Abstract
Purpose
Increasing evidence suggests myopia is not a simple refractive error, many other factors might also be involved. Here, we assessed myopic and normal corneas’ gene expression profiles to identify possible diagnostic and therapeutic biomarkers for myopia.
Materials and methods
We obtained the expression profile of ten patients and seven normal control samples from the GSE112155 and GSE151631 datasets based on the Gene Expression Omnibus (GEO) database. We used the “limma” R package to determine the differentially expressed genes (DEGs) between myopic and normal corneas. Weighted gene co-expression network analysis (WGCNA) was used to identify critical co-expressed modules related to myopia, and enrichment analyses were used to annotate the function of genes encompassed in the compulsory module. We also validated these findings in two external datasets (GSE24641 and GSE136701).
Results
We identified that the DEGs were significantly enriched in ultraviolet (UV) response, TNF-α signaling via NFκB, Angiogenesis, Myogenesis pathways, etc. We used 2095 genes to construct the co-expression gene modules and found five interesting modules because the eigengene expression of these modules was significantly differentially expressed between myopic and normal corneas. Notably, the enrichment analysis found that the genes encompassed in lightgreen module were significantly enriched in immune-related pathways. These findings were proved by subsequent analysis based on Xcell software. We found the component of B cells, CD4+ memory T cells, CD8+ central memory T cells, plasmacytoid dendritic cells, T helper 2 (Th2) cells, regulatory T cells (Tregs), etc. were significantly increased in myopic corneas, while CD8+ T cells, CD4+ T central memory cells, natural killer T (NKT) cells, and T helper 1 (Th1) cells were significantly decreased.
Conclusion
Our findings identified some markers that might detect diagnosis and treatment for myopia from cornea aspect. Future studies are warranted to verify the functional role of immune-related pathways in cornea during the pathogenesis or progression of myopia.
Similar content being viewed by others
Introduction
Myopia is a common eye disease which influenced 22.9% of human beings [1]. Myopia occurs when the axial length is too long, relative to the focusing power of the cornea and lens of the eye. This causes light rays to focus at a point in front of the macular fovea, rather than directly on its surface. Myopia can also be caused by the cornea and/or lens being too curved for the axial length of the eyeball. Carney et al. found myopic eyes had steeper corneas, and there were significant correlations between corneal radius of curvature and myopia [2]. Cross-sectional [2] and longitudinal [3] studies showed patients with higher asphericity of cornea (less negative or even positive) always had increasing myopia.
However, the causes of myopia are very complicated, and the underlying biological mechanism has not been clearly studied so far. Both gene-gene interactions and gene-environment interactions have been reported to be the pathogenesis of myopia. Many candidate genes were identified related to myopia through chromosome linkage analysis in myopic families. For example, Zhang et al. [4] conducted linkage analysis on 12 family members of a large Chinese family with the autosomal dominant inheritance of high myopia and determined that the MYP11 locus on chromosome 4q22-q27 was related to myopia. MYP13 on chromosome Xq23-q25 was also identified through linkage analysis of a 4-generation Chinese Han family [5]. In recent years, discovering genes and genomic regions related to ophthalmic diseases, including myopia, has been extensively promoted by the progress in high-throughput sequencing, gene association research, and bioinformatics. Through genome sequencing technology, researchers have discovered a variety of non-syndromic myopia pathogenic genes, including ZNF644 [6], SCO2 [7], SLC39A5 [8], CCDC111 [9], P4HA2 [10], and LRPAP1 [10], etc. In addition, based on the method of genome-wide association analysis, some potentially relevant SNP loci have also been reported. Transcriptome sequencing technology was also used in myopia research. For example, Riddell et al. performed RNA-seq to examine gene expression in the retina/RPE/choroid across 3 days of optically-induced myopia and hyperopia induction in chick. Interestingly, they detected the expression of various immune pathways were correlated with axial length and and refraction [11]. Enzymelinked immunosorbent assay studies also showed that the decreased immune response to collagen and low-grade intraocular inflammation were characteristic of the progression of myopia, respectively. These studies highlighted the important role of immunological changes in myopia [12, 13]. However, except for in vivo experiments in animal models, few studies reported the gene expression changes between human myopic and normal samples. Studies using human samples would enable us to get more direct data to reveal the biological mechanism behind myopia.
In order to further study the genetic changes in cornea of myopic samples, we explored the expression variation between myopic and normal corneas, and found that the immune-related pathways might be activated in the myopic corneas group, and these processes might be resulted in the pathogenesis or progression of myopia.
Materials and methods
Data source
The RNA-seq data of corneal epitheliums from myopia patients (GSE112155, ten samples) and control individuals with healthy corneal epithelium (GSE151631, seven samples) were downloaded from Gene Expression Omnibus (GEO) database, respectively. Both datasets were sequenced on Illumina sequencing platforms. The reads count matrices of the case and control were normalized using the “limma” package [14], respectively. In order to adjust the batch effect, the normalized read count matrices were merged and processed by ComBat [15]. An expression profile containing three highly myopic human eye lenses and three emmetropia lenses (GSE136701) were also downloaded from GEO, which was generated by microarray. Besides, another microarray-based chicken retina/retinal pigment epithelium (RPE) expression matrices (GSE24641) was downloaded from the GEO database, including both normal eyes as well as eyes with myopia/farsightedness that obtained after artificial induction through wearing a unilateral spectacle lens with different degrees for different long times. Samples with hyperopia were removed in this study.
Co-expression analysis
To reduce the computing resources, only highly variable genes (HVGs) were considered to perform the co-expression analysis, while the HVGs were caused by biological effects instead of merely technical noise. We assumed that the observed mean expression (\(\widehat {\mu _i}\)) and the observed squared coefficient of variation (CV2) (\(\widehat {w_i}\)) of gene i among cells have the following relationship:
We fitted the expected CV2 and the 95% confidence intervals (CI) following the relationship and treated the genes that express more than the upper 95% CI as HVGs. We applied WGCNA [16] to construct the co-expressed genes into modules to identify genes related to myopia. We assumed that gene networks should obey a scale-free distribution during the WGCNA analysis. The co-expression relationship was determined by pairwise Pearson’s correlation coefficients among all the genes and subsequently transformed into a scale-free network by converting the matrix to an adjacent matrix. We set the soft threshold value as seven in this study. Genes with high correlations were assigned into the same module based on the adjacent matrix, and we set the minimum number of genes in each module at 30. The eigengene has represented a specific expression profile of each module [17]. In order to identify critical modules related to myopia, we compared the eigengene expression level of each module between myopia samples and control, and differentially expressed modules were selected based on the p value (p < 0.05) calculated by the Wilcox test. In this way, we detected five modules (lightgreen, magenta, purple, red, and salmon) associated with myopia. For different modules, we selected different weight thresholds to define authentic co-expression relationships among genes (modules of red, lightgreen, magenta, and salmon were set as 0.5, and purple were set as 0.4) in consideration of the gene size. The top ten genes with most links (authentic co-expression relationship) with other genes were considered as hub-genes in each module, and hub-genes differentially expressed between myopia samples and control were extracted as essential genes of myopia.
Enrichment analysis
We used the R package clusterProfiler to identify the functional pathways of critical modules [18]. Gene set enrichment analysis (GSEA) was performed via GSEApy (https://github.com/zqfang/GSEApy). We downloaded the terms of Gene Ontology, Kyoto Encyclopedia of Genes and Genomes, Reactome, and MSigDB Hallmark pathways, and conducted the GSEA analysis, respectively. The significant gene terms were considered as significantly enriched as false discovery rate <0.05.
Infiltrating immune cells analysis and statistical analysis
Normalized gene expression data were used to infer the abundance scores of different types of infiltrating immune cells using the xCell algorithm [19]. A two-sided Wilcox test was applied to compare the statistical difference between groups. Statistical analysis was executed using R software, version 3.6.0.
Results
Differential analysis between myopic and normal corneas
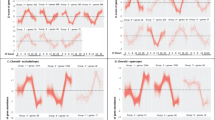
Expression profiles of myopic and normal corneas were downloaded from GEO (GSE112155 and GSE151631). The “limma” package was used to standardize the expression profile, and then batch effects were removed by using the “Combat” package. To explore the functional changes in myopia samples, we performed GSEA analyses to compare the difference between myopic and normal corneas at pathway levels. As a result, we found that the differences between these two groups were concentrated on Gene silencing by RNA, DNA packaging related pathway, Extracellular matrix related pathway TNF-α Signaling via NFκB, UV Response, Angiogenesis, Myogenesis, Proximal Tubule Bicarbonate Reclamation, ECM Receptor Interaction, Leishmania Infection, Complement, and Coagulation Cascades, Systemic Lupus Erythematosus (SLE) (Fig. 1A and Table S1), etc. Interestingly, several immune-related pathway/terms were significantly enriched, including Inflammatory response (Fig. 1B), IL6 Jack Stat5 signaling (Fig. 1C), IL2 Stat5 signaling (Fig. 1D), Intestinal immune network for IgA production, Leukocyte transendothelial migration, Cytokine cytokine receptor interaction, etc. (Table S1), suggesting the disruption of the immune microenvironment in myopia.
We next downloaded other two expression profiles (GSE136701 and GSE24641) from GEO database, one is a microarray-based expression profile containing three highly myopic human eye lenses and three emmetropia lenses, and the other is chicken RPE transcriptome obtained from both normal eyes as well as myopic eyes (hypermetropic samples were removed in this study) after artificial induction through wearing a unilateral spectacle lens with degrees. Myopia vs. normal GSEA analysis was also performed on these two datasets, and we also found immune pathways enriched in myopic tissues. For example, Humoral immune response, B cell homeostasis/activation, Regulation of t cell-mediated immunity, T cell activation involved in immune response, Lymphocyte activation involved in immune response were significantly enriched in highly myopic human eyes in GSE136701 (Fig. S1A and Table S2), and gene terms of Humoral immune response mediated by circulating immunoglobulin, Complement activation, B cell-mediated immunity, T cell receptor complex, Interferon alpha/gamma response, IL6 Jak Stat3 signaling, Inflammatory response and Immunoregulatory interactions between a lymphoid and a non-lymphoid cell were detected significantly activated in myopic tissues from GSE24641 (Fig. S1B and Table S3). These results show consistency with the above findings.
Co-expression network analysis reveals an immune-related module differentially expressed between myopia and normal tissue
To investigate the myopia-related critical genes in our expression data, we performed the co-expression analysis. We first determined the HVGs among samples for the downstream analysis. The squared CV of genes and their average expression were fitted, and genes with CV2 greater than the 95% CI of expected CV2 were defined as HVGs (see “Material and methods”) (Fig. 2A). Ultimately 2095 genes and 17 samples were extracted for doanstream analysis. WGCNA algorithm was applied to the expression network analysis, and in this process, the appropriate soft threshold power for matrix transformation was selected as 7 (Fig. 2B), and the minimum gene size in co-expression modules was set as 30. As a result, we constructed the co-expression modules and identified 18 myopia-related modules (Fig. 2C), which were black (95 genes), blue (222 genes), brown (203 genes), cyan (66 genes), green (150 genes), yellow (156 genes), turquoise (346 genes), salmon (81 genes), purple (84 genes), pink (90 genes), magenta (84 genes), lightgreen (35 genes), lightcyan (51 genes), grey60 (48 genes), greenyellow (83 genes), midnight-blue (62 genes), red (137 genes), and tan (82 genes).
A Identification of highly variable genes (HVGs). The relationship between CV2 and the mean expression of genes was shown in the plot. The black line shows the trend for the fit curve between CV2 and mean expression and was used to identify HVGs (colored in red). For each gene, the residual variability is calculated as the difference between observed CV2 and expected CV2 from the fitted curve. B Soft-thresholding power analysis was used to obtain the scale-free fit index of network topology. C Heatmap depicts the Topological Overlap Matrix (TOM) of genes selected for weighted co-expression network analysis. Light color represents lower overlap, and red represents higher overlap.
We compared the eigengene expression of each module between myopic and normal corneas, and found that the eigengene of magenta, red and purple were significantly lower expressed in myopic than normal corneas, while the eigengene of salmon and lightgreen was significantly higher expressed (Fig. S2A). The gene co-expression networks of each module were visualized by the Cytoscape software (Fig. 3A and Fig. S2B–E). To further explain the biological significance of these five critical modules, we performed over-represent enrichment analyses. We found that the genes encompassed in the purple module were primarily enriched in the mitotic nuclear division, nuclear division, Regulation of nuclear division, G2M checkpoint, E2F targets, Oocyte meiosis, Progesterone-mediated oocyte maturation, etc. (Fig. S3A). The genes encompassed in the red module were mainly enriched in epithelial-mesenchymal transition, extracellular structure organization, extracellular matrix organization, Collagen formation, Elastic fiber formation, etc. (Fig. S3B). Particularly, the genes involved in the lightgreen module were primarily enriched in immune-related terms, including T cell activation, T cell differentiation, cytokine receptor activity, CXCR chemokine receptor binding Allograft rejection, Inflammatory response, IL6/Jak/Stat3 signaling, etc. Besides, this module also enriched in KRAS signaling, which was also significantly enriched in GSEA results of all datasets above (Fig. 3B). However, we failed to identify any significantly enriched pathways for the magenta and salmon modules.
Differences in infiltrated immune cells between myopic and normal corneas
Considering the significant enrichment of the immune-related pathway in the GSEA analysis and lightgreen module, we performed the immune cell deconstruction analysis to compare the immune cell component differences between myopia and normal tissues. xCell software was applied in this analysis, which is a webtool that performs cell type enrichment analysis from gene expression data for different immune and stromal cell types. Consistent with the functional enrichment results of lightgreen module, we identified a significant difference in T cell abundances between these two groups, including CD4+ memory T cell, CD8+ central memory T cell, CD4+ Th2, Tregs, which were significantly higher enriched in myopic corneas, and CD8+ T cell, CD4+ T central memory cell, NK T cell, and CD4+ Th1 were significantly lower enriched in myopic corneas. We also found that the B cell, Common myeloid progenitor, B cell naive, Plasmacytoid dendritic cell, Cancer-associated fibroblast, and memory B cell were significantly higher enriched in myopic corneas, which is also consistent with GSEA analysis results (Fig. 4 and Table S4). This indicates that immune abnormality is an essential sign of myopia and may play an important role in the process of myopia.
Discussion
In this study, we compared the expression profile between corneas tissues derived from healthy control and myopia patients. GSEA of different datasets suggested that immune-related pathways were significantly enriched in the comparison of myopic and normal corneas. We used WGCNA to construct predictive function-related gene clusters, identify modules, and select genes that can serve as potential biomarkers for the diagnosis, prevention, and/or treatment of myopia, considering the claim that it is a method more reliable and biological than others [20]. As a results, a total of 18 co-expression modules were identified based on 2095 genes from 17 human samples. Besides, we found five modules of interest since the Eigengene expression of these modules were significantly varied between the two groups.
Genes encompassed in the lightgreen module were mainly gathered in T cell differentiation, cytokine receptor activity, calcium ion transmembrane transport, T cell activation, CXCR chemokine receptor binding, Inflammatory response, Allograft rejection, KRAS signaling, and IL6/Jak/Stat3 signaling and so on, indicating that the immune process takes part in the pathogenesis of myopia. Therefore, the discrepancy of infiltrated immune cells between myopic and normal corneas was further contrasted. We found that the components of B cell, CD4+ memory T cell, Common myeloid progenitor, B cell naive, CD8+ central memory T cell, Plasmacytoid dendritic cell, Cancer-associated fibroblast, CD4+ Th2, Tregs, and memory B cell were significantly increased in myopic corneas. In contrast, CD8+ T cell, CD4+ T central memory cell, NK T cell, and CD4+ Th1 were significantly decreased in the myopia tissue. The inflammatory reaction, which attracts blood cells, cytokines, prostaglandins, growth factors and cytotoxic factors to the infected or injured areas [21], can induce local biochemical reactions and lead to remodeling of the tissue [22]. More frequently appeared in diabetic patients than in the normal person (38% vs. 27%), type I and type II diabetes are risk factors of myopia [23], while the latter is an inflammatory illness, relating to the increase of serum levels of IL-1 β and IL-6, TNF-α and TGF-β [24]. Identically, over 30% of SLE patients have been reported to suffer from visual system disorders like myopia. SLE is also characterized by inflammatory xerophthalmia, scleritis, and scleritis [25]. Uveitis, which around 6% of all its patients are individuals under 18 years old [26], can cause myopic displacement and acute or constitutive myopia. Besides, juvenile rheumtoid arthritis (JCA)-associated uveitis performs as the most common reason for intraocular inflammation [27], while acute scleritis can cause acute myopia. About 10–20% of JCA patients have chronic uveitis [28], which usually has no apparent symptoms when infecting children with JCA and gradually develop and even lead to blindness. The inflammatory factors IL-6 and TNF-α are reported to be higher expressed in the aqueous humor of patients with uveitis [29], while the high incidence of uveitis in JCA patients and elevated levels of IL-6 and TNF-α may exacerbate myopia, which can be reversed by application of anti-inflammatory agents [30]. In addition, the incidence of myopia may get rise by chronic or acute systemic inflammation concerns these diseases. We identify that the inflammation processes were also existed in corneas tiisues derived from myopic patients. These results were interesting but lack of functional assay to investigate the real role of corneas’s inflammatory in the pathogenesis and progression of myopia. Thus, subsequent studies are warranted to verify these findings.
As descripted in the introduction, several studies have reported the morphological changes of the cornea in myopic people, suggesting that it is valuable to study changes at the transcriptome level of cornea. Objectively, there is currently few public transcriptome data with sufficient sample sizes from other parts of the eye (for example, retina or sclera, which are also physiologically changed when myopia occurs) with both myopic and normal samples for our study. An important reason is that the myopia cornea is relatively easy to obtain (e.g., femtosecond surgery), while tissue samples from other eye parts need to be donated from the body, which is more difficult to obtain. However, we validated our finding in independent datasets, including human lenses and chicken RPE, and finding immune pathways abnormal expression in all myopic tissues.
There are several advantages and limitations of the current study. Based on the DEGs, we identified some crucial pathways potentially involved in the development of myopia. We found that there exists a significant difference in infiltrated immune cells between the myopic and normal corneas. These results further confirmed the role of inflammation processes in the pathogenesis of myopia. However, the samples of cases and controls were not derived from the same patients, compromising the current study’s evidence level. Secondly, the findings were not validated by external clinical samples. Besides, there still need more evidence to prove whether the corneas inflammation involves in the pathogenesis or progression of myopia.
In conclusion, we have identified 18 modules via WGCNA, and five modules were selected to be analyzed in detail. We found that the genes encompassed in the lightgreen module were primarily enriched in immune-related pathways, which is worthy of further in-depth study to explore the mechanism of myopia.
Summary
What was known before
-
We identified that the differentially expressed genes were significantly enriched in UV response, TNF-α signaling via NF-κB, Angiogenesis, Myogenesis pathways, and so on, between myopic and normal corneas.
-
We used 2095 genes to construct the co-expression gene modules and found five interesting modules because the eigengene expression of these modules was significantly differentially expressed between myopic and normal corneas. Notably, the enrichment analysis found that the genes encompassed in lightgreen module were significantly enriched in immune-related pathways.
-
Xcell analyses suggested that the B cell, CD4+ memory T cell, CD8+ central memory T cell, Plasmacytoid dendritic cell, Th2, Tregs, etc. were significantly higher enriched in myopic corneas, while CD8+ T cell, CD4+ T central memory cell, NK T cell, and Th1 were significantly lower enriched.
What this study adds
-
Our findings identified some markers that might detect diagnosis and treatment for myopia from cornea aspect.
References
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42.
Carney LG, Mainstone JC, Henderson BA. Corneal topography and myopia. A cross-sectional study. Invest Ophthalmol Vis Sci. 1997;38:311–20.
Horner DG, Soni PS, Vyas N, Himebaugh NL. Longitudinal changes in corneal asphericity in myopia. Optom Vis Sci. 2000;77:198–203.
Zhang Q, Guo X, Xiao X, Jia X, Li S, Hejtmancik JF. A new locus for autosomal dominant high myopia maps to 4q22-q27 between D4S1578 and D4S1612. Mol Vis. 2005;11:554–60.
Zhang Q, Guo X, Xiao X, Jia X, Li S, Hejtmancik JF. Novel locus for X linked recessive high myopia maps to Xq23-q25 but outside MYP1. J Med Genet. 2006;43:e20.
Shi Y, Li Y, Zhang D, Zhang H, Li Y, Lu F, et al. Exome sequencing identifies ZNF644 mutations in high myopia. PLoS Genet. 2011;7:e1002084.
Tran-Viet KN, Powell C, Barathi VA, Klemm T, Maurer-Stroh S, Limviphuvadh V, et al. Mutations in SCO2 are associated with autosomal-dominant high-grade myopia. Am J Hum Genet. 2013;92:820–6.
Guo H, Jin X, Zhu T, Wang T, Tong P, Tian L, et al. SLC39A5 mutations interfering with the BMP/TGF-beta pathway in non-syndromic high myopia. J Med Genet. 2014;51:518–25.
Zhao F, Wu J, Xue A, Su Y, Wang X, Lu X, et al. Exome sequencing reveals CCDC111 mutation associated with high myopia. Hum Genet. 2013;132:913–21.
Guo H, Tong P, Liu Y, Xia L, Wang T, Tian Q, et al. Mutations of P4HA2 encoding prolyl 4-hydroxylase 2 are associated with nonsyndromic high myopia. Genet Med. 2015;17:300–6.
Riddell N, Giummarra L, Hall NE, Crewther SG. Bidirectional expression of metabolic, structural, and immune pathways in early myopia and hyperopia. Front Neurosci. 2016;10:390.
Lazuk AV, Slepova OS, Tarutta EP. Antibodies to collagen in patients with progressive myopia. In: Tokoro T, editor. Myopia updates: Proceedings of the 6th International Conference on Myopia. Tokyo, Japan: Springer; 1998. p. 120–3.
Yuan J, Wu S, Wang Y, Pan S, Wang P, Cheng L. Inflammatory cytokines in highly myopic eyes. Sci Rep. 2019;9:3517.
Ritchie ME, Phipson B, Wu D, Hu Y, Law CW, Shi W, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47.
Zhang Y, Parmigiani G, Johnson WE. ComBat-seq: batch effect adjustment for RNA-seq count data. NAR Genom Bioinform. 2020;2:lqaa078.
Langfelder P, Horvath S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinforma. 2008;9:559.
Zhang C, Peng L, Zhang Y, Liu Z, Li W, Chen S, et al. The identification of key genes and pathways in hepatocellular carcinoma by bioinformatics analysis of high-throughput data. Med Oncol. 2017;34:101.
Yu G, Wang LG, Han Y, He QY. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS. 2012;16:284–7.
Aran D, Hu Z, Butte AJ. xCell: digitally portraying the tissue cellular heterogeneity landscape. Genome Biol. 2017;18:220.
Chou WC, Cheng AL, Brotto M, Chuang CY. Visual gene-network analysis reveals the cancer gene co-expression in human endometrial cancer. BMC Genomics. 2014;15:300.
Kawai T, Akira S. Innate immune recognition of viral infection. Nat Immunol. 2006;7:131–7.
Kim S, Shin S, Hyun B, Kong H, Han S, Lee A, et al. Immunomodulatory effects of dioscoreae rhizome against inflammation through suppressed production of cytokines via inhibition of the NF-κB pathway. Immune Netw. 2012;12:181–8.
Fledelius HC. Is myopia getting more frequent? A cross-sectional study of 1416 Danes aged 16 years+. Acta Ophthalmol. 1983;61:545–59.
Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol. 2011;11:98–107.
Palejwala NV, Walia HS, Yeh S. Ocular manifestations of systemic lupus erythematosus: a review of the literature. Autoimmune Dis. 2012;2012:290898.
Nguyen QD, Foster CS. Saving the vision of children with juvenile rheumatoid arthritis-associated uveitis. JAMA. 1998;280:1133–4.
Päivönsalo-Hietanen T, Tuominen J, Saari KM. Uveitis in children: population-based study in Finland. Acta Ophthalmol. 2000;78:84–8.
Kesen MR, Setlur V, Goldstein DA. Juvenile idiopathic arthritis-related uveitis. Int Ophthalmol Clin. 2008;48:21–38.
Chen W, Zhao B, Jiang R, Zhang R, Wang Y, Wu H, et al. Cytokine expression profile in aqueous humor and sera of patients with acute anterior uveitis. Curr Mol Med. 2015;15:543–9.
Lin HJ, Wei CC, Chang CY, Chen TH, Hsu YA, Hsieh YC, et al. Role of chronic inflammation in myopia progression: clinical evidence and experimental validation. EBioMedicine. 2016;10:269–81.
Author information
Authors and Affiliations
Contributions
YN, LW, and CL performed bioinformatics analysis. YN and JZ designed the research study. YN prepared the paper drafting. ZL, JY and JZ performed paper editing. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ni, Y., Wang, L., Liu, C. et al. Gene expression profile analyses to identify potential biomarkers for myopia. Eye 37, 1264–1270 (2023). https://doi.org/10.1038/s41433-022-02013-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02013-6
This article is cited by
-
Comparisons of the protein expressions between high myopia and moderate myopia on the anterior corneal stroma in human
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)