Abstract
Background
Timely management of aphakic children is critical for the rehabilitation of adequate visual gain. This study aims to evaluate the long-term efficacy of scleral contact lenses in terms of visual outcomes, complications, and compliance in aphakic children.
Methods
Retrospective data review of children with congenital or acquired cataract, or subluxated crystalline lenses, who underwent lensectomy from 2004 to 2018 and who used scleral contact lenses for refractive correction. Collected data from the follow up period included recorded aphakic refraction and visual acuity, complications following scleral contact lens wear documented in the clinic and ophthalmic emergency room and compliance to lens wear according to parental feedback on every visit in the clinic.
Results
76% of cases, with final best corrected visual acuity (BCVA) of 20/40 or better achieved in seventeen eyes (34%). The rate of amblyopia was 50%. Strabismus developed in 56% of children, and those had less favourable visual outcomes (0.43 ± 0.4 LogMAR without strabismus and 0.8 ± 0.5 LogMAR with strabismus, p = 0.015). No corneal infections were documented during the follow up. Main adverse effect on the ocular surface was superficial punctate keratopathy (n = 16). Compliance was good in 48 children (96%)- except for two cases, the scleral lenses were tolerated well by all children.
Conclusion
Scleral contact lenses are an effective means of visual rehabilitation in aphakic children after lensectomy and may be used long-term with good compliance of wear, excellent visual outcomes, and tolerable adverse events.
Similar content being viewed by others
Introduction
Congenital cataract should be diagnosed at birth or early in the postnatal period, as it is highly amblyogenic and if not treated in time will lead to deprivation amblyopia and severe permanent visual loss [1]. For any significant lens opacity that leads to a considerable risk of amblyopia, cataract surgery is indicated [2].
There are two major approaches for refractive correction in these cases, being primary intraocular lens (IOL) implantation or refractive correction by means of contact lens or glasses, with an option of secondary IOL implantation in the future. Primary IOL implantation is considered by many to be the standard of care for children 2 years of age or older in the United States [3]. In addition to its convenience, it may be associated with better visual outcomes [4]. However, these potential advantages may be offset by a higher incidence of intraoperative and postoperative adverse events, such as lens re-proliferation into the visual axis, pupillary membranes, and corectopia [5, 6]. Furthermore, the rapid and unpredictable growth of infant eyes makes it difficult to select the ideal IOL power to implant [7].
It has been suggested that the practice of using contact lenses may contribute to poor long-term visual outcome [8], and recent years have shown an increase in the use of IOLs to optically correct unilateral aphakia during infancy [9].
The Infant Aphakia Treatment Study (IATS) did not find a significant difference in visual acuity for infants with a unilateral congenital cataract under 7 months of age who were corrected with a contact lens compared to an intraocular lens after cataract surgery. Of note, it has been shown that there were significantly more adverse events and additional intraoperative procedures in the IOL group [10].
Common contact lens alternatives for postoperative visual rehabilitation in aphakia are mostly silicon soft lenses or rigid gas permeable corneal contact lenses.
The soft lenses do not correct for astigmatism, are easily contaminated with dirt and debris increasing the risk of infection. The RGP lenses are easily rubbed out and in these cases are not cost effective. Scleral lenses are stable and cost effective, their disadvantage being a possible cause of mild corneal adverse effects [11].
A scleral contact lens is a lens fitted to vault over the entire cornea, and to land on conjunctiva overlying the sclera. The lens edge resting entirely on the conjunctiva over the sclera, provides lens stability and comfort. These lenses provide excellent optical correction of high refractive errors and enable the development of binocularity in anisometropic, non-strabismic children [12]. The purpose of this study is to evaluate the long-term efficacy of scleral contact lenses in terms of visual outcomes, complications, rates of amblyopia, and compliance in aphakic children after lensectomy. To the best of our knowledge, this is the first study on the use of scleral contact lenses for long-term correction infantile aphakia.
Methods
Participants
This is a retrospective study, approved by the local institutional review board. The files of all children who underwent lensectomy between January 1st, 2004 and December 31st 2018 were retrospectively reviewed. Children with unilateral or bilateral congenital or acquired cataract who underwent lensectomy without primary or secondary IOL implantation and who used scleral contact lenses to correct their visual acuity were included. All eyes included in this study were intentionally left aphakic at the time of the initial surgery.
Excluded from the study were children that did not complete any follow up, follow up of less than 6 months, children with mental retardation who could not use contact lenses and children who were not able to be evaluated using a stationary or portable slit-lamp and were examined only under anaesthesia due to aggressive resistance to examination and not due to a younger age. Cases in which scleral lenses were changed to corneal contact lenses within a period of less than 6 months were also excluded.
Data collection
Data were collected from the medical records from the time of birth and lens pathology diagnosis, surgical reports and the subsequent follow up visits with ophthalmologists, optometrists, and orthoptists. Collected parameters included basic demographics (age, gender, birth history), cataract characteristics (type, family history, age of diagnosis), surgery (technique, complications, examination under anaesthesia), aphakic refraction and visual acuity, scleral lenses fitting (refraction, complications, visual acuity) and the characteristics of the last follow up (visual acuity, rates of strabismus, amblyopia, compliance to occlusions, glaucoma and uveitis). Amblyopia was defined as unilateral or bilateral reduction of BCVA that cannot be attributed to any structural abnormalities of the eye or visual pathways. Severe amblyopia visual acuity 20/125-20/400, moderate 20/100 or better and mild amblyopia 20/40-20/100 (we took into consideration the younger age whose vision not supposed to be 20/20).
Poor compliance with occlusion was decided based on the information provided by the parents, if the occlusion was done less than half the time required by the physician.
Postoperative follow up
Following surgery, frequent follow up examinations were performed: In the ophthalmology department by a specialist in paediatric ophthalmology every 3–6 months and in the private optometric clinic 2 weeks after receiving the lens, and every 3 months thereafter. Compliance to lens wear was calculated according to parental feedback on every visit in the clinic. During the follow up, the paediatric ophthalmologist explained to the patients the options of secondary IOL implantation versus continuation of scleral lens wear. If the patient underwent secondary IOL implantation, their data was collated only up to the time of surgery.
Scleral lens fitting
Postoperative objective retinoscopic refraction was performed on the aphakic eye and a cycloplegic retinoscopy on the fellow phakic eye within 1 week after surgery. The standard routine for aphakic infants in the optometric clinic is to fit a rigid gas permeable contact lens. If the lens continually falls out, or is easily rubbed out of the eye, a scleral lens is fitted. This study included only the cases fitted with scleral lenses. All scleral lenses used in this study were fenestrated, facilitating the ease of insertion and removal by the parents. Their 14.0 mm diameter created stability of the lens, not easily rubbed out by the infant. The optical correction was directed to close nearby focus of approximately 30 cm, being the infants natural near focus distance.
The adjustment of the scleral lenses was re-assured with the use of the Topcon OCT Meistro Spectralis 3D, depending on children’s co-operation.
Additionally, a patching regime was initiated for 2/3 of the child’s waking hours—The patching regimen was recommended to both unilateral and bilateral cases – in unilateral cases, the parents were instructed to patch the phakic eye. In bilateral aphakia- both eyes were patched alternately, with less hours for the deeper amblyopic eye (e.g., the strabismic eye).
The eye was continually monitored for any resultant corneo-scleral pathology, optical changes and development of strabismus and nystagmus.
Outcome measures
The primary outcome measure was the final visual acuity achieved in the aphakic eye. Secondary outcome measures were orthoptic measurements, rate of amblyopia development, compliance and adherence to treatment, adverse effects, and rates of glaucoma and uveitis.
Statistical analysis
Data were expressed as numbers and percentage for qualitative variables and as mean and standard deviation for continuous parameters. Normality distribution was checked for continuous data (Shapiro–Wilk test) and tests were done in accordance: T-test or Mann–Whitney non-parametric test. For nominal variables – Chi-Square test was done.
P < 0.05 was considered statistically significant. All analyses were done with SPSS-25 software (IBM, Armonk, NY, USA).
Results
Demographic characteristics
The study included 50 eyes of 35 patients. Of these, 45 (90%) were eyes with congenital cataract. Other indications for paediatric lens extraction included one (2%) case of traumatic cataract and four (8%) cases of subluxated crystalline lenses. The majority (86%) of children were born in term, and 14% had a pre-term birth (between 34 and 36 weeks). No children with retinopathy of prematurity were included. The mean birth weight was 2942.03 ± 697.5 grams (range 1840–4300 grams) and the median age of diagnosis was 2 months (range 0–59 months). The eyes included were 22 (44%) right eyes and 28 (56%) left eyes. Mean follow up was 66.32 ± 39.5 months (range 6–139 months). These characteristics are detailed in Table 1.
Surgery and lens fitting
The median age at the time of surgery was 2 months (range 1–62 months). Only one child was operated at the age of over 2.5 years, due to a traumatic cataract and was left aphakic because of bag instability.
All children underwent cataract surgery by the same method of anterior capsulorhexis, lensectomy and posterior capsulectomy, in six different ophthalmology departments in Israel. Additional anterior vitrectomy was performed in 34 (76%) eyes.
All scleral lenses were custom made, according to the base curve and dioptrical power required for the specific case (Fig. 1).
Refractive and visual outcomes
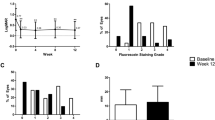
Mean spherical equivalence (SE) was plus 17.43 ± 3.6 Dioptres (D) 1 week after the surgery, and significantly changed to plus 10.01 ± 6.75 D on the last follow up (range −7.00D and + 20.00D, p < 0.0001). Astigmatism was found in twenty-two (44%) eyes, of these 14 (28%) were < 1 D and 8 (16%) eyes were between 1-2D. The size of the astigmatism differed significantly on the last follow up (changing from 0.67 ± 0.9 D to 0.53 ± 0.7 D, p < 0.0001). Final good visual acuity of ≥ 1 LogMAR (i.e., better than 20/200 Snellen) was seen in 76% of cases. Final BCVA of ≥ 0.3 LogMAR (i.e., better than 20/40 Snellen) was achieved in seventeen eyes (34%). Mean BCVA after unilateral surgery was 1 LogMAR (equivalent to 20/200 Snellen) versus 0.4 LogMAR (equivalent to 20/50 Snellen) after bilateral surgery. The rate of amblyopia was 50%. We did not find a significant correlation between the age of diagnosis and the age of surgery to final BCVA (p = 0.342 and p = 0.150, respectively). Surprisingly, while comparing the age at which the children began to wear scleral lenses, we found that those who were started wearing scleral lenses at an older age, had a better final BCVA (p = 0.007, r = −0.402). Strabismus developed in 28 (56%) cases. Children with strabismus had less favourable visual outcomes, as mean final BCVA without strabismus was 0.43 ± 0.4 LogMAR (equivalent to 20/53 Snellen) versus 0.8 ± 0.5 LogMAR (equivalent to 20/126 Snellen) in children with strabismus (p = 0.005) (Fig. 2). Moreover, children who underwent unilateral surgery had less favourable visual outcomes than those who had bilateral surgery, with mean final BCVA after unilateral surgery of 0.99 ± 0.54 LogMAR (equivalent to 20/200 Snellen) versus 0.4 ± 0.29 LogMAR (equivalent to 20/50 Snellen) in eyes after bilateral surgery (p < 0.001) (Fig. 3). Other parameters, such as age at surgery, refraction, cylinder, or age at the last follow up, were not associated with strabismus (P > 0.05 for all). Eye patching was implemented in 30 eyes (60%)− 16 eyes (80%) in cases of a unilateral aphakic eye as compared to 14 eyes of 9 children in cases of bilateral aphakia (Of them, five children had bilateral alternating patching regimen, and four children patched only one eye) (46.7%) (p = 0.022). Poor compliance was recorded in 8 cases (16%) and was not significantly correlated to unilaterality (p = 1.00).
Scleral lens outcomes
During the follow up, no corneal infections were documented. In 19 eyes (38%) adverse effects on the ocular surface were recorded, such as superficial punctate keratopathy (n = 16), peri-limbal pannus (n = 2) and peripheral non-visually significant corneal scars (n = 1). No differences were found between binocular and uniocular scleral contact lens wear (p = 0.65), and there was no correlation between age at the time of surgery, initiation of scleral contact lens use or at the final follow up and final BCVA. Contact lens exchange was required in seventeen eyes (34%), due to scratched lenses (n = 2), chronic irritation and inconvenience (n = 4), loss of the lens (n = 2), exchange to soft contact lenses (n = 2) and broken lenses (n = 4). Except for two cases, the lenses were well-tolerated by the children. Rates of contact lens exchange (due to loss, irrigation or damage) were not significantly different between bilateral and unilateral cases and did not correlate with age (p > 0.05 for all).
Complications and additional surgeries
Intraoperative complications were encountered in 8 (16%) cases, and included vitreous haemorrhage (n = 4), iris damage (n = 2) and anterior chamber haemorrhage (n = 2). Nineteen eyes (38%) required additional surgery for the treatment of postoperative complications, which included visually significant phimosis (n = 6), secondary IOL implantation (n = 3), strabismus (n = 5), tractional retinal detachment (n = 2) (one of them occurred 6 months after secondary IOL implantation), glaucoma requiring surgical intervention (n = 2) and corneal decompensation requiring a keratoplasy (n = 1) (the corneal decompensation was attributed to additional surgeries, and not to the scleral contact lens). Additionally, 4 (8%) eyes underwent Nd:YAG laser posterior capsulotomy during the follow up period.
As mentioned above, the mean follow up was 66.32 ± 39.5 months. The average age at the last follow up was 59.42 ± 38.03 months. During the follow up, only three children underwent secondary IOL implantation. Ten (20%) eyes developed glaucoma – eight were treated medically and two required surgical intervention. Mean intraocular pressure at the last follow up was 17.3 ± 4.07 mmHg (range 12–33 mmHg). One eye (2%) developed uveitis. There was no statistically significant correlation between glaucoma and uveitis development and age at operation, strabismus or binocular surgeries (p > 0.05 for all).
Discussion
Previous studies have reported the efficacy and safety of contact lenses (CL) in correcting infantile aphakia [13, 14]. However, most of the patients enrolled were wearing a soft contact lens. To the best of our knowledge, this is the first study on the use of scleral contact lenses for long-term correction infantile aphakia.
With a mean follow up of 66.32 ± 39.5 months, we found that baseline mean SE changed significantly from + 17.43 ± 3.6 D 1 week after surgery, to + 10.01 ± 6.75 D on the last follow up. Astigmatism was found in twenty-two (44%) eyes, all less than 2D. The size of the astigmatism differed significantly on the last follow up changing from −0.67 ± 0.9 to −0.53 ± 0.7. To emphasise, the change in the amount of astigmatism was calculated from individual cases and is not an expression of the average astigmatism.
This is consistent with two other reports that noted a reduction of astigmatism of −0.26 ± 0.36 D in children during the first year of life [15]. In these studies, the keratometric astigmatism for the contact lens wearing cohort decreased by a mean of 0.36 D in the first year of life [16], and similar to our findings, approximately half (52%) of treated eyes had ≤ 2 D of corneal astigmatism.
In our study, mean final BCVA was 0.65 LogMAR (equivalent to 20/89 Snellen). Seventeen eyes (34%) achieved final BCVA of 0.3 LogMAR (equivalent to 20/40 Snellen) or better. Mean final BCVA in unilateral cataract was 1 LogMAR (equivalent to 20/200 Snellen). In the IATS children were prescribed with silicone elastomer (SE) contact lenses or rigid gas permeable (GP) contact lenses [10]. Our results were not very different from the IATS, over a longer follow up time. In the IATS, the objective median logMAR visual acuity for both contact lens groups was 0.9 (equivalent to 20/160 Snellen). Thirty three percent of patients wearing GP lenses achieved 0.3 LogMAR (equivalent to 20/40 Snellen) or better vision compared to only 20% wearing SE lenses [17]. Our findings are similar to Aurata et al., who found that the mean final visual acuity of the operated eyes in the IOL group was 0.45 LogMAR (equivalent to 20/55 Snellen) compared with 0.6 LogMAR (equivalent to 20/80 Snellen) for the affected eyes in the CL group, with no statistically significant difference found between the groups [8]. We note that both studies did not use scleral contact lenses.
We found that children with a better final BCVA, started wearing scleral contact lens at older age (p = 0.007, r = −0.402). This finding is seemingly inconsistent with the fact that we did not find a significant correlation between the age of diagnosis and the age of surgery to final BCVA. We suggest that children with better visual acuity were less symptomatic, with more slowly progressive cataracts, and therefore were operated at an older age, outside the critical sensitive period. Strabismus developed in 28 (56%) cases. Children with strabismus had significantly less favourable visual outcomes (mean BCVA without strabismus was 0.42 LogMAR (equivalent to 20/53 Snellen) versus 0.8 LogMAR (equivalent to 20/126 Snellen) in children with strabismus). Aurata et al. reported that the incidence of strabismus postoperatively was 55% in the IOL group compared with 83% in the CL group (p = 0.039). The rates of strabismus in our study are similar to the results in IOL implantation group, the incidence of which is much lower than in the contact lens wear group. This shows that wearing scleral contact lenses can promote the development of binocular vision and fusion function in children, just as well as IOL implantation. It is important to note, that it may be inaccurate to state, that eyes with strabismus had worse visual acuity, since eyes with worse acuity that did not develop properly, may develop strabismus.
Our results showed that unilateral surgeries had less favourable visual outcomes than bilateral surgeries. These results are compatible with those reported by Check et al., who found that median postoperative visual acuity in eyes of children with bilateral cataracts was better than the median acuity of children with unilateral cataracts (20/63 vs 20/200) [18]. This finding is consistent with other studies [19,20,21]- Lu et al. showed a mean BCVA of 0.98 ± 0.18, 0.50 ± 0.14 and 0.61 ± 0.25 logMAR for unilateral, bilateral and all eyes, respectively [20]. Moreover, Louison et al. reported a higher median postoperative BCVA in the bilateral cataract group than in the unilateral cataract group, 0.1 logMAR [IQR: 0.0–0.8] vs. 0.5 logMAR [IQR: 0.2–0.8], respectively [21]. A possible reason for worse outcomes in unilateral cataracts may be that amblyopia develops more rapidly in unilateral cataract because of unequal visual deprivation. Moreover, it is possible that patients with bilateral aphakia accept amblyopic treatment more easily.
Except for two cases (4%), the scleral lenses were tolerated well by all the children. Similarly, in the IATS, during 5 years of follow up, only three (5%) patients randomised to contact lens wear underwent the implantation of a secondary IOL. In contrast, Mittelviefhaus et al., found that up to 30% of children had to discontinue contact lens wear [22]. The lower failure rate in our study may be explained by a very strict follow up routine in the clinic, providing efficient solutions and by the fact that the other were not scleral contact lenses.
Infectious keratitis and corneal ulcers, the most serious complication of contact lens wear [23], was not encountered during the follow up in our cohort. In the literature, the incidence of these complications in adults wearing scleral contact lenses is also very low—several case reports describe scleral lens-related keratitis [24,25,26]. Severinsky et al. reviewed outcomes of scleral contact lens wear in 31 patients (36 eyes), and reported two cases of microbial keratitis, which were attributed to patient noncompliance [27]. The results of Russell et al. were less favourable with SE and GP contact lenses: Out of fifty-seven eyes in the study, six eyes had a single incidence of bacterial keratitis (10%).
In this study, over a follow up period of 5.5 ± 3.2 years, ten eyes (20%) developed glaucoma and two eyes required surgical intervention. This rate was comparable to previous reports. The IATS at 5 years, found that a total of 20 children (17%) in the contact lens group were diagnosed with glaucoma or glaucoma suspect vs a total of 16 children (14%) in the IOL group, an insignificant difference [17]. However, it is important to mention that in the IATS, children who were operated younger (under 48 days of age) conferred increased risk of glaucoma (26% versus 9%, respectively), while in our study- we found no correlation between age at surgery and increased risk of glaucoma. We operated nineteen eyes before the age of 48 days, this group developed glaucoma in 15% of cases. Eyes operated older than 48 days (31 eyes), developed glaucoma in 21% of cases (p > 0.05). Magnusson et al. found that a diagnosis of glaucoma was recorded for 12% of the eyes (with a mean follow up time was 9.6 years) [28, 29], similar to Solebo et al., who included children operated before age of two, found that secondary glaucoma was diagnosed in 19 (12%) of 158 children–ten in the conventional treatment and nine in the IOL group (an insignificant difference) [30].
Additional surgery for the treatment of postoperative complications was conducted in nineteen eyes (38%). This percentage correlates with the overall reoperation rate in the study of Aurata et al., which reported a 35% reoperation rate in the CL group compared with 78% in the IOL group (p = 0.027) [8]. In the CL group, the indications for surgery were different from our study, as nineteen patients in the CL group underwent strabismus surgery and three received a secondary IOL.
The most common reason for reoperation in our study was visually significant phimosis (n = 6, 12%). These results are comparable to the IOLunder2 study, which also showed that the most common adverse event was visual axis opacity − 12 [17%] of 70 children in the conventional treatment group. It is interesting to note, that in the IOL group in this study, this adverse event was three times more − 42 [48%] of 88 children [30]. Lower reoperation rate in the contact lens group is an important advantage.
This study has several limitations. First, it is limited due to its size and retrospective nature. However, since the follow up was conducted in the same optometric clinic with only one specialist, the data was very organised. We also note that this is the first, and relatively large series focused on the management of paediatric aphakia with scleral contact lenses, with long-term follow up. Second, we reported broad postoperative outcomes, not only the outcomes associated with the use of a contact lens. Third, our article absence of definitions of key outcomes or associated clinical variables. Fourth, we did not divide the results by the age of the children. Moreover, we note the limitation of not including a control group of children treated by IOL implantation or other forms of optical correction.
In conclusion, our results demonstrate that scleral contact lenses are an effective and safe means of optical correction method for aphakic children after lensectomy, which may be used long-term with good compliance of wear, excellent visual outcomes, and tolerable adverse events. Long-term visual results are comparable to those achieved with IOL implantation and better than those achieved with corneal contact lenses, with likely lower rates of complications and reoperations. Therefore, in cases where delaying the IOL implantation is considered, use of scleral contact lenses is a good option for managing aphakia and preserving the visual potential, for the long term or until the IOL implantation. We recommend the skills required for the fitting of scleral contact lenses and monitoring their use be available to any institution that treats paediatric cataract and aphakic patients.
Summary
What was known before
-
With secondary IOL implantation, refractive correction is managed by contact lenses.
-
Scleral lenses are stable, cost effective and have few or no adverse corneal effects in adults.
What this study adds
-
Scleral contact lenses are an effective and safe means of optical correction method for aphakic children after lensectomy.
-
Scleral contact lenses may be used long-term with good compliance of wear, excellent visual outcomes, and tolerable adverse events.
-
Long-term visual results are comparable to those achieved with IOL implantation and better than those achieved with corneal contact lenses.
References
Ceyhan D, Schnall BM, Breckenridge A, Fontanarosa J, Lehman SS, Calhoun JC. Risk factors for amblyopia in congenital anterior lens opacities. J AAPOS. 2005;9:537–41. https://doi.org/10.1016/j.jaapos.2005.09.001.
Mohammadpour M, Shaabani A, Sahraian A, Momenaei B, Tayebi F, Bayat R, et al. Updates on managements of pediatric cataract. J Curr Ophthalmol. 2018;31:118–26. https://doi.org/10.1016/j.joco.2018.11.005.
Wilson ME,Jr, Trivedi RH, Buckley EG, Granet DB, Lambert SR, Plager DA, et al. ASCRS white paper. Hydrophobic acrylic intraocular lenses in children. J Cataract Refract Surg. 2007;33:1966–73. https://doi.org/10.1016/j.jcrs.2007.06.047.
Birch EE, Cheng C, Stager DR,Jr, Felius J. Visual acuity development after the implantation of unilateral intraocular lenses in infants and young children. J AAPOS. 2005;9:527–32. https://doi.org/10.1016/j.jaapos.2005.07.008.
Plager DA, Lynn MJ, Buckley EG, Wilson ME, Lambert SR.Infant Aphakia Treatment Study Group. Complications, adverse events, and additional intraocular surgery 1 year after cataract surgery in the infant Aphakia Treatment Study. Ophthalmology. 2011;118:2330–4. https://doi.org/10.1016/j.ophtha.2011.06.017.
Plager DA, Yang S, Neely D, Sprunger D, Sondhi N. Complications in the first year following cataract surgery with and without IOL in infants and older children. J AAPOS. 2002;6:9–14. https://doi.org/10.1067/mpa.2002.121169.
Lambert SR, Lynn MJ, DuBois LG, Cotsonis GA, Hartmann EE, Wilson ME, Infant Aphakia Treatment Study G. Axial elongation following cataract surgery during the first year of life in the infant Aphakia Treatment Study. Invest Ophthalmol Vis Sci. 2012;53:7539–45. https://doi.org/10.1167/iovs.12-10285.
Autrata R, Rehurek J, Vodicková K. Visual results after primary intraocular lens implantation or contact lens correction for aphakia in the first year of age. Ophthalmologica. 2005;219:72–79. https://doi.org/10.1159/000083264.
Lambert SR, Lynn M, Drews-Botsch C, DuBois L, Wilson ME, Plager DA, et al. Intraocular lens implantation during infancy: perceptions of parents and the American Association for Pediatric Ophthalmology and Strabismus members. J AAPOS. 2003;7:400–5. https://doi.org/10.1016/j.jaapos.2003.08.004.
Lambert SR, Lynn MJ, Hartmann EE, DuBois L, Drews-Botsch C, Freedman SF.Infant Aphakia Treatment Study Group, et al. Comparison of contact lens and intraocular lens correction of monocular aphakia during infancy: a randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 years. JAMA Ophthalmol. 2014;132:676–82. https://doi.org/10.1001/jamaophthalmol.2014.531.
Lambert SR, Kraker RT, Pineles SL, Hutchinson AK, Wilson LB, Galvin JA, et al. Contact lens correction of aphakia in children: a report by the American academy of ophthalmology. Ophthalmology. 2018;125:1452–8. https://doi.org/10.1016/j.ophtha.2018.03.014.
van der Worp E, Bornman D, Ferreira DL, Faria-Ribeiro M, Garcia-Porta N, González-Meijome JM. Modern scleral contact lenses: A review. Cont Lens Anterior Eye. 2014;37:240–50. https://doi.org/10.1016/j.clae.2014.02.002.
Saltarelli DP. Hyper oxygen-permeable rigid contact lenses as an alternative for the treatment of pediatric aphakia. Eye Contact Lens. 2008;34:84–93. https://doi.org/10.1097/ICL.0b013e31811eadaa.
Chen YC, Hu AC, Rosenbaum A, Spooner S, Weissman BA. Long-term results of early contact lens use in pediatric unilateral aphakia. Eye Contact Lens. 2010;36:19–25. https://doi.org/10.1097/ICL.0b013e3181c6dfdc.
Russell B, Ward MA, Lynn M, Dubois L, Lambert SR.Infant Aphakia Treatment Study Group. The infant aphakia treatment study contact lens experience: one-year outcomes. Eye Contact Lens. 2012;38:234–9. https://doi.org/10.1097/ICL.0b013e3182562dc0.
Mutti DO, Mitchell GL, Jones LA, Friedman NE, Frane SL, Lin WK, et al. Refractive astigmatism and the toricity of ocular components in human infants. Optom Vis Sci. 2004;81:753–61. https://doi.org/10.1097/00006324-200410000-00007.
Russell B, DuBois L, Lynn M, Ward MA, Lambert SR.Infant Aphakia Treatment Study Group. The infant aphakia treatment study contact lens experience to age 5 years. Eye Contact Lens. 2017;43:352–7. https://doi.org/10.1097/ICL.0000000000000291.
Chak M, Wade A, Rahi JS.British Congenital Cataract Interest Group. Long-term visual acuity and its predictors after surgery for congenital cataract: findings of the British congenital cataract study. Invest Ophthalmol Vis Sci. 2006;47:4262–9. https://doi.org/10.1167/iovs.05-1160.
Borisovsky G, Silberberg G, Wygnanski-Jaffe T, Spierer A. Results of congenital cataract surgery with and without intraocular lens implantation in infants and children. Graefes Arch Clin Exp Ophthalmol. 2013;251:2205–11. https://doi.org/10.1007/s00417-013-2327-2.
Lu Y, Ji YH, Luo Y, Jiang YX, Wang M, Chen X. Visual results and complications of primary intraocular lens implantation in infants aged 6 to 12 months. Graefes Arch Clin Exp Ophthalmol. 2010;248:681–6. https://doi.org/10.1007/s00417-010-1310-4.
Louison S, Blanc J, Pallot C, Alassane S, Praudel A, Bron AM, et al. Visual outcomes and complications of congenital cataract surgery. J Fr Ophtalmol. 2019;42:368–74. https://doi.org/10.1016/j.jfo.2018.10.007.
Mittelviefhaus H, Mittelviefhaus K, Gerling J. Ursachen des Kontaktlinsen-Abbruchs bei kindlichen Aphakien. Indikation für Intraokularlinsen? [Etiology of contact lens failure in pediatric aphakia. Indications for intraocular lenses?]. Ophthalmologe. 1998;95:207–12. https://doi.org/10.1007/s003470050263.
Schornack M. “Adverse events associated with scleral lens wear”. J Contact lens Res Sci. 2018;2.SP 1:e13–e17.
Zimmerman AB, Marks A. Microbial keratitis secondary to unintended poor compliance with scleral gas-permeable contact lenses. Eye Contact Lens. 2014;40:e1–e4. https://doi.org/10.1097/ICL.0b013e318273420f.
Fernandes M, Sharma S. Polymicrobial and microsporidial keratitis in a patient using Boston scleral contact lens for Sjogren’s syndrome and ocular cicatricial pemphigoid. Cont Lens Anterior Eye. 2013;36:95–97. https://doi.org/10.1016/j.clae.2012.10.082.
Bruce AS, Nguyen LM. Acute red eye (non-ulcerative keratitis) associated with mini-scleral contact lens wear for keratoconus. Clin Exp Optom. 2013;96:245–8. https://doi.org/10.1111/cxo.12033.
Severinsky B, Behrman S, Frucht-Pery J, Solomon A. Scleral contact lenses for visual rehabilitation after penetrating keratoplasty: long term outcomes. Cont Lens Anterior Eye. 2014;37:196–202. https://doi.org/10.1016/j.clae.2013.11.001.
Vishwanath M, Cheong-Leen R, Taylor D, Russell-Eggitt I, Rahi J. Is early surgery for congenital cataract a risk factor for glaucoma?. Br J Ophthalmol. 2004;88:905–10. https://doi.org/10.1136/bjo.2003.040378.
Magnusson G, Abrahamsson M, Sjöstrand J. Glaucoma following congenital cataract surgery: an 18-year longitudinal follow-up. Acta Ophthalmol Scand. 2000;78:65–70. https://doi.org/10.1034/j.1600-0420.2000.078001065.x.
Solebo AL, Cumberland P, Rahi JS.British Isles Congenital Cataract Interest Group. 5-year outcomes after primary intraocular lens implantation in children aged 2 years or younger with congenital or infantile cataract: findings from the IoLunder2 prospective inception cohort study. Lancet Child Adolesc Health. 2018;2:863–71. https://doi.org/10.1016/S2352-4642(18)30317-1.
Acknowledgements
The abstract of the article has not been presented previously. None of the authors have any proprietary interest in this study. No funds or grants were received for this study. The authors have declared that no competing interests exist. None of the authors has a potential source of conflict of interest - financial or otherwise that might be perceived as influencing an author’s objectivity. VY was responsible for designing the review protocol, writing the protocol and report, conducting the search, screening potentially eligible studies, extracting and analysing data, interpreting results, updating reference lists. IH was responsible for designing the review protocol, the orthoptist who fitted and prescribed the scleral contact lenses, was interpreting results and contributed to writing the report. EM contributed to the design of the review protocol, helped in writing the report, EIA was the surgeon of most of the paediatric patients and provided feedback on the report, IC was extracting and analysing data and interpreting results. NED contributed to designing the review protocol, was the main paediatric ophthalmologist doing a follow up on the patients and provided feedback on the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yehezkeli, V., Hare, I., Moisseiev, E. et al. Assessment of long-term visual outcomes in aphakic children wearing scleral contact lenses. Eye 37, 421–426 (2023). https://doi.org/10.1038/s41433-022-01942-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-01942-6