performed increased for five surgeons across the three time periods while the percentage of SB performed decreased over the three time periods for three surgeons, and increased from T1 to T2 but decreased in T3 for two surgeons. Trends for percentage of PPV/SB use were less consistent across the time periods for the six surgeons examined.
Discussion
The optimal procedure to repair a primary RRD remains unresolved, and can be highly dependent on the surgeon’s training and experience since some studies have shown similar overall efficacy for SB, PPV and PPV/SB [11,12,13], while others have not [14,15,16]. In this study, we identified an evolution in practice pattern over a 10-year period at the Wilmer Eye Institute from a predominance of SB in 2008–2011 to PPV in 2015–2017. Meanwhile, the proportion of eyes that underwent PPV/SB remained stable over time. PR was uncommonly utilized in all three time periods; we will therefore focus the discussion on PPV, SB, and PPV/SB. Importantly, we found that the evolution of practice patterns from a preference for SB to PPV was driven by surgeon factor, and not patient or ocular factor. Younger surgeons who graduated more recently (2010–2017) were more likely to elect PPV over SB when compared to their older counterparts who graduated earlier (1984–2000 and 2001–2009). In addition, this change in practice pattern occurred despite similar baseline patient and ocular characteristics over the years. Also, of note, this evolution occurred despite a higher one-year SSAS with SB and PPV/SB as compared to PPV.
The increase in PPV over SB was most notable in the pseudophakic/aphakic subgroup (OR 12.7), eyes with macula off detachments (OR 9.48), and detachments of more than 2 quadrants (OR 31.5). This trend may have been driven by results from the Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment (SPR) Study Group, a prospective, randomized multicentre clinical trial that reported superior anatomic outcomes for PPV over SB in pseudophakic/aphakic eyes [12]. In macula involving and extensive detachments, PPV has not been shown to be superior to SB [17]. However, the preference for PPV may be driven by other factors. When the macula is detached, external drainage during SB carries a risk of subfoveal hemorrhage [18]. In our study, development of subretinal hemorrhage during SB occurred in 7 eyes (4 occurred during external drainage and 3 during scleral suture pass). Fortunately, all cases of subretinal hemorrhage were small and none involved the macula (including the 3 of 7 eyes that were undergoing surgery for macula involving retinal detachments).
Some surgeons consider it technically easier to completely remove subretinal fluid by internal drainage during PPV than with external drainage during SB [19]. Since RRD greater than 2 quadrants has previously been identified as a risk factor for PVR [20], some authors advocate for immediate and complete reattachment since resuming contact between photoreceptors and the RPE is hypothesized to abort the stimulus for RPE cell proliferation and migration that leads to PVR [21]. In our cohort, eight eyes were initially planned to receive primary SB, but were converted to a combined PPV/SB procedure due to excessive subretinal fluid remaining over the retinal break (n = 4), inadequate visualization of retinal break (n = 2), retinal break being too posterior (n = 1) and retinal incarceration (n = 1).
PR was used sparingly at our institution during all time periods. The choice of PR has previously been shown to be region specific. A 1997 survey demonstrated that PR is more popular on the West Coast [22] while a more recent study concluded that PR was most frequently utilized in the Northeast [6]. PR offers the convenience of being an outpatient procedure [22], and costs less ($800 for a single PR procedure) than SB ($1100) and PPV ($1400) [7]. However, PR has also been reported to have a lower success rate compared to SB and PPV [23]. Most recently, Chronopoulos and colleagues reported that PR led to higher rates of reoperation and PVR when compared to SB or PPV alone for uncomplicated RRDs [24]. Surprisingly, in our study, only white patients were treated with PR. The reasons for why patients from minority groups were not treated with PR at Wilmer are unclear; while this may be one of the limitations of a study that included a small number of eyes that received the procedure, this trend ought to be further explored in a future study.
Despite the trend toward PPV, we found that the overall SSAS at the one-year follow-up was higher in the SB and PPV/SB groups than the PPV group. Higher SSAS with SB over PPV is especially seen in older patients (81.7% vs 72.9%) and in eyes with inferior retinal breaks (81.8% vs 66.7%). Since PVR tends to initially develop inferiorly, SB may improve the SSAS because it can counteract the tractional forces of PVR that can mechanically detach the retina or reopen retinal breaks in eyes with inferior pathology, or in case gas or oil inadequately tamponades the inferior break during postoperative patient positioning, as is necessary with PPV [25]. Our study is also in agreement with others that demonstrated that PPV/SB improved reattachment rates compared to PPV, especially in eyes with inferior retinal breaks [25] although some other reports have shown that PPV and PPV/SB yield comparable anatomic outcomes [26, 27].
We emphasized SSAS as the primary study outcome because functional visual outcomes diverged in eyes that did and did not achieve SSAS at one year. In the PPV, and PPV/SB groups, eyes that achieved SSAS at one year had improvement in mean BCVA when compared to baseline at every follow-up including the one-year visit. In the SB group, eyes that achieved SSAS at one year did not differ in mean BCVA between POM1–2 and baseline, but had improvement in mean BCVA at the POM3–7 and POM8–15 visit when compared to baseline. In contrast, eyes that did not achieve SSAS at one year in the PPV, SB, and PPV/SB groups had unchanged BCVA at each of the postoperative visits when compared to baseline. This result is in agreement with the recent publication by Echegaray et al. [16].
Our overall SSAS for the PPV group (72.8%) is higher than the Pseudophakic and Aphakic Retinal Detachment (PARD) (62.6%) and SPR (67.0%) [12] study groups, but lower than previously reported in other studies (76.8 to 90%) [13,14,15,16]. We note that our follow-up period of 1 year minimum is substantially longer than most of these other studies, which mostly ranged from 2–6 months [14,15,16]. The longer follow-up period provides a higher degree of confidence for long-term reattachment and reflects the true SSAS. Importantly, we found that the mean (SD) time to redetachment is 3.4 (7.4), 3.7 (7.9), 3.0 (5.2), and 3.4 (7.5) months in the PPV, SB, PPV/SB and PR groups, respectively. Therefore, we suggest that a short follow-up period may not adequately capture the true prevalence of redetachment.
Since ocular characteristics of RRDs did not change over time, we hypothesized that the shift toward PPV was due to surgeon preference. To address this hypothesis, we analyzed the effect of fellowship graduation year on procedure choice. We found that surgeons who graduated most recently from 2010 to 2017 were more likely to choose PPV over SB when compared to their counterparts who graduated in 1984–2000 or 2001–2009. These results suggest that younger surgeons choose PPV over SB, and we postulate that this preference is due to a decreased emphasis of SB training that reduces the number of SB performed during vitreoretinal fellowships. Two surveys of graduating vitreoretinal fellows published over the past decade illustrate this trend [28, 29]. Bakri et al. collected responses from 54 fellows in 2010 and found that the largest proportion of fellows surveyed had performed fewer than 20 primary SB (n = 21, 38.9%) [28]. More recently, Venincasa and co-authors collected responses from 34 fellows in 2018 and found that an even greater percentage of those surveyed had performed fewer than 20 primary SB (n = 17, 50%) [29]. Given the low response rate to these surveys, further investigation into this trend is warranted.
In our study, younger surgeons were, however, not more likely to choose PPV over PPV/SB when compared to their more senior colleagues. Unlike primary SB, PPV/SB success does not depend on precise SB placement to support causative retinal breaks, and is thus not as technically challenging. Moreover, the success of primary SB depends on the skillful use of indirect ophthalmoscopy to locate and treat all retinal breaks, which can be difficult in cases with poor pupillary dilation and media opacities. In contrast, PPV and PPV/SB utilize wide-angle microscope illumination which allows superior visualization of the entire retina. We suggest that these factors explain why preference for PPV/SB has remained unchanged through the generations of surgeons studied. Interestingly, chandelier-assisted SB with the wide-field microscope viewing system has become increasingly popular in recent years since it circumvents the challenges of indirect ophthalmoscopy [30]. It remains to be seen if this technique will increase the utilization of primary SB in the future.
The strengths of this study include the large number of eyes that each underwent SB, PPV, and PPV/SB and the follow-up period (minimum of one year) which was longer than comparable studies. Limitations include the retrospective nature of the study with variability in chart documentation resulting in missing information for some of the variables collected, lack of standardization of surgical techniques given inclusion of cases from many surgeons with diverse training and the involvement of vitreoretinal fellows in surgical cases, as well as lack of standardization in refraction limiting the BCVA that were collected.
In summary, the trend to treat primary RRDs with PPV increased over the past 10 years at the Wilmer Eye Institute, independent of the case complexity. Surgeons who graduated most recently are most likely to choose PPV over SB but not PPV/SB when compared to their more senior counterparts. Therefore, the evolution of practice patterns towards PPV may be driven not just by improvements in small gauge vitrectomy, but also by a shift in vitreoretinal training away from primary SB. Due to the long postoperative follow-up period and superior anatomic outcomes with SB and PPV/SB over PPV, these results should make us carefully consider the procedure that will provide sustained attachment with a single procedure. We also advocate that SB training remains an important element that should be emphasized during vitreoretinal fellowship.
Summary
What was known before
-
Pars plana vitrectomy has grown in popularity for the repair of uncomplicated rhegmatogenous retinal detachments over time, when compared to scleral buckling or vitrectomy/scleral buckling.
What this study adds
-
This study confirms that the trend favouring pars plana vitrectomy over scleral buckling and vitrectomy/scleral buckling was also seen in a real-world setting at a tertiary academic center. The study additionally found that this trend was driven by the preference of younger surgeons and was not influenced by ocular or patient characteristics. Morever, this study shows that the single surgery anatomic success rates are higher for scleral buckling and vitrectomy/scleral buckling when compared to pars plana vitrectomy. Therefore, scleral buckling and vitrectomy/scleral buckling should be more often considered in the repair of rhegmatogenous retinal detachments.
Data availability
The data that support the findings of this study are available from the corresponding author, JTH, upon reasonable request.
References
Gonin J. Abbildungen von operativ verschlossenen Netzhautrissen bei Ablösung. Ber Dtsch Ophth Ges. 1929;47:445–7.
Schepens CL. Progress in detachment surgery. Trans Am Acad Ophthalmol Otolaryngol. 1951;55:607–15.
Machemer R, Buettner H, Norton EW, Parel JM. Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol. 1971;75:813–20.
Hilton GF, Grizzard WS. Pneumatic retinopexy. A two-step outpatient operation without conjunctival incision. Ophthalmology. 1986;93:626–41.
Eckardt C. Transconjunctival sutureless 23-gauge vitrectomy. Retina. 2005;25:208–11.
Hwang JC. Regional practice patterns for retinal detachment repair in the United States. Am J Ophthalmol. 2012;153:1125–8.
Vail D, Pershing S, Reeves M, Afshar AR. The relative impact of patient, physician, and geographic factors on variation in primary rhegmatogenous retinal detachment management. Ophthalmology. 2020;127:97–106.
Wong CW, Wong WL, Yeo IY, Loh BK, Wong EY, Wong DW, et al. Trends and factors related to outcomes for primary rhegmatogenous retinal detachment surgery in a large Asian tertiary eye center. Retina. 2014;34:684–92.
de la Rua ER, Pastor JC, Fernandez I, Sanabria MR, Garcia-Arumi J, Martinez-Castillo V, et al. Non-complicated retinal detachment management: variations in 4 years. Retina 1 project; report 1. Br J Ophthalmol. 2008;92:523–5.
Eibenberger K, Georgopoulos M, Rezar-Dreindl S, Schmidt-Erfurth U, Sacu S. Development of surgical management in primary rhegmatogenous retinal detachment treatment from 2009 to 2015. Curr Eye Res. 2018;43:517–25.
Znaor L, Medic A, Binder S, Vucinovic A, Marin Lovric J, Puljak L. Pars plana vitrectomy versus scleral buckling for repairing simple rhegmatogenous retinal detachments. Cochrane Database Syst Rev. 2019;3:CD009562.
Heimann H, Bartz-Schmidt KU, Bornfeld N, Weiss C, Hilgers RD, Foerster MH, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical study. Ophthalmology. 2007;114:2142–54.
Schaal S, Sherman MP, Barr CC, Kaplan HJ. Primary retinal detachment repair: comparison of 1-year outcomes of four surgical techniques. Retina. 2011;31:1500–4.
Ryan EH, Ryan CM, Forbes NJ, Yonekawa Y, Wagley S, Mittra RA, et al. Primary retinal detachment outcomes study report number 2: Phakic retinal detachment outcomes. Ophthalmology. 2020;127:1077–85.
Joseph DP, Ryan EH, Ryan CM, Forbes NJK, Wagley S, Yonekawa Y, et al. Primary retinal detachment outcomes study: pseudophakic retinal detachment outcomes: primary retinal detachment outcomes study report number 3. Ophthalmology. 2020;127:1507–14.
Echegaray JJ, Vanner EA, Zhang L, Fortun JA, Albini TA, Berrocal AM, et al. Outcomes of pars plana vitrectomy alone versus combined scleral buckling plus pars plana vitrectomy for primary retinal detachment. Ophthalmol Retina. 2021;5:169–75.
Wong CW, Yeo IY, Loh BK, Wong EY, Wong DW, Ong SG, et al. Scleral buckling versus vitrectomy in the management of macula-off primary rhegmatogenous retinal detachment: a comparison of visual outcomes. Retina. 2015;35:2552–7.
Chen SN, Ho CL, Kuo YH, Ho JD. Intravitreous tissue plasminogen activator injection and pneumatic displacement in the management of submacular hemorrhage complicating scleral buckling procedures. Retina. 2001;21:460–3.
Chen X, Zhang Y, Yan Y, Hong L, Zhu L, Deng J, et al. Complete subretinal fluid drainage is not necessary during vitrectomy surgery for macula-off rhegmatogenous retinal detachment with peripheral breaks: a prospective, nonrandomized comparative interventional study. Retina. 2017;37:487–93.
Girard P, Mimoun G, Karpouzas I, Montefiore G. Clinical risk factors for proliferative vitreoretinopathy after retinal detachment surgery. Retina. 1994;14:417–24.
Campochiaro PA. Pathogenic mechanisms in proliferative vitreoretinopathy. Arch Ophthalmol. 1997;115:237–41.
Benson WE, Chan P, Sharma S, Snyder WB, Bloome MA, Birch DG. Current popularity of pneumatic retinopexy. Retina. 1999;19:238–41.
Zaidi AA, Alvarado R, Irvine A. Pneumatic retinopexy: success rate and complications. Br J Ophthalmol. 2006;90:427–8.
Chronopoulos A, Hattenbach LO, Schutz JS. Pneumatic retinopexy – a critical re-appraisal. Surv Ophthal. 2020;S0039-6257:30179–X.
Starr MR, Obeid A, Ryan EH, Ryan C, Ammar M, Patel LG, et al. RETINAL DETACHMENT WITH INFERIOR RETINAL BREAKS: primary vitrectomy versus vitrectomy with scleral buckle (PRO Study Report No. 9). Retina. 2021;41:525–30.
Martinez-Castillo VJ, Garcia-Arumi J, Boixadera A. Pars plana vitrectomy alone for the management of pseudophakic rhegmatogenous retinal detachment with only inferior breaks. Ophthalmology. 2016;123:1563–9.
Duvdevan N, Mimouni M, Feigin E, Barak Y. 25-gauge pars plana vitrectomy and SF6 GAS for the repair of primary inferior rhegmatogenous retinal detachment. Retina. 2016;36:1064–9.
Bakri SJ, Alniemi ST, Chan RV. Experiences of vitreoretinal surgery fellows in the United States. Retina. 2013;33:392–6.
Venincasa MJ, Hubschman S, Kuriyan AE, Berrocal A, Sivalingam A, Albini TA, et al. Perceptions of vitreoretinal surgical fellowship training in the United States. Ophthalmol Retina. 2019;3:802–4.
Roca JA, Maia M, da Cruz NFS, Polizelli MU, Chhablani J, Gangakhedkar S, et al. Non-contact wide-angled visualization with chandelier-assisted scleral buckling for primary uncomplicated rhegmatogenous retinal detachment. Graefes Arch Clin Exp Ophthalmol 2020;258:1857–61.
Funding
This project was supported by an unrestricted grant from Research to Prevent Blindness (Wilmer Eye Institute) and the Wilmer Biostatistics Core Grant P30EY01765. JTH is the Robert Bond Welch Professor. The funding organizations had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
SSO, IA, and JTH designed the concept of this work and interpreted the data. SSO, IA, AG, UTA, BB, XD, ATP, YSS, and AZ completed data collection. SSO, LTA, and JW performed statistical analysis. SSO and IA drafted the manuscript. All authors critically reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ong, S.S., Ahmed, I., Gonzales, A. et al. Management of uncomplicated rhegmatogenous retinal detachments: a comparison of practice patterns and clinical outcomes in a real-world setting. Eye 37, 684–691 (2023). https://doi.org/10.1038/s41433-022-02028-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02028-z
This article is cited by
-
Pre-operative intravitreal bevacizumab for tractional retinal detachment secondary to proliferative diabetic retinopathy: the Alvaro Rodriguez lecture 2023
International Journal of Retina and Vitreous (2023)