Abstract
Purpose
To assess the clinical significance of suspended scattering particles in motion (SSPiM) and different cystic phenotypes in diabetic macular oedema (DME) treated with dexamethasone implant (DEX-i).
Methods
A retrospective review of type 2 diabetic patients with DME treated with a DEX-i was conducted. Swept-source optical coherence tomography angiography (OCTA, PLEX Elite 9000) with a 3-mm volume cube was performed. Regions of interest were delineated with Fiji software (version 2.1.0/1.53.c) in the superficial vascular complex (SVC) and deep capillary plexus (DCP) at baseline, 2- and 4-months after DEX-i. SSPiM was defined as regions of variable reflectivity with a decorrelation signal. Without a detectable decorrelation signal, its counterpart was addressed as ‘corpuscular,’ while hyporeflective cysts were optical empty without hyperreflective material enclosed.
Results
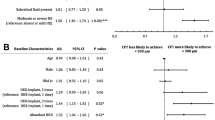
After treatment, the hyporeflective component demonstrated substantial reabsorption in the SVC (–95.4% at 2- and –84.4% at 4-months, p < 0.01 both) and DVC (–84.4%, 2-months), with a less critical decrease of the corpuscular component in the SVC (2-months: –41.9%, p = 0.001 and 4 months: –1.8%, p = 0.73), and not significant in the DVC. SSPiM did not significantly change in the SVC and DVC neither at 2- and 4-months (p > 0.05, all).
Conclusions
After a single DEX-i, the clearance of different cystic phenotypes proceeds with resorption of hyporeflective, followed by corpuscular components. SSPiM demonstrated minimal response, indicating a severe BRB breakdown that may require repeated treatment to reach a satisfactory anatomical response.
Similar content being viewed by others
Suspended scattering particles in motion (SSPiM) describe a decorrelation signal caused by Brownian motion of particles within intraretinal fluid pockets on optical coherence tomography angiography (OCTA), likely lipoprotein particles suspended in a liquid compartment [1]. Since not all the cysts in diabetic macular oedema (DME) present a decorrelation signal, presumably other factors such as concentration, composition, or flow velocity may contribute to the generation of this OCTA signal [2]. In this regard, we hypothesized that different cystic phenotypes might represent various degrees of retinal–blood-barrier (BRB) breakdown. The present work aimed to assess the clinical and prognostic value of SSPiM in DME eyes treated with intravitreal dexamethasone (DEX-i). Further, to understand the relationship between different cystic phenotypes and the clinical response to treatment.
A retrospective review of 18 type 2 diabetic patients (18 eyes) with DME treated with a single DEX-i was conducted. Swept-source OCTA (PLEX Elite 9000) with a 3-mm volume cube was analysed. Regions of interest were delineated with Fiji software (version 2.1.0/1.53.c) in the superficial vascular complex (SVC) and deep capillary plexus (DCP) at baseline, 2- and 4 months after DEX-I (Fig. 1). SSPiM was defined as cystic regions of variable reflectivity with a decorrelation signal. Without a detectable decorrelation signal, its counterpart was addressed as “corpuscular,” while hyporeflective cysts were optical empty without hyperreflective material enclosed (Fig. 2) [3].
A En-face OCTA and structural OCTA (B) of the superficial vascular complex (SVC), the light blue line represents the corresponding B-scan visible at (C). En-face (D) and structural OCTA (E) of the deep capillary plexus (DCP) with the corresponding B scan (F). The presence of SSPiM on both SVC (G) and DCP (H) was confirmed using each b scan with flow overlaid as reference. The automatic segmentation used for the SVC is represented through the dotted purple lines. If any discontinuation or irregularities was noted, the boundaries were manually traced by a single experienced operator (S.F.).
A Structural en-face OCTA helps track cystic areas within the central 3 × 3 mm volume. Their contents can be discerned using a B-scan with flow overlaid. Hyporeflective cysts (pale pink arrows and circles) appear with a hyporeflective interior, without evidence of flow signal nor hyperreflective material. Corpuscolate cysts (a white dotted circle and arrows) are characterized by various degrees of hyperreflective material without a flow signal. En-face angio OCTA (B) demonstrating the presence of a reflective area corresponding to suspended scattering in motion (SSPiM) at the corresponding OCTA b-scan (C).
Overall, SSPiM was detectable in 12/18 eyes (66.7%), with a pyramidal distribution from avascular (16.7%) alone, avascular combined with DVC (83.3%) reaching the SVC in 50%. Of note, SSPiM was associated with older age (+4.3 years, p = 0.03) and a history of previous intravitreal treatment (75% of cases, r = 0.53, p = 0.02).
Qualitative and quantitative evaluation of the different cystic area demonstrated substantial reabsorption of the hyporeflective component in the SVC (−95.4% at 2- and −84.4% at 4 months, p = 0.001) and DVC (−84.4% at 2 months), with a less critical decrease of the corpuscular component in the SVC (−41.9% 2 months, p = 0.001 and −1.8% at 4 months, p = 0.73), and not significant in the DVC. SSPiM did not significantly change in both the SVC and DVC at 2- and 4 months (p > 0.05, all).
The topographic distribution of SSPiM showed a pyramidal organization from the outer towards the inner retinal layers. This peculiar distribution has been hypothesized to follow the anatomical location of DME as a result of a diffuse exudation [1], or the extravasated lipoproteinaceous material denser than fluid may sink toward the outer retinal layers [4].
The association of SSPiM with older age may indicate an easier BRB rupture for a physiologic aging process. Moreover, SSPiM was greater in eyes with previous intravitreal treatment, indicating that the fluid resorption is not counteracted by a macromolecules clearance due to a significant BRB damage, leading to further accumulation of this material unable to be removed [1, 5]. After a single DEX-I, the hyporeflective fluid exhibited the greatest response, followed by the corpuscular component, proceeding from the innermost retinal layers. SSPiM persisted despite treatment, representing a factor of a severe BRB breakdown that may require repeated treatments to reach a satisfactory anatomical response.
References
Kashani AH, Green KM, Kwon J, Chu Z, Zhang Q, Wang RK, et al. Suspended scattering particles in motion: a novel feature of OCT angiography in exudative maculopathies. Ophthalmol Retina. 2018;2:694–702.
Ahn J, Han S, Ahn SM, Kim SW, Oh J. Clinical implications of suspended scattering particles in motion observed by optical coherence tomography angiography. Sci Rep. 2020;10:15.
Parravano M, Costanzo E, Borrelli E, Sacconi R, Virgili G, Sadda SR, et al. Appearance of cysts and capillary non perfusion areas in diabetic macular edema using two different OCTA devices. Sci Rep. 2020;10:800.
Choi KE, Han S, Yun C, Kim SW, Oh J. Suspended scattering particles in motion using OCT angiography in branch retinal vein occlusion disease cases with cystoid macular edema. Sci Rep. 2020;10:14011.
Kashani AH, Cheung AY, Robinson J, Williams GA. Longitudinal optical density analysis of subretinal fluid after surgical repair of rhegmatogenous retinal detachment. Retina. 2015;35:149–56.
Acknowledgements
The research for this paper was financially supported by the Italian Ministry of Health and Fondazione Roma. The authors gratefully acknowledge Puma Foundation for its support. The funders had no role in study design, data collection, analysis, decision to publish, or paper preparation.
Author information
Authors and Affiliations
Contributions
MP and SF were responsible for designing and writing the study; EC, DDG and PV conducted the retrospective search, verified the eligibility, and extracting data; DG and SR analysed the data and interpreted the results; GQ reviewed critically and provided writing support of the final draft.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests regarding the publication of this study. MP reports personal fees from Allergan, Novartis, Bayer, Zeiss, Omikron, Alfaintes, Sifi outside the submitted work. PV, EC, DG, SF, DDG has nothing to disclose. SR reported personal fees from: Novartis, Bayer, Zeiss outside the submitted work. GQ: Alimera Sciences, Inc.: Consultant/Advisor; Allegro: Advisor; Allergan: Consultant/Advisor; Apellis: Consultant/Advisor; Baush & Lomb: Consultant; Bayer Healthcare Pharmaceuticals: Consultant/Advisor; Boehringer Ingelheim: Advisor; CenterVue: Consultant/Advisor; Heidelberg Engineering: Consultant/Advisor; Lumithera: Advisor; Nevacar: Advisor; Novartis Pharmaceuticals Corporation: Consultant/Advisor; Roche: Consultant/Advisor. SIFI: Advisor/Consultant; Sooft/Fidia: Consultant; Topcon: Consultant; Thea: Consultant; Zeiss: Consultant/Advisor.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parravano, M., Fragiotta, S., Costanzo, E. et al. Differences in cysts characteristics and related influence on the anatomical response after dexamethasone implant in diabetic macular oedema. Eye 36, 1329–1331 (2022). https://doi.org/10.1038/s41433-021-01857-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01857-8